Genital Transplants: Is Science Going Too Far, Too Fast?

Medical staff rushing organs to a surgery for transplantation.
Thanks to the remarkable evolution of organ transplantation, it's now possible to replace genitals that don't work properly or have been injured. Surgeons have been transplanting ovarian tissue for more than a decade, and they're now successfully transplanting penises and wombs too.
Rules and regulations aren't keeping up with the rapid rise of genital transplants.
Earlier this year, an American soldier whose genitals were injured by a bomb in Afghanistan received the first-ever transplant of a penis and scrotum at Johns Hopkins Medicine.
Rules and regulations aren't keeping up with the rapid rise of genital transplants, however, and there's no consensus about how society should handle a long list of difficult and delicate questions.
Are these expensive transplants worth the risk when other alternatives exist? Should men, famously obsessed with their penises, be able to ask for a better model simply because they want one? And what happens when transplant technology further muddles the concept of biological parenthood?
"We need to remember that the human body is not a machine with interchangeable parts," says bioethicist Craig M. Klugman of DePaul University. "These are complicated, difficult and potentially dangerous surgeries. And they require deep consideration on a physical, psychological, spiritual, and financial level."
From Extra Testicles to Replacement Penises
Tinkering with human genitalia -- especially the male variety -- is hardly a new phenomenon. A French surgeon created artificial penises for injured soldiers in the 16th century. And a bizarre implant craze swept the U.S. in the 1930s when a quack physician convinced men that, quite literally, the more testicles the merrier – and if the human variety wasn't available, then ones from goats would have to do.
Now we're more sophisticated. Modern genital transplants are designed to do two things: Treat infertility (in women) and restore the appearance and function of genitals (in men).
In women, surgeons have successfully transplanted ovarian tissue from one woman to another since the mid-2000s, when an Alabama woman gave birth after getting a transplant from her identical twin sister. Last year, for the first time in the U.S., a young woman gave birth after getting a uterus transplant from a living donor.
"Where do you draw the line? Is pregnancy a privilege? Is it a right?"
As for men, surgeons in the U.S. and South Africa have successfully transplanted penises from dead men into four men whose genitals were injured by a botched circumcision, penile cancer or a wartime injury. One man reportedly fathered a child after the procedure.
The Johns Hopkins procedure was the first to include a scrotum. Testicles, however, were not transplanted due to ethical concerns. Surgeons have successfully transplanted testicles from man-to-man in the past, but this procedure isn't performed because the testes would produce sperm with the donor's DNA. As a result, the recipient could father a baby who is genetically related to the donor.
Are Transplants Worth the Expense and Risk?
Genital transplants are not simple procedures. They're extremely expensive, with a uterus transplant estimated to cost as much as $250,000. They're dangerous, since patients typically must take powerful drugs to keep their immune systems from rejecting their new organs. And they're not medically necessary. All have alternatives that are much less risky and costly.
Dr. Hiten D. Patel, a urologist at Johns Hopkins University, believes these types of factors make penis transplants unnecessary. As he wrote in a 2018 commentary in the journal European Urology, "What in the world are we doing?"
There are similar questions about female genital transplants, which allow infertile women to become pregnant instead of turning to alternatives like adoption or surrogacy. "This is not a life-saving transplant. A woman can very well live without a uterus," says McGill University's Dr. Jacques Balayla, who studies uterine transplantation. "Where do you draw the line? Is pregnancy a privilege? Is it a right? You don't want to cause harm to an individual unless there's an absolute need for the procedure."
But Johns Hopkins urologist Dr. Arthur L. Burnett II, who served on the surgical team that performed the penis-and-scrotum procedure, says penis transplants can be appropriate when other alternatives – like a "neophallus" created from forearm skin and tissue – aren't feasible.
It's also important to "restore normalcy," he says. "We want someone to be able to have sense of male adequacy and a normal sense of bodily well-being on both physical and psychological levels."

Surgical team members who performed the penis transplant, including W. P. Andrew Lee, director of the department of plastic and reconstructive surgery, center.
As for the anonymous recipient, he's reportedly doing "very well" five months after the transplant. An update on Johns Hopkins' website states that "he has normal urinary functions and is beginning to regain sensation in the transplanted tissues."
When the Organ Donors Do It Live
Some peculiar messages reached Burnett's desk after his institution announced it would begin performing penis transplants. Several men wanted to donate their own organs. But for now, transplanted penises are only coming from dead donors whose next of kin have approved the donation.
Burnett doesn't expect live donors to enter the penis transplant picture. But there are no guidelines or policies to stop surgeons from transplanting a penis from a live donor or, for that matter, a testicle.
Live women have already donated wombs and ovarian tissue, forcing them to face their own risks from transplant surgery. "You're putting the donor at risk because she has to undergo pretty expensive surgery for a procedure that is not technically lifesaving," McGill University's Balayla says.
When it comes to uterus transplants, the risk spreads even beyond donor and recipient. Balayla notes there's a third person in the equation: The fetus. "Immunosuppressant medication may harm the baby, and you're feeding the baby with a [uterine] blood vessel that's not natural, held together by stitches," he says.
It's up to each medical institution that performs the procedures to set its own policies.
Bioethicists are talking about other issues raised by genital transplants: How should operations for transgender people fit in? Should men be able to get penis transplants for purely cosmetic reasons? And then there's the looming question of genetic parenthood.
It's up to each medical institution that performs the procedures to set its own policies.
Let's say a woman gets a transplant of ovarian tissue, a man gets a testicle transplant, and they have a baby the old-fashioned way.* The child would be genetically linked to the donors, not the parents who conceived him or her.
Call this a full-employment act not just for bioethicists but theologians too. "Catholicism is generally against reproductive technologies because it removes God from the nature of the procreative act. This technology, though, could result in conception through the natural act. Would their concern remain?" DePaul University's Klugman asked. "Judaism is concerned with knowing a child's parentage, would a child from transplanted testes be the child of the donor or the recipient? Would an act of coitus with a transplanted penis be adultery?"
Yikes. Maybe it's time for the medical field or the law to step in to determine what genital transplants surgeons can and can't -- or shouldn't -- do.
So far, however, only uterus transplants have guidelines in place. Otherwise, it's up to each medical institution that performs the procedures to set its own policies.
"I don't know if the medical establishment is in the position to do the best job of self-regulation," says Lisa Campo-Engelstein, a bioethicist with Albany Medical College. "Reproductive medicine in this country is a huge for-profit industry. There's a possibility of exploitation if we leave this to for-profit fertility companies."
And, as bioethicist Klugman notes, guidelines "aren't laws, and people can and do violate them with no effect."
He doesn't think laws are the solution to the ethical issues raised by genital transplants either. Still, he says, "we do need a national conversation on these topics to help provide guidance for doctors and patients."
[Correction: The following sentence has been updated: "Let's say a woman gets a transplant of ovarian tissue, a man gets a testicle transplant, and they have a baby the old-fashioned way." The original sentence mistakenly read "uterus transplant" instead of "ovarian tissue."]
Dr. May Edward Chinn, Kizzmekia Corbett, PhD., and Alice Ball, among others, have been behind some of the most important scientific work of the last century.
If you look back on the last century of scientific achievements, you might notice that most of the scientists we celebrate are overwhelmingly white, while scientists of color take a backseat. Since the Nobel Prize was introduced in 1901, for example, no black scientists have landed this prestigious award.
The work of black women scientists has gone unrecognized in particular. Their work uncredited and often stolen, black women have nevertheless contributed to some of the most important advancements of the last 100 years, from the polio vaccine to GPS.
Here are five black women who have changed science forever.
Dr. May Edward Chinn
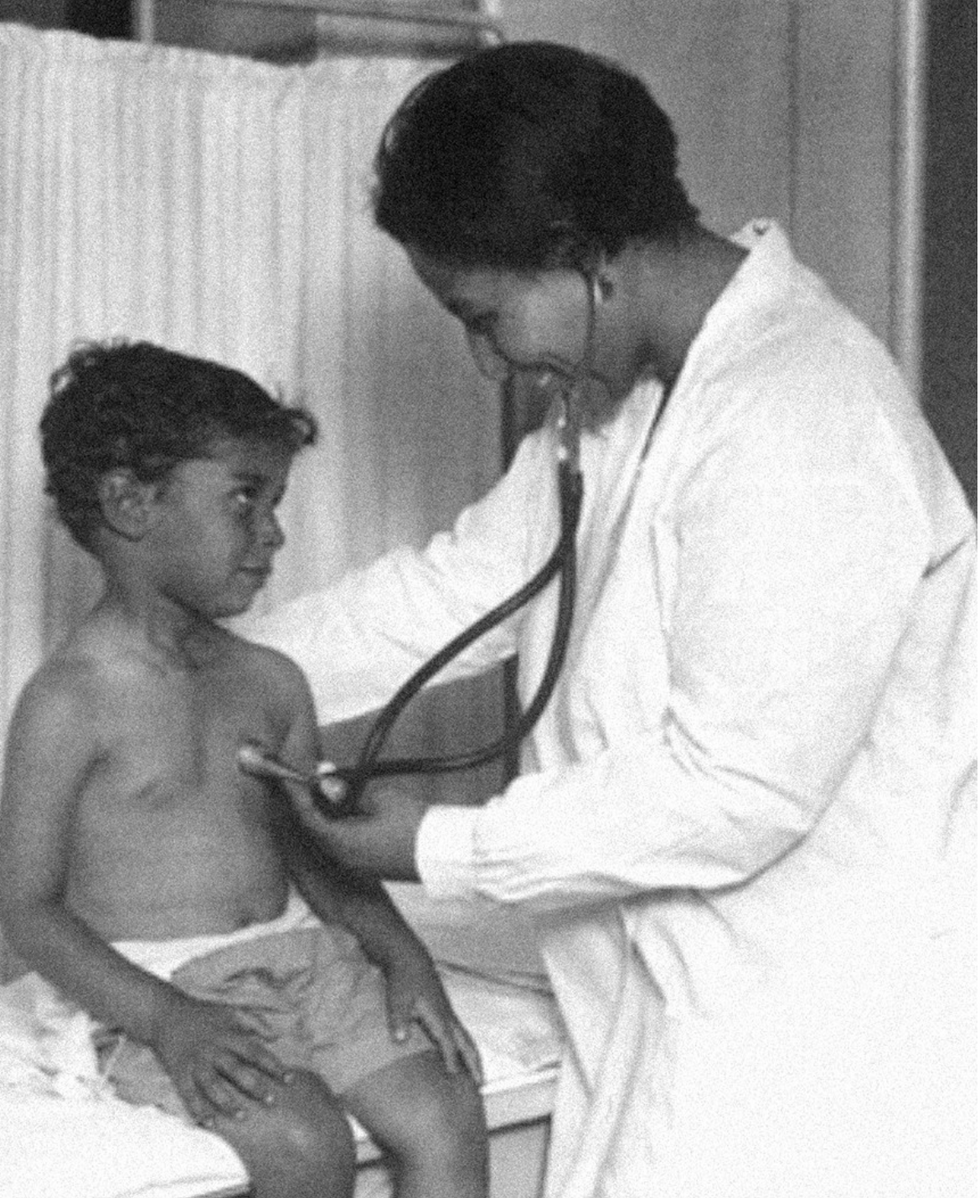
Dr. May Edward Chinn practicing medicine in Harlem
George B. Davis, PhD.
Chinn was born to poor parents in New York City just before the start of the 20th century. Although she showed great promise as a pianist, playing with the legendary musician Paul Robeson throughout the 1920s, she decided to study medicine instead. Chinn, like other black doctors of the time, were barred from studying or practicing in New York hospitals. So Chinn formed a private practice and made house calls, sometimes operating in patients’ living rooms, using an ironing board as a makeshift operating table.
Chinn worked among the city’s poor, and in doing this, started to notice her patients had late-stage cancers that often had gone undetected or untreated for years. To learn more about cancer and its prevention, Chinn begged information off white doctors who were willing to share with her, and even accompanied her patients to other clinic appointments in the city, claiming to be the family physician. Chinn took this information and integrated it into her own practice, creating guidelines for early cancer detection that were revolutionary at the time—for instance, checking patient health histories, checking family histories, performing routine pap smears, and screening patients for cancer even before they showed symptoms. For years, Chinn was the only black female doctor working in Harlem, and she continued to work closely with the poor and advocate for early cancer screenings until she retired at age 81.
Alice Ball

Pictorial Press Ltd/Alamy
Alice Ball was a chemist best known for her groundbreaking work on the development of the “Ball Method,” the first successful treatment for those suffering from leprosy during the early 20th century.
In 1916, while she was an undergraduate student at the University of Hawaii, Ball studied the effects of Chaulmoogra oil in treating leprosy. This oil was a well-established therapy in Asian countries, but it had such a foul taste and led to such unpleasant side effects that many patients refused to take it.
So Ball developed a method to isolate and extract the active compounds from Chaulmoogra oil to create an injectable medicine. This marked a significant breakthrough in leprosy treatment and became the standard of care for several decades afterward.
Unfortunately, Ball died before she could publish her results, and credit for this discovery was given to another scientist. One of her colleagues, however, was able to properly credit her in a publication in 1922.
Henrietta Lacks

onathan Newton/The Washington Post/Getty
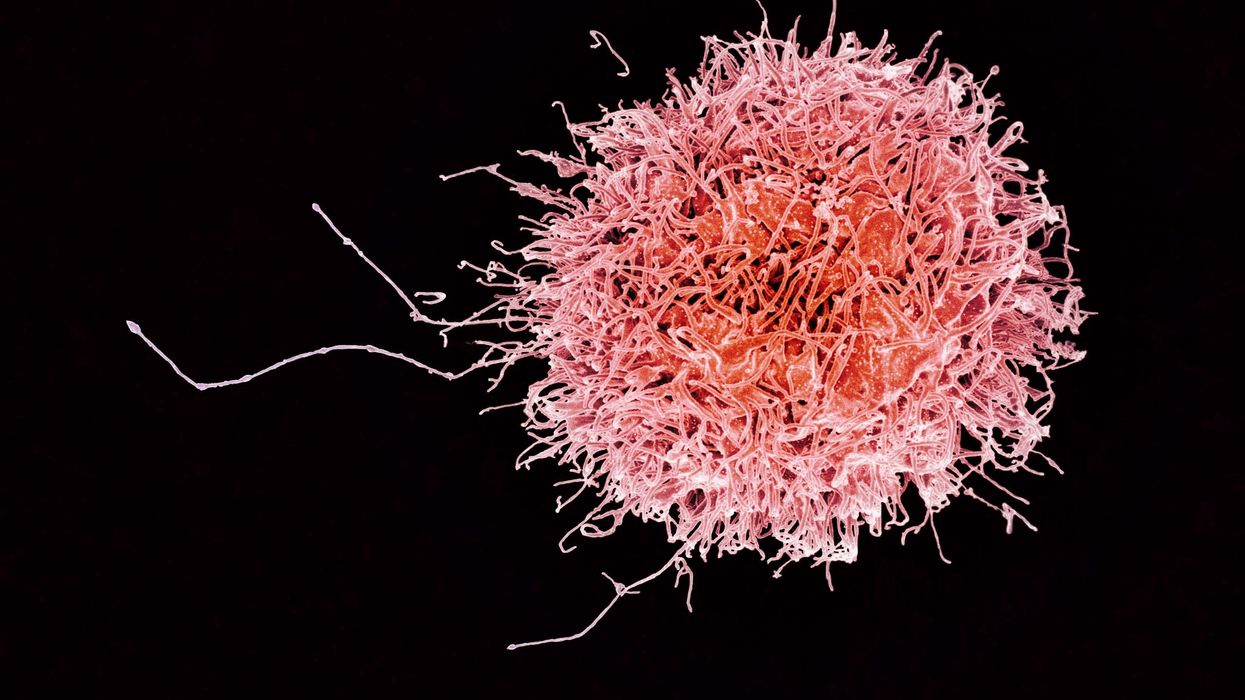
The person who arguably contributed the most to scientific research in the last century, surprisingly, wasn’t even a scientist. Henrietta Lacks was a tobacco farmer and mother of five children who lived in Maryland during the 1940s. In 1951, Lacks visited Johns Hopkins Hospital where doctors found a cancerous tumor on her cervix. Before treating the tumor, the doctor who examined Lacks clipped two small samples of tissue from Lacks’ cervix without her knowledge or consent—something unthinkable today thanks to informed consent practices, but commonplace back then.
As Lacks underwent treatment for her cancer, her tissue samples made their way to the desk of George Otto Gey, a cancer researcher at Johns Hopkins. He noticed that unlike the other cell cultures that came into his lab, Lacks’ cells grew and multiplied instead of dying out. Lacks’ cells were “immortal,” meaning that because of a genetic defect, they were able to reproduce indefinitely as long as certain conditions were kept stable inside the lab.
Gey started shipping Lacks’ cells to other researchers across the globe, and scientists were thrilled to have an unlimited amount of sturdy human cells with which to experiment. Long after Lacks died of cervical cancer in 1951, her cells continued to multiply and scientists continued to use them to develop cancer treatments, to learn more about HIV/AIDS, to pioneer fertility treatments like in vitro fertilization, and to develop the polio vaccine. To this day, Lacks’ cells have saved an estimated 10 million lives, and her family is beginning to get the compensation and recognition that Henrietta deserved.
Dr. Gladys West

Andre West
Gladys West was a mathematician who helped invent something nearly everyone uses today. West started her career in the 1950s at the Naval Surface Warfare Center Dahlgren Division in Virginia, and took data from satellites to create a mathematical model of the Earth’s shape and gravitational field. This important work would lay the groundwork for the technology that would later become the Global Positioning System, or GPS. West’s work was not widely recognized until she was honored by the US Air Force in 2018.
Dr. Kizzmekia "Kizzy" Corbett

TIME Magazine
At just 35 years old, immunologist Kizzmekia “Kizzy” Corbett has already made history. A viral immunologist by training, Corbett studied coronaviruses at the National Institutes of Health (NIH) and researched possible vaccines for coronaviruses such as SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome).
At the start of the COVID pandemic, Corbett and her team at the NIH partnered with pharmaceutical giant Moderna to develop an mRNA-based vaccine against the virus. Corbett’s previous work with mRNA and coronaviruses was vital in developing the vaccine, which became one of the first to be authorized for emergency use in the United States. The vaccine, along with others, is responsible for saving an estimated 14 million lives.On today’s episode of Making Sense of Science, I’m honored to be joined by Dr. Paul Song, a physician, oncologist, progressive activist and biotech chief medical officer. Through his company, NKGen Biotech, Dr. Song is leveraging the power of patients’ own immune systems by supercharging the body’s natural killer cells to make new treatments for Alzheimer’s and cancer.
Whereas other treatments for Alzheimer’s focus directly on reducing the build-up of proteins in the brain such as amyloid and tau in patients will mild cognitive impairment, NKGen is seeking to help patients that much of the rest of the medical community has written off as hopeless cases, those with late stage Alzheimer’s. And in small studies, NKGen has shown remarkable results, even improvement in the symptoms of people with these very progressed forms of Alzheimer’s, above and beyond slowing down the disease.
In the realm of cancer, Dr. Song is similarly setting his sights on another group of patients for whom treatment options are few and far between: people with solid tumors. Whereas some gradual progress has been made in treating blood cancers such as certain leukemias in past few decades, solid tumors have been even more of a challenge. But Dr. Song’s approach of using natural killer cells to treat solid tumors is promising. You may have heard of CAR-T, which uses genetic engineering to introduce cells into the body that have a particular function to help treat a disease. NKGen focuses on other means to enhance the 40 plus receptors of natural killer cells, making them more receptive and sensitive to picking out cancer cells.
Paul Y. Song, MD is currently CEO and Vice Chairman of NKGen Biotech. Dr. Song’s last clinical role was Asst. Professor at the Samuel Oschin Cancer Center at Cedars Sinai Medical Center.
Dr. Song served as the very first visiting fellow on healthcare policy in the California Department of Insurance in 2013. He is currently on the advisory board of the Pritzker School of Molecular Engineering at the University of Chicago and a board member of Mercy Corps, The Center for Health and Democracy, and Gideon’s Promise.
Dr. Song graduated with honors from the University of Chicago and received his MD from George Washington University. He completed his residency in radiation oncology at the University of Chicago where he served as Chief Resident and did a brachytherapy fellowship at the Institute Gustave Roussy in Villejuif, France. He was also awarded an ASTRO research fellowship in 1995 for his research in radiation inducible gene therapy.
With Dr. Song’s leadership, NKGen Biotech’s work on natural killer cells represents cutting-edge science leading to key findings and important pieces of the puzzle for treating two of humanity’s most intractable diseases.
Show links
- Paul Song LinkedIn
- NKGen Biotech on Twitter - @NKGenBiotech
- NKGen Website: https://nkgenbiotech.com/
- NKGen appoints Paul Song
- Patient Story: https://pix11.com/news/local-news/long-island/promising-new-treatment-for-advanced-alzheimers-patients/
- FDA Clearance: https://nkgenbiotech.com/nkgen-biotech-receives-ind-clearance-from-fda-for-snk02-allogeneic-natural-killer-cell-therapy-for-solid-tumors/Q3 earnings data: https://www.nasdaq.com/press-release/nkgen-biotech-inc.-reports-third-quarter-2023-financial-results-and-business