Breakthrough in Creating Fuel from Sunlight Puts Us Closer to Carbon-Neutral Energy

Recent leaps in technology represent an important step forward in unlocking artificial photosynthesis.
Since the beginning of life on Earth, plants have been naturally converting sunlight into energy. This photosynthesis process that's effortless for them has been anything but for scientists who have been trying to achieve artificial photosynthesis for the last half a century with the goal of creating a carbon-neutral fuel. Such a fuel could be a gamechanger — rather than putting CO2 back into the atmosphere like traditional fuels do, it would take CO2 out of the atmosphere and convert it into usable energy.
If given the option between a carbon-neutral fuel at the gas station and a fuel that produces carbon dioxide in spades -- and if costs and effectiveness were equal --who wouldn't choose the one best for the planet? That's the endgame scientists are after. A consumer switch to clean fuel could have a huge impact on our global CO2 emissions.
Up until this point, the methods used to make liquid fuel from atmospheric CO2 have been expensive, not efficient enough to really get off the ground, and often resulted in unwanted byproducts. But now, a new technology may be the key to unlocking the full potential of artificial photosynthesis. At the very least, it's a step forward and could help make a dent in atmospheric CO2 reduction.
"It's an important breakthrough in artificial photosynthesis," says Qian Wang, a researcher in the Department of Chemistry at Cambridge University and lead author on a recent study published in Nature about an innovation she calls "photosheets."
The latest version of the artificial leaf directly produces liquid fuel, which is easier to transport and use commercially.
These photosheets convert CO2, sunlight, and water into a carbon-neutral liquid fuel called formic acid without the aid of electricity. They're made of semiconductor powders that absorb sunlight. When in the presence of water and CO2, the electrons in the powders become excited and join with the CO2 and protons from the water molecules, reducing the CO2 in the process. The chemical reaction results in the production of formic acid, which can be used directly or converted to hydrogen, another clean energy fuel.
In the past, it's been difficult to reduce CO2 without creating a lot of unwanted byproducts. According to Wang, this new conversion process achieves the reduction and fuel creation with almost no byproducts.
The Cambridge team's new technology is a first and certainly momentous, but they're far from the only team to have produced fuel from CO2 using some form of artificial photosynthesis. More and more scientists are aiming to perfect the method in hopes of producing a truly sustainable, photosynthetic fuel capable of lowering carbon emissions.
Thanks to advancements in nanoscience, which has led to better control of materials, more successes are emerging. A team at the University of Illinois at Urbana-Champaign, for example, used gold nanoparticles as the photocatalysts in their process.
"My group demonstrated that you could actually use gold nanoparticles both as a light absorber and a catalyst in the process of converting carbon dioxide to hydrocarbons such as methane, ethane and propane fuels," says professor Prashant Jain, co-author of the study. Not only are gold nanoparticles great at absorbing light, they don't degrade as quickly as other metals, which makes them more sustainable.
That said, Jain's team, like every other research team working on artificial photosynthesis including the Cambridge team, is grappling with efficiency issues. Jain says that all parts of the process need to be optimized so the reaction can happen as quickly as possible.
"You can't just improve one [aspect], because that can lead to a decrease in performance in some other aspects," Jain explains.
The Cambridge team is currently experimenting with a range of catalysts to improve their device's stability and efficiency. Virgil Andrei, who is working on an artificial leaf design that was developed at Cambridge in 2019, was recently able to improve the performance and selectivity of the device. Now the leaf's solar-to-CO2 energy conversion efficiency is 0.2%, twice its previous efficiency.
The latest version also directly produces liquid fuel, which is easier to transport and use commercially.
In determining a method of fuel production's efficiency, one must consider how sustainable it is at every stage. That involves calculating whenever excess energy is needed to complete a step. According to Jain, in order to use CO2 for fuel production, you have to condense the CO2, which takes energy. And on the fuel production side, once the chemical reaction has created your byproducts, they need to be separated, which also takes energy.
To be truly sustainable, each part of the conversion system also needs to be durable. If parts need to be replaced often, or regularly maintained, that counts against it. Then you have to account for the system's reuse cycle. If you extract CO2 from the environment and convert it into fuel that's then put into a fuel cell, it's going to release CO2 at the other end. In order to create a fully green, carbon-neutral fuel source, that same amount of CO2 needs to be trapped and reintroduced back into the fuel conversion system.
"The cycle continues, and at each point, you will see a loss in efficiency, and depending on how much you [may also] see a loss in yield," says Jain. "And depending on what those efficiencies are at each one of those points will determine whether or not this process can be sustainable."
The science is at least a decade away from offering a competitive sustainable fuel option at scale. Streamlining a process to mimic what plants have perfected over billions of years is no small feat, but an ever-growing community of researchers using rapidly advancing technology is driving progress forward.
Scientists have known about and studied heart rate variability, or HRV, for a long time and, in recent years, monitors have come to market that can measure HRV accurately.
This episode is about a health metric you may not have heard of before: heart rate variability, or HRV. This refers to the small changes in the length of time between each of your heart beats.
Scientists have known about and studied HRV for a long time. In recent years, though, new monitors have come to market that can measure HRV accurately whenever you want.
Five months ago, I got interested in HRV as a more scientific approach to finding the lifestyle changes that work best for me as an individual. It's at the convergence of some important trends in health right now, such as health tech, precision health and the holistic approach in systems biology, which recognizes how interactions among different parts of the body are key to health.
But HRV is just one of many numbers worth paying attention to. For this episode of Making Sense of Science, I spoke with psychologist Dr. Leah Lagos; Dr. Jessilyn Dunn, assistant professor in biomedical engineering at Duke; and Jason Moore, the CEO of Spren and an app called Elite HRV. We talked about what HRV is, research on its benefits, how to measure it, whether it can be used to make improvements in health, and what researchers still need to learn about HRV.
*Talk to your doctor before trying anything discussed in this episode related to HRV and lifestyle changes to raise it.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Show notes
Spren - https://www.spren.com/
Elite HRV - https://elitehrv.com/
Jason Moore's Twitter - https://twitter.com/jasonmooreme?lang=en
Dr. Jessilyn Dunn's Twitter - https://twitter.com/drjessilyn?lang=en
Dr. Dunn's study on HRV, flu and common cold - https://jamanetwork.com/journals/jamanetworkopen/f...
Dr. Leah Lagos - https://drleahlagos.com/
Dr. Lagos on Star Talk - https://www.youtube.com/watch?v=jC2Q10SonV8
Research on HRV and intermittent fasting - https://pubmed.ncbi.nlm.nih.gov/33859841/
Research on HRV and Mediterranean diet - https://medicalxpress.com/news/2010-06-twin-medite...:~:text=Using%20data%20from%20the%20Emory,eating%20a%20Western%2Dtype%20diet
Devices for HRV biofeedback - https://elitehrv.com/heart-variability-monitors-an...
Benefits of HRV biofeedback - https://pubmed.ncbi.nlm.nih.gov/32385728/
HRV and cognitive performance - https://www.frontiersin.org/articles/10.3389/fnins...
HRV and emotional regulation - https://pubmed.ncbi.nlm.nih.gov/36030986/
Fortune article on HRV - https://fortune.com/well/2022/12/26/heart-rate-var...
Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
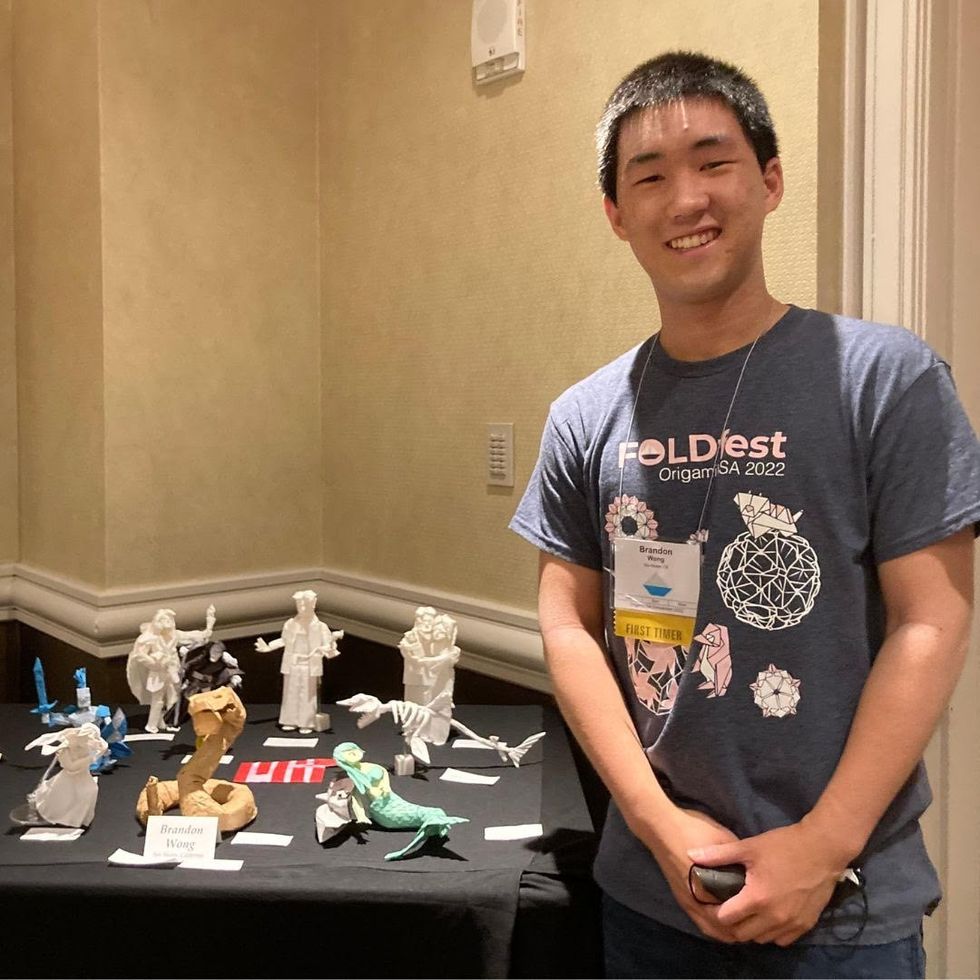
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”

