He Beat Lymphoma at 31, While Pioneering Breakthroughs in Cancer Research

Taylor Schreiber, now 39, runs an immunotherapy company testing drugs that may be less toxic alternative to chemotherapy.
It looked like only good things were ahead of Taylor Schreiber in 2010.
Schreiber had just finished his PhD in cancer biology and was preparing to return to medical school to complete his degree. He also had been married a year, and, like any young newlyweds up for adventure, he and his wife Nicki decided to go backpacking in the Costa Rican rainforest.
He was 31, and it was April Fool's Day—but no joke.
During the trip, he experienced a series of night sweats and didn't think too much about it. Schreiber hadn't been feeling right for a few weeks and assumed he had a respiratory infection. Besides, they were sleeping outdoors in a hot, tropical jungle.
But the night sweats continued even after he got home, leaving his mattress so soaked in the morning it was if a bucket of water had been dumped on him overnight. On instinct, he called one of his thesis advisors at the Sylvester Comprehensive Cancer Center in Florida and described his symptoms.
Dr. Joseph Rosenblatt didn't hesitate. "It sounds like Hodgkins. Come see me tomorrow," he said.
The next day, Schreiber was diagnosed with Stage 3b Hodgkin Lymphoma, which meant the disease was advanced. He was 31, and it was April Fool's Day—but no joke.
"I was scared to death," he recalls. "[Thank] goodness it's one of those cancers that is highly treatable. But being 31 years old and all of a sudden being told that you have a 30 percent of mortality within the next two years wasn't anything that I was relieved about."
For Schreiber, the diagnosis was a personal and professional game-changer. He couldn't work in the hospital as a medical student while undergoing chemotherapy, so he wound up remaining in his post-doctorate lab for another two years. The experience also solidified his decision to apply his scientific and medical knowledge to drug development.
Today, now 39, Schreiber is co-founder, director and chief scientific officer of Shattuck Labs, an immuno-oncology startup, and the developer of several important research breakthroughs in the field of immunotherapy.
After his diagnosis, he continued working full-time as a postdoc, while undergoing an aggressive chemotherapy regimen.
"These days, I look back on [my cancer] and think it was one of the luckiest things that ever happened to me," he says. "In medical school, you learn what it is to treat people and learn about the disease. But there is nothing like being a patient to teach you another side of medicine."
Medicine first called to Schreiber when his maternal grandfather was dying from lung cancer complications. Schreiber's uncle, a radiologist at the medical center where his grandfather was being treated, took him on a tour of his department and showed him images of the insides of his body on an ultrasound machine.
Schreiber was mesmerized. His mother was a teacher and his dad sold windows, so medicine was not something to which he had been routinely exposed.
"This weird device was like looking through jelly, and I thought that was the coolest thing ever," he says.
The experience led him to his first real job at the Catholic Medical Center in Manchester, NH, then to a semester-long internship program during his senior year in high school in Concord Hospital's radiology department.
"This was a great experience, but it also made clear that there was not any meaningful way to learn or contribute to medicine before you obtained a medical degree," says Schreiber, who enrolled in Bucknell College to study biology.
Bench science appealed to him, and he volunteered in Dr. Jing Zhou's nephrology department lab at the Harvard Institutes of Medicine. Under the mentorship of one of her post-docs, Lei Guo, he learned a range of critical techniques in molecular biology, leading to their discovery of a new gene related to human polycystic kidney disease and his first published paper.
Before his cancer diagnosis, Schreiber also volunteered in the lab of Dr. Robert "Doc" Sackstein, a world-renowned bone marrow transplant physician and biomedical researcher, and his interests began to shift towards immunology.
"He was just one of those dynamic people who has a real knack for teaching, first of all, and for inspiring people to want to learn more and ask hard questions and understand experimental medicine," Schreiber says.
It was there that he learned the scientific method and the importance of incorporating the right controls in experiments—a simple idea, but difficult to perform well. He also made what Sackstein calls "a startling discovery" about chemokines, which are signaling proteins that can activate an immune response.
As immune cells travel around our bodies looking for potential sources of infection or disease, they latch onto blood vessel walls and "sniff around" for specific chemical cues that indicate a source of infection. Schreiber and his colleagues designed a system that mimics the blood vessel wall, allowing them to define which chemical cues efficiently drive immune cell migration from the blood into tissues.
Schreiber received the best overall research award in 2008 from the National Student Research Foundation. But even as Schreiber's expertise about immunology grew, his own immune system was about to fight its hardest battle.
After his diagnosis, he continued working full-time as a postdoc in the lab of Eckhard Podack, then chair of the microbiology and immunology department at the University of Miami's Leonard M. Miller School of Medicine.
At the same time, Schreiber began an aggressive intravenous chemotherapy regimen of adriamycin, bleomycin, vincristine and dacarbazine, every two weeks, for 6 months. His wife Nicki, an obgyn, transferred her residency from Emory University in Atlanta to Miami so they could be together.
"It was a weird period. I mean, it made me feel good to keep doing things and not just lay idle," he said. "But by the second cycle of chemo, I was immunosuppressed and losing my hair and wore a face mask walking around the lab, which I was certainly self-conscious. But everyone around me didn't make me feel like an alien so I just went about my business."
The experience reinforced his desire to stay in immunology, especially after having taken the most toxic chemotherapies.
He stayed home the day after chemo when he felt his worst, then rested his body and timed exercise to give the drugs the best shot of targeting sick cells (a strategy, he says, that "could have been voodoo"). He also drank "an incredible" amount of fluids to help flush the toxins out of his system.
Side effects of the chemo, besides hair loss, included intense nausea, diarrhea, a loss of appetite, some severe lung toxicities that eventually resolved, and incredible fatigue.
"I've always been a runner, and I would even try to run while I was doing chemo," he said. "After I finished treatment, I would go literally 150 yards and just have to stop, and it took a lot of effort to work through it."
The experience reinforced his desire to stay in immunology, especially after having taken the most toxic chemotherapies.
"They worked, and I could tolerate them because I was young, but people who are older can't," Schreiber said. "The whole field of immunotherapy has really demonstrated that there are effective therapies out there that don't come with all of the same toxicities as the original chemo, so it was galvanizing to imagine contributing to finding some of those."
Schreiber went on to complete his MD and PhD degrees from the Sheila and David Fuente Program in Cancer Biology at the Miller School of Medicine and was nominated in 2011 as a Future Leader in Cancer Research by the American Association for Cancer Research. He also has numerous publications in the fields of tumor immunology and immunotherapy.
Sackstein, who was struck by Schreiber's enthusiasm and "boundless energy," predicts he will be a "major player in the world of therapeutics."
"The future for Taylor is amazing because he has the capacity to synthesize current knowledge and understand the gaps and then ask the right questions to establish new paradigms," said Sackstein, currently dean of the Herbert Wertheim College of Medicine at Florida International University. "It's a very unusual talent."
Since then, he has devoted his career to developing innovative techniques aimed at unleashing the immune system to attack cancer with less toxicity than chemotherapy and better clinical results—first, at a company called Heat Biologics and then at Pelican Therapeutics.
His primary work at Austin, Texas-based Shattuck is aimed at combining two functions in a single therapy for cancer and inflammatory diseases, blocking molecules that put a brake on the immune system (checkpoint inhibitors) while also stimulating the immune system's cancer-killing T cells.
The company has one drug in clinical testing as part of its Agonist Redirected Checkpoint (ARC) platform, which represents a new class of biological medicine. Two others are expected within the next year, with a pipeline of more than 250 drug candidates spanning cancer, inflammatory, and metabolic diseases.
Nine years after his own cancer diagnosis, Schreiber says it remains a huge part of his life, though his chances of a cancer recurrence today are about the same as his chances of getting newly diagnosed with any other cancer.
"I feel blessed to be in a position to help cancer patients live longer and could not imagine a more fulfilling way to spend my life," he says.
Thanks to safety cautions from the COVID-19 pandemic, a strain of influenza has been completely eliminated.
If you were one of the millions who masked up, washed your hands thoroughly and socially distanced, pat yourself on the back—you may have helped change the course of human history.
Scientists say that thanks to these safety precautions, which were introduced in early 2020 as a way to stop transmission of the novel COVID-19 virus, a strain of influenza has been completely eliminated. This marks the first time in human history that a virus has been wiped out through non-pharmaceutical interventions, such as vaccines.
The flu shot, explained
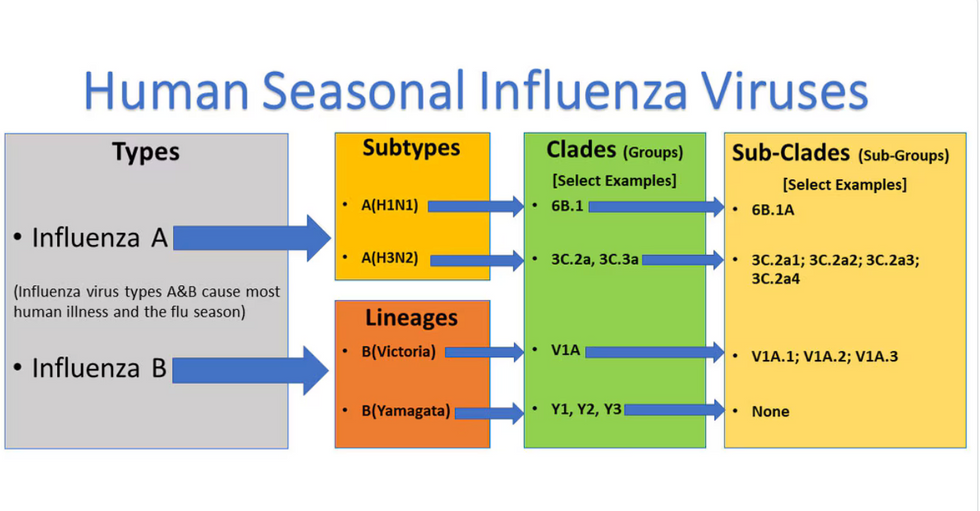
Influenza viruses type A and B are responsible for the majority of human illnesses and the flu season.
Centers for Disease Control
For more than a decade, flu shots have protected against two types of the influenza virus–type A and type B. While there are four different strains of influenza in existence (A, B, C, and D), only strains A, B, and C are capable of infecting humans, and only A and B cause pandemics. In other words, if you catch the flu during flu season, you’re most likely sick with flu type A or B.
Flu vaccines contain inactivated—or dead—influenza virus. These inactivated viruses can’t cause sickness in humans, but when administered as part of a vaccine, they teach a person’s immune system to recognize and kill those viruses when they’re encountered in the wild.
Each spring, a panel of experts gives a recommendation to the US Food and Drug Administration on which strains of each flu type to include in that year’s flu vaccine, depending on what surveillance data says is circulating and what they believe is likely to cause the most illness during the upcoming flu season. For the past decade, Americans have had access to vaccines that provide protection against two strains of influenza A and two lineages of influenza B, known as the Victoria lineage and the Yamagata lineage. But this year, the seasonal flu shot won’t include the Yamagata strain, because the Yamagata strain is no longer circulating among humans.
How Yamagata Disappeared

Flu surveillance data from the Global Initiative on Sharing All Influenza Data (GISAID) shows that the Yamagata lineage of flu type B has not been sequenced since April 2020.
Nature
Experts believe that the Yamagata lineage had already been in decline before the pandemic hit, likely because the strain was naturally less capable of infecting large numbers of people compared to the other strains. When the COVID-19 pandemic hit, the resulting safety precautions such as social distancing, isolating, hand-washing, and masking were enough to drive the virus into extinction completely.
Because the strain hasn’t been circulating since 2020, the FDA elected to remove the Yamagata strain from the seasonal flu vaccine. This will mark the first time since 2012 that the annual flu shot will be trivalent (three-component) rather than quadrivalent (four-component).
Should I still get the flu shot?
The flu shot will protect against fewer strains this year—but that doesn’t mean we should skip it. Influenza places a substantial health burden on the United States every year, responsible for hundreds of thousands of hospitalizations and tens of thousands of deaths. The flu shot has been shown to prevent millions of illnesses each year (more than six million during the 2022-2023 season). And while it’s still possible to catch the flu after getting the flu shot, studies show that people are far less likely to be hospitalized or die when they’re vaccinated.
Another unexpected benefit of dropping the Yamagata strain from the seasonal vaccine? This will possibly make production of the flu vaccine faster, and enable manufacturers to make more vaccines, helping countries who have a flu vaccine shortage and potentially saving millions more lives.
After his grandmother’s dementia diagnosis, one man invented a snack to keep her healthy and hydrated.
Founder Lewis Hornby and his grandmother Pat, sampling Jelly Drops—an edible gummy containing water and life-saving electrolytes.
On a visit to his grandmother’s nursing home in 2016, college student Lewis Hornby made a shocking discovery: Dehydration is a common (and dangerous) problem among seniors—especially those that are diagnosed with dementia.
Hornby’s grandmother, Pat, had always had difficulty keeping up her water intake as she got older, a common issue with seniors. As we age, our body composition changes, and we naturally hold less water than younger adults or children, so it’s easier to become dehydrated quickly if those fluids aren’t replenished. What’s more, our thirst signals diminish naturally as we age as well—meaning our body is not as good as it once was in letting us know that we need to rehydrate. This often creates a perfect storm that commonly leads to dehydration. In Pat’s case, her dehydration was so severe she nearly died.
When Lewis Hornby visited his grandmother at her nursing home afterward, he learned that dehydration especially affects people with dementia, as they often don’t feel thirst cues at all, or may not recognize how to use cups correctly. But while dementia patients often don’t remember to drink water, it seemed to Hornby that they had less problem remembering to eat, particularly candy.

Hornby wanted to create a solution for elderly people who struggled keeping their fluid intake up. He spent the next eighteen months researching and designing a solution and securing funding for his project. In 2019, Hornby won a sizable grant from the Alzheimer’s Society, a UK-based care and research charity for people with dementia and their caregivers. Together, through the charity’s Accelerator Program, they created a bite-sized, sugar-free, edible jelly drop that looked and tasted like candy. The candy, called Jelly Drops, contained 95% water and electrolytes—important minerals that are often lost during dehydration. The final product launched in 2020—and was an immediate success. The drops were able to provide extra hydration to the elderly, as well as help keep dementia patients safe, since dehydration commonly leads to confusion, hospitalization, and sometimes even death.
Not only did Jelly Drops quickly become a favorite snack among dementia patients in the UK, but they were able to provide an additional boost of hydration to hospital workers during the pandemic. In NHS coronavirus hospital wards, patients infected with the virus were regularly given Jelly Drops to keep their fluid levels normal—and staff members snacked on them as well, since long shifts and personal protective equipment (PPE) they were required to wear often left them feeling parched.
In April 2022, Jelly Drops launched in the United States. The company continues to donate 1% of its profits to help fund Alzheimer’s research.

