He Poisoned Himself to Find a Cure for Stomach Ulcers -- And Won a Nobel Prize

Dr. Barry Marshall (along with a collaborator) discovered that the bacteria H. Pylori, pictured, caused stomach ulcers.
[Editor's Note: Welcome to Leaps of the Past, a new monthly column that spotlights the fascinating backstory behind a medical or scientific breakthrough from history.]
------
Until about 40 years ago, ulcers were a mysterious – and sometimes deadly – ailment. Found in a person's stomach lining or intestine, ulcers are small sores that cause a variety of painful symptoms, such as vomiting, a burning or aching sensation, internal bleeding and stomach obstruction. Patients with ulcers suffered for years without a cure and sometimes even needed their stomachs completely removed to rid them from pain.
"To gastroenterologists, the concept of a germ causing ulcers was like saying the Earth is flat."
In the early 1980s, the majority of scientists thought that ulcers were caused by stress or poor diet. But a handful of scientists had a different theory: They believed that ulcers were caused by a corkscrew-shaped bacterium called Helicobacter pylori, or H. pylori for short. Robin Warren, a pathologist, and Barry Marshall, an internist, were the two pioneers of this theory, and the two teamed up to study H. pylori at the Royal Perth Hospital in 1981.
The pair started off by trying to culture the bacteria in the stomachs of patients with gastritis, an inflammation of the stomach lining and a precursor to developing an ulcer. Initially, the microbiologists involved in their clinical trial found no trace of the bacteria from patient samples – but after a few weeks, the microbiologists discovered that their lab techs had been throwing away the cultures before H. pylori could grow. "After that, we let the cultures grow longer and found 13 patients with duodenal ulcer," said Marshall in a later interview. "All of them had the bacteria."
Marshall and Warren also cultured H. pylori in the stomachs of patients with stomach cancer. They observed that "everybody with stomach cancer developed it on a background of gastritis. Whenever we found a person without Helicobacter, we couldn't find gastritis either." Marshall and Warren were convinced that H. pylori not only caused gastritis and peptic ulcers, but stomach cancer as well.
But when the team presented their findings at an annual meeting of the Royal Australasian College of Physicians in Perth, they were mostly met with skepticism. "To gastroenterologists, the concept of a germ causing ulcers was like saying the Earth is flat," Marshall said. "The idea was too weird."
Warren started treating his gastritis patients with antibiotics with great success – but other internists remained doubtful, continuing to treat their patients with antacids instead. Making matters more complicated, neither Warren nor Marshall could readily test their theory, since the pair only had lab mice at their disposal and H. pylori infects only humans and non-human primates, such as rhesus monkeys.
So Marshall took an unconventional approach. First, he underwent two tests to get a baseline reading of his stomach, which showed no presence of H. pylori. Then, Marshall took some H. pylori bacteria from a petri dish, mixed it with beef extract to create a broth, and gulped it down. If his theory was correct, a second gastric biopsy would show that his stomach was overrun with H. pylori bacteria, and a second endoscopy would show a painfully inflamed stomach – gastritis.
Less than a week later, Marshall started feeling sick. "I expected to develop an asymptomatic infection," he later said in an interview published in the Canadian Journal of Gastroenterology. "… [but] after five days, I started to have bloating and fullness after the evening meal, and my appetite decreased. My breath was bad and I vomited clear watery liquid, without acid, each morning."
At his wife's urging, Marshall started on a regimen of antibiotics to kill off the burgeoning bacteria, so a follow-up biopsy showed no signs of H. pylori. A follow-up endoscopy, however, showed "severe active gastritis" along with epithelial damage. This was the smoking gun other clinicians needed to believe that H. pylori caused gastritis and stomach cancer. When they began to treat their gastritis patients with antibiotics, the rate of peptic ulcers in the Australian population diminished by 70 percent.
Today, antibiotics are the standard of care for anyone afflicted with gastritis.
In 2005, Marshall and Warren were awarded the Nobel Prize in Physiology or Medicine for their discovery of H. Pylori and its role in developing gastritis and peptic ulcers. "Thanks to the pioneering discovery by Marshall and Warren, peptic ulcer disease is no longer a chronic, frequently disabling condition, but a disease that can be cured by a short regimen of antibiotics and acid secretion inhibitors," the Nobel Prize Committee said.
Today, antibiotics are the standard of care for anyone afflicted with gastritis – and stomach cancer has been significantly reduced in the Western world.
A robot server, controlled remotely by a disabled worker, delivers drinks to patrons at the DAWN cafe in Tokyo.
A sleek, four-foot tall white robot glides across a cafe storefront in Tokyo’s Nihonbashi district, holding a two-tiered serving tray full of tea sandwiches and pastries. The cafe’s patrons smile and say thanks as they take the tray—but it’s not the robot they’re thanking. Instead, the patrons are talking to the person controlling the robot—a restaurant employee who operates the avatar from the comfort of their home.
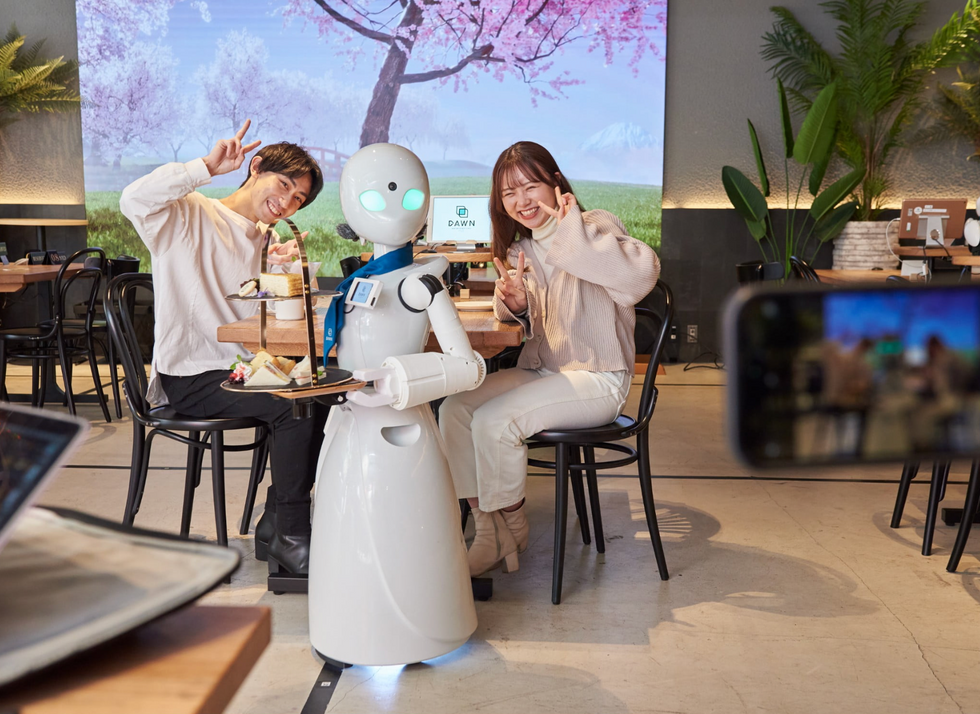
It’s a typical scene at DAWN, short for Diverse Avatar Working Network—a cafe that launched in Tokyo six years ago as an experimental pop-up and quickly became an overnight success. Today, the cafe is a permanent fixture in Nihonbashi, staffing roughly 60 remote workers who control the robots remotely and communicate to customers via a built-in microphone.
More than just a creative idea, however, DAWN is being hailed as a life-changing opportunity. The workers who control the robots remotely (known as “pilots”) all have disabilities that limit their ability to move around freely and travel outside their homes. Worldwide, an estimated 16 percent of the global population lives with a significant disability—and according to the World Health Organization, these disabilities give rise to other problems, such as exclusion from education, unemployment, and poverty.
These are all problems that Kentaro Yoshifuji, founder and CEO of Ory Laboratory, which supplies the robot servers at DAWN, is looking to correct. Yoshifuji, who was bedridden for several years in high school due to an undisclosed health problem, launched the company to help enable people who are house-bound or bedridden to more fully participate in society, as well as end the loneliness, isolation, and feelings of worthlessness that can sometimes go hand-in-hand with being disabled.
“It’s heartbreaking to think that [people with disabilities] feel they are a burden to society, or that they fear their families suffer by caring for them,” said Yoshifuji in an interview in 2020. “We are dedicating ourselves to providing workable, technology-based solutions. That is our purpose.”

Shota, Kuwahara, a DAWN employee with muscular dystrophy, agrees. "There are many difficulties in my daily life, but I believe my life has a purpose and is not being wasted," he says. "Being useful, able to help other people, even feeling needed by others, is so motivational."
A woman receives a mammogram, which can detect the presence of tumors in a patient's breast.
When a patient is diagnosed with early-stage breast cancer, having surgery to remove the tumor is considered the standard of care. But what happens when a patient can’t have surgery?
Whether it’s due to high blood pressure, advanced age, heart issues, or other reasons, some breast cancer patients don’t qualify for a lumpectomy—one of the most common treatment options for early-stage breast cancer. A lumpectomy surgically removes the tumor while keeping the patient’s breast intact, while a mastectomy removes the entire breast and nearby lymph nodes.
Fortunately, a new technique called cryoablation is now available for breast cancer patients who either aren’t candidates for surgery or don’t feel comfortable undergoing a surgical procedure. With cryoablation, doctors use an ultrasound or CT scan to locate any tumors inside the patient’s breast. They then insert small, needle-like probes into the patient's breast which create an “ice ball” that surrounds the tumor and kills the cancer cells.
Cryoablation has been used for decades to treat cancers of the kidneys and liver—but only in the past few years have doctors been able to use the procedure to treat breast cancer patients. And while clinical trials have shown that cryoablation works for tumors smaller than 1.5 centimeters, a recent clinical trial at Memorial Sloan Kettering Cancer Center in New York has shown that it can work for larger tumors, too.
In this study, doctors performed cryoablation on patients whose tumors were, on average, 2.5 centimeters. The cryoablation procedure lasted for about 30 minutes, and patients were able to go home on the same day following treatment. Doctors then followed up with the patients after 16 months. In the follow-up, doctors found the recurrence rate for tumors after using cryoablation was only 10 percent.
For patients who don’t qualify for surgery, radiation and hormonal therapy is typically used to treat tumors. However, said Yolanda Brice, M.D., an interventional radiologist at Memorial Sloan Kettering Cancer Center, “when treated with only radiation and hormonal therapy, the tumors will eventually return.” Cryotherapy, Brice said, could be a more effective way to treat cancer for patients who can’t have surgery.
“The fact that we only saw a 10 percent recurrence rate in our study is incredibly promising,” she said.

