He Wants to Eliminate Inherited Diseases in Embryos. Congress Just Said No (Again).
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

Dr. Shoukhrat Mitalipov, May 13, 2013.
Biologist Shoukhrat Mitalipov is famous—and controversial--in the world of cutting-edge fertility treatments. A decade ago, he pioneered mitochondrial replacement therapy, paving the way for the world's first "three-parent" babies to be born free of a devastating inherited disease.
He sees his work toward embryo gene therapy as not only moral, but necessary.
In 2017, he shocked the world again when his group at Oregon Health and Science University became the first to repair a genetic mutation causing heart disease in dozens of human embryos. The embryos were later destroyed a part of the experiment; current policy in the U.S. prohibits such research from moving into clinical trials.
And that policy doesn't look like it's going to change anytime soon, despite recent political wavering. Last month, a House subcommittee dropped the ban that has blocked the Food and Drug Administration since 2015 from considering any clinical trials of genetically altered embryos intended to create a baby. The move raised the hopes of supporters who want to see such research move forward and angered critics who feel that the science is getting ahead of the ethics. But yesterday, a House committee decided to restore the ban on gene-edited babies after all.
As for Mitalipov, he told leapsmag that he sees his work toward embryo gene therapy as not only moral, but necessary. This interview has been edited and condensed for clarity.
What motivates you to pursue this line of research, even though it is highly controversial?
It's my expertise, I'm an embryologist. We study early development in humans -- sperm, egg, and the first five days of development -- and try to use our knowledge to treat human diseases, particularly in that early stage. This is how IVF started, as a treatment for infertility. It's a very successful cell therapy treatment, with millions of children born. [Now the idea is] to actually to use this IVF platform not as much to treat infertility, but also to treat heritable genetic diseases, because this is a very important stage when gametes from either dad or mom will transmit mutations. This is the bottleneck where we could actually interfere and repair that mutation.
Many people are hesitant to support embryo editing because of "designer babies," yet polls do show that Americans are more open to embryo editing for the purpose of disease prevention. Where should society draw a line?
Yeah, I agree with most Americans that we don't have to edit -- meaning you could make all kind of changes. Instead we do gene repair, which is a therapeutic application.
Gene repair is quite different than gene editing. It involves [focusing on] already known disease-causing mutations and how we can turn them back to normal.
Thousands of gene mutations cause human diseases, like Crohn's, for example, or mutations causing cancer, heart disease. These are well-described, well-studied cause-and-effect diseases and we need to do something about it because otherwise it's impossible to treat once the mutation is already passed to a child.
Early intervention is the best in any disease, but in genetics, "early" means you have to do it at the time of fertilization. That's when we are dealing with one copy of the mutation or maybe two, versus when you have a whole body with billions of cells in solid tissues that we cannot really access and target. So this is the most efficient way of preventing thousands and thousands of genetic diseases. I understand that we have to make sure that it's very safe, of course, and efficient as well. But at the same time, I think this is the future. We have to work toward developing these technologies.
"If we continue banning the research everywhere and not funding it, maybe 100 years will not be enough."
What's your opinion of Dr. He Jiankui and the Chinese CRISPR'ed babies?
This is a case where he was doing gene editing, not gene repair. He hasn't corrected anything, he induced a mutation to normal human genes, hoping that this would somehow confer resistance to HIV, which is still unclear.
I think such straightforward editing is unacceptable specifically for human embryos. He's approach has also never been tested in an animal model. That's why the reaction from the public and scientists was very negative, because this is the case where the doctor does this without any expertise in this area, without knowing probably much about what he is doing, and he acquired it without any oversights, which is troubling. And of course, it negatively affects the legitimate research that is going on in some labs.
What might the future of embryo gene therapy look like?
Hopefully in 10 years from now, thousands and thousands of families that know they carry germline mutations…could go through IVF and we would correct it, and they could have healthy children.
Right now, we have some tools. We cannot correct, but we can select. So what happens is the parents become pregnant and then at about three months along, we can biopsy the amniotic fluid and say, "Hey unfortunately you passed on this mutation." And that means this child, if it's born, will be affected, so we give parents a choice of terminating the pregnancy.
Or we could do it much earlier, so parents go to the IVF clinic where we retrieve about ten eggs, after stimulating a woman's ovaries. Each of them will be fertilized so we have ten embryos that develop. We have a five-day window where we can keep them in the lab. And we basically reap a few cells, we do a biopsy from each of these ten, and we say, "Hey embryo number 1 and number 4 are not mutant, but the others are."
Then we can take these two and the other eight usually will be thrown away. That's the technology that we have now. Some ethicists argue on religious grounds that we have this selection technology available, so why do we need germline gene therapy [i.e. repairing the disease-causing mutations in an embryo]?
I don't understand the moral argument there, because all the available technology is based on selective destruction of the embryo.
With [IVF gene therapy], we will take ten embryos and every embryo we'll make healthy because we can get rid of the mutations. How could embryo destruction be morally superior?
How long do you think it will take for this technology to be available to prospective parents?
It depends how many legitimate labs with expertise can get into this field and resolve all the scientific questions. If we continue banning the research everywhere and not funding it, maybe 100 years will not be enough.
So far, I think that my lab is the only one legitimately working on it. But we would like five, 10, maybe 100 labs in this country and Europe really working. Because we have scientific challenges that we need to resolve before we could say, "Hey now we know how to correct [a given mutation] and now this could be efficient, and there are no side effects or very little." And then we could say, "Okay, I think we've done everything we could in petri dishes and in animals, and now we are ready to transplant this embryo in a patient and see what happens."
"There's just no way you could sink your head into the sand and say, 'Oh, we just ban it and then hopefully everything will go away.'"
Does banning emerging technology actually work?
Banning it usually means it will leak out to a gray area where there's no regulation and many private IVF clinics will just use it while it is still premature. So I think we have to regulate the clinical testing. There's just no way you could sink your head into the sand and say, "Oh, we just ban it and then hopefully everything will go away." That's not going to happen.
If this technology does become feasible and legal in the future, do you think that more and more couples will choose IVF and gene therapy versus the natural method of rolling the dice?
As sequencing technology is becoming available, like 23andMe, more and more parents will realize what kind of mutations they carry. And if your spouse carries the same mutation on the same locus, now you have very high chance of transmitting it. Most of the time today, we find out these families carry it once they have one or two children with that condition.
Of course, parents can just do it naturally in the bedroom and have a chance of transmitting or not transmitting mutations, but hopefully eventually we can say, "Hey, because of your condition, you don't want to play this Russian Roulette. Let's just do IVF." And hopefully the government will cover that kind of treatment because right now IVF is not covered in most states. And we do this therapy and then they have a healthy child.
We have 10,000 different mutations in the human population. That means probably billions of people carry mutations. And unless they go through this gene therapy through IVF, they will keep transmitting them. And we're going to keep having millions and millions of children with diseases. We have to do something about it.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Scientists have known about and studied heart rate variability, or HRV, for a long time and, in recent years, monitors have come to market that can measure HRV accurately.
This episode is about a health metric you may not have heard of before: heart rate variability, or HRV. This refers to the small changes in the length of time between each of your heart beats.
Scientists have known about and studied HRV for a long time. In recent years, though, new monitors have come to market that can measure HRV accurately whenever you want.
Five months ago, I got interested in HRV as a more scientific approach to finding the lifestyle changes that work best for me as an individual. It's at the convergence of some important trends in health right now, such as health tech, precision health and the holistic approach in systems biology, which recognizes how interactions among different parts of the body are key to health.
But HRV is just one of many numbers worth paying attention to. For this episode of Making Sense of Science, I spoke with psychologist Dr. Leah Lagos; Dr. Jessilyn Dunn, assistant professor in biomedical engineering at Duke; and Jason Moore, the CEO of Spren and an app called Elite HRV. We talked about what HRV is, research on its benefits, how to measure it, whether it can be used to make improvements in health, and what researchers still need to learn about HRV.
*Talk to your doctor before trying anything discussed in this episode related to HRV and lifestyle changes to raise it.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Show notes
Spren - https://www.spren.com/
Elite HRV - https://elitehrv.com/
Jason Moore's Twitter - https://twitter.com/jasonmooreme?lang=en
Dr. Jessilyn Dunn's Twitter - https://twitter.com/drjessilyn?lang=en
Dr. Dunn's study on HRV, flu and common cold - https://jamanetwork.com/journals/jamanetworkopen/f...
Dr. Leah Lagos - https://drleahlagos.com/
Dr. Lagos on Star Talk - https://www.youtube.com/watch?v=jC2Q10SonV8
Research on HRV and intermittent fasting - https://pubmed.ncbi.nlm.nih.gov/33859841/
Research on HRV and Mediterranean diet - https://medicalxpress.com/news/2010-06-twin-medite...:~:text=Using%20data%20from%20the%20Emory,eating%20a%20Western%2Dtype%20diet
Devices for HRV biofeedback - https://elitehrv.com/heart-variability-monitors-an...
Benefits of HRV biofeedback - https://pubmed.ncbi.nlm.nih.gov/32385728/
HRV and cognitive performance - https://www.frontiersin.org/articles/10.3389/fnins...
HRV and emotional regulation - https://pubmed.ncbi.nlm.nih.gov/36030986/
Fortune article on HRV - https://fortune.com/well/2022/12/26/heart-rate-var...
Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
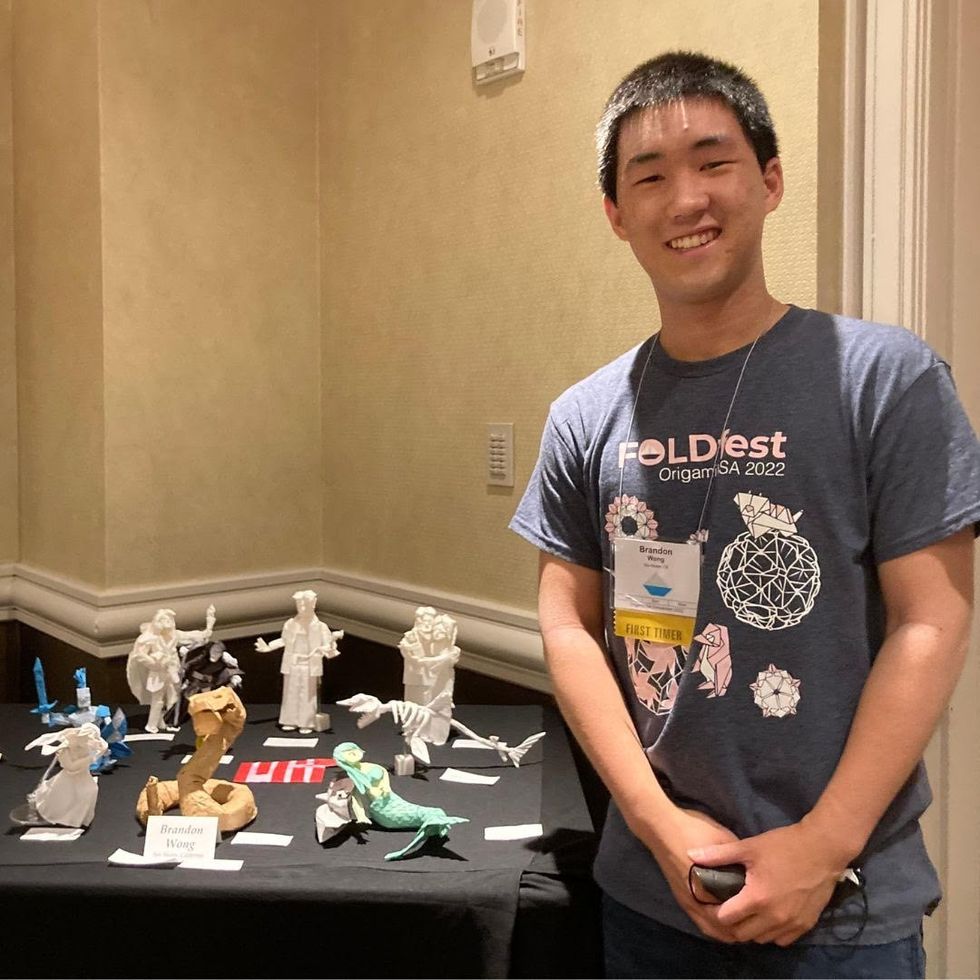
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”

