AI and you: Is the promise of personalized nutrition apps worth the hype?

Personalized nutrition apps could provide valuable data to people trying to eat healthier, though more research must be done to show effectiveness.
As a type 2 diabetic, Michael Snyder has long been interested in how blood sugar levels vary from one person to another in response to the same food, and whether a more personalized approach to nutrition could help tackle the rapidly cascading levels of diabetes and obesity in much of the western world.
Eight years ago, Snyder, who directs the Center for Genomics and Personalized Medicine at Stanford University, decided to put his theories to the test. In the 2000s continuous glucose monitoring, or CGM, had begun to revolutionize the lives of diabetics, both type 1 and type 2. Using spherical sensors which sit on the upper arm or abdomen – with tiny wires that pierce the skin – the technology allowed patients to gain real-time updates on their blood sugar levels, transmitted directly to their phone.
It gave Snyder an idea for his research at Stanford. Applying the same technology to a group of apparently healthy people, and looking for ‘spikes’ or sudden surges in blood sugar known as hyperglycemia, could provide a means of observing how their bodies reacted to an array of foods.
“We discovered that different foods spike people differently,” he says. “Some people spike to pasta, others to bread, others to bananas, and so on. It’s very personalized and our feeling was that building programs around these devices could be extremely powerful for better managing people’s glucose.”
Unbeknown to Snyder at the time, thousands of miles away, a group of Israeli scientists at the Weizmann Institute of Science were doing exactly the same experiments. In 2015, they published a landmark paper which used CGM to track the blood sugar levels of 800 people over several days, showing that the biological response to identical foods can vary wildly. Like Snyder, they theorized that giving people a greater understanding of their own glucose responses, so they spend more time in the normal range, may reduce the prevalence of type 2 diabetes.
The commercial potential of such apps is clear, but the underlying science continues to generate intriguing findings.
“At the moment 33 percent of the U.S. population is pre-diabetic, and 70 percent of those pre-diabetics will become diabetic,” says Snyder. “Those numbers are going up, so it’s pretty clear we need to do something about it.”
Fast forward to 2022,and both teams have converted their ideas into subscription-based dietary apps which use artificial intelligence to offer data-informed nutritional and lifestyle recommendations. Snyder’s spinoff, January AI, combines CGM information with heart rate, sleep, and activity data to advise on foods to avoid and the best times to exercise. DayTwo–a start-up which utilizes the findings of Weizmann Institute of Science–obtains microbiome information by sequencing stool samples, and combines this with blood glucose data to rate ‘good’ and ‘bad’ foods for a particular person.
“CGMs can be used to devise personalized diets,” says Eran Elinav, an immunology professor and microbiota researcher at the Weizmann Institute of Science in addition to serving as a scientific consultant for DayTwo. “However, this process can be cumbersome. Therefore, in our lab we created an algorithm, based on data acquired from a big cohort of people, which can accurately predict post-meal glucose responses on a personal basis.”
The commercial potential of such apps is clear. DayTwo, who market their product to corporate employers and health insurers rather than individual consumers, recently raised $37 million in funding. But the underlying science continues to generate intriguing findings.
Last year, Elinav and colleagues published a study on 225 individuals with pre-diabetes which found that they achieved better blood sugar control when they followed a personalized diet based on DayTwo’s recommendations, compared to a Mediterranean diet. The journal Cell just released a new paper from Snyder’s group which shows that different types of fibre benefit people in different ways.
“The idea is you hear different fibres are good for you,” says Snyder. “But if you look at fibres they’re all over the map—it’s like saying all animals are the same. The responses are very individual. For a lot of people [a type of fibre called] arabinoxylan clearly reduced cholesterol while the fibre inulin had no effect. But in some people, it was the complete opposite.”

Eight years ago, Stanford's Michael Snyder began studying how continuous glucose monitors could be used by patients to gain real-time updates on their blood sugar levels, transmitted directly to their phone.
The Snyder Lab, Stanford Medicine
Because of studies like these, interest in precision nutrition approaches has exploded in recent years. In January, the National Institutes of Health announced that they are spending $170 million on a five year, multi-center initiative which aims to develop algorithms based on a whole range of data sources from blood sugar to sleep, exercise, stress, microbiome and even genomic information which can help predict which diets are most suitable for a particular individual.
“There's so many different factors which influence what you put into your mouth but also what happens to different types of nutrients and how that ultimately affects your health, which means you can’t have a one-size-fits-all set of nutritional guidelines for everyone,” says Bruce Y. Lee, professor of health policy and management at the City University of New York Graduate School of Public Health.
With the falling costs of genomic sequencing, other precision nutrition clinical trials are choosing to look at whether our genomes alone can yield key information about what our diets should look like, an emerging field of research known as nutrigenomics.
The ASPIRE-DNA clinical trial at Imperial College London is aiming to see whether particular genetic variants can be used to classify individuals into two groups, those who are more glucose sensitive to fat and those who are more sensitive to carbohydrates. By following a tailored diet based on these sensitivities, the trial aims to see whether it can prevent people with pre-diabetes from developing the disease.
But while much hope is riding on these trials, even precision nutrition advocates caution that the field remains in the very earliest of stages. Lars-Oliver Klotz, professor of nutrigenomics at Friedrich-Schiller-University in Jena, Germany, says that while the overall goal is to identify means of avoiding nutrition-related diseases, genomic data alone is unlikely to be sufficient to prevent obesity and type 2 diabetes.
“Genome data is rather simple to acquire these days as sequencing techniques have dramatically advanced in recent years,” he says. “However, the predictive value of just genome sequencing is too low in the case of obesity and prediabetes.”
Others say that while genomic data can yield useful information in terms of how different people metabolize different types of fat and specific nutrients such as B vitamins, there is a need for more research before it can be utilized in an algorithm for making dietary recommendations.
“I think it’s a little early,” says Eileen Gibney, a professor at University College Dublin. “We’ve identified a limited number of gene-nutrient interactions so far, but we need more randomized control trials of people with different genetic profiles on the same diet, to see whether they respond differently, and if that can be explained by their genetic differences.”
Some start-ups have already come unstuck for promising too much, or pushing recommendations which are not based on scientifically rigorous trials. The world of precision nutrition apps was dubbed a ‘Wild West’ by some commentators after the founders of uBiome – a start-up which offered nutritional recommendations based on information obtained from sequencing stool samples –were charged with fraud last year. The weight-loss app Noom, which was valued at $3.7 billion in May 2021, has been criticized on Twitter by a number of users who claimed that its recommendations have led to them developed eating disorders.
With precision nutrition apps marketing their technology at healthy individuals, question marks have also been raised about the value which can be gained through non-diabetics monitoring their blood sugar through CGM. While some small studies have found that wearing a CGM can make overweight or obese individuals more motivated to exercise, there is still a lack of conclusive evidence showing that this translates to improved health.
However, independent researchers remain intrigued by the technology, and say that the wealth of data generated through such apps could be used to help further stratify the different types of people who become at risk of developing type 2 diabetes.
“CGM not only enables a longer sampling time for capturing glucose levels, but will also capture lifestyle factors,” says Robert Wagner, a diabetes researcher at University Hospital Düsseldorf. “It is probable that it can be used to identify many clusters of prediabetic metabolism and predict the risk of diabetes and its complications, but maybe also specific cardiometabolic risk constellations. However, we still don’t know which forms of diabetes can be prevented by such approaches and how feasible and long-lasting such self-feedback dietary modifications are.”
Snyder himself has now been wearing a CGM for eight years, and he credits the insights it provides with helping him to manage his own diabetes. “My CGM still gives me novel insights into what foods and behaviors affect my glucose levels,” he says.
He is now looking to run clinical trials with his group at Stanford to see whether following a precision nutrition approach based on CGM and microbiome data, combined with other health information, can be used to reverse signs of pre-diabetes. If it proves successful, January AI may look to incorporate microbiome data in future.
“Ultimately, what I want to do is be able take people’s poop samples, maybe a blood draw, and say, ‘Alright, based on these parameters, this is what I think is going to spike you,’ and then have a CGM to test that out,” he says. “Getting very predictive about this, so right from the get go, you can have people better manage their health and then use the glucose monitor to help follow that.”
Scientists Are Working to Decipher the Puzzle of ‘Broken Heart Syndrome’
Elaine Kamil had just returned home after a few days of business meetings in 2013 when she started having chest pains. At first Kamil, then 66, wasn't worried—she had had some chest pain before and recently went to a cardiologist to do a stress test, which was normal.
"I can't be having a heart attack because I just got checked," she thought, attributing the discomfort to stress and high demands of her job. A pediatric nephrologist at Cedars-Sinai Hospital in Los Angeles, she takes care of critically ill children who are on dialysis or are kidney transplant patients. Supporting families through difficult times and answering calls at odd hours is part of her daily routine, and often leaves her exhausted.
She figured the pain would go away. But instead, it intensified that night. Kamil's husband drove her to the Cedars-Sinai hospital, where she was admitted to the coronary care unit. It turned out she wasn't having a heart attack after all. Instead, she was diagnosed with a much less common but nonetheless dangerous heart condition called takotsubo syndrome, or broken heart syndrome.
A heart attack happens when blood flow to the heart is obstructed—such as when an artery is blocked—causing heart muscle tissue to die. In takotsubo syndrome, the blood flow isn't blocked, but the heart doesn't pump it properly. The heart changes its shape and starts to resemble a Japanese fishing device called tako-tsubo, a clay pot with a wider body and narrower mouth, used to catch octopus.
"The heart muscle is stunned and doesn't function properly anywhere from three days to three weeks," explains Noel Bairey Merz, the cardiologist at Cedar Sinai who Kamil went to see after she was discharged.
"The heart muscle is stunned and doesn't function properly anywhere from three days to three weeks."
But even though the heart isn't permanently damaged, mortality rates due to takotsubo syndrome are comparable to those of a heart attack, Merz notes—about 4-5 percent of patients die from the attack, and 20 percent within the next five years. "It's as bad as a heart attack," Merz says—only it's much less known, even to doctors. The condition affects only about 1 percent of people, and there are around 15,000 new cases annually. It's diagnosed using a cardiac ventriculogram, an imaging test that allows doctors to see how the heart pumps blood.
Scientists don't fully understand what causes Takotsubo syndrome, but it usually occurs after extreme emotional or physical stress. Doctors think it's triggered by a so-called catecholamine storm, a phenomenon in which the body releases too much catecholamines—hormones involved in the fight-or-flight response. Evolutionarily, when early humans lived in savannas or forests and had to either fight off predators or flee from them, these hormones gave our ancestors the needed strength and stamina to take either action. Released by nerve endings and by the adrenal glands that sit on top of the kidneys, these hormones still flood our bodies in moments of stress, but an overabundance of them could sometimes be damaging.

Elaine Kamil
A study by scientists at Harvard Medical School linked increased risk of takotsubo to higher activity in the amygdala, a brain region responsible for emotions that's involved in responses to stress. The scientists believe that chronic stress makes people more susceptible to the syndrome. Notably, one small study suggested that the number of Takotsubo cases increased during the COVID-19 pandemic.
There are no specific drugs to treat takotsubo, so doctors rely on supportive therapies, which include medications typically used for high blood pressure and heart failure. In most cases, the heart returns to its normal shape within a few weeks. "It's a spontaneous recovery—the catecholamine storm is resolved, the injury trigger is removed and the heart heals itself because our bodies have an amazing healing capacity," Merz says. It also helps that tissues remain intact. 'The heart cells don't die, they just aren't functioning properly for some time."
That's the good news. The bad news is that takotsubo is likely to strike again—in 5-20 percent of patients the condition comes back, sometimes more severe than before.
That's exactly what happened to Kamil. After getting her diagnosis in 2013, she realized that she actually had a previous takotsubo episode. In 2010, she experienced similar symptoms after her son died. "The night after he died, I was having severe chest pain at night, but I was too overwhelmed with grief to do anything about it," she recalls. After a while, the pain subsided and didn't return until three years later.
For weeks after her second attack, she felt exhausted, listless and anxious. "You lose confidence in your body," she says. "You have these little twinges on your chest, or if you start having arrhythmia, and you wonder if this is another episode coming up. It's really unnerving because you don't know how to read these cues." And that's very typical, Merz says. Even when the heart muscle appears to recover, patients don't return to normal right away. They have shortens of breath, they can't exercise, and they stay anxious and worried for a while.
Women over the age of 50 are diagnosed with takotsubo more often than other demographics. However, it happens in men too, although it typically strikes after physical stress, such as a triathlon or an exhausting day of cycling. Young people can also get takotsubo. Older patients are hospitalized more often, but younger people tend to have more severe complications. It could be because an older person may go for a jog while younger one may run a marathon, which would take a stronger toll on the body of a person who's predisposed to the condition.
Notably, the emotional stressors don't always have to be negative—the heart muscle can get out of shape from good emotions, too. "There have been case reports of takotsubo at weddings," Merz says. Moreover, one out of three or four takotsubo patients experience no apparent stress, she adds. "So it could be that it's not so much the catecholamine storm itself, but the body's reaction to it—the physiological reaction deeply embedded into out physiology," she explains.
Merz and her team are working to understand what makes people predisposed to takotsubo. They think a person's genetics play a role, but they haven't yet pinpointed genes that seem to be responsible. Genes code for proteins, which affect how the body metabolizes various compounds, which, in turn, affect the body's response to stress. Pinning down the protein involved in takotsubo susceptibility would allow doctors to develop screening tests and identify those prone to severe repeating attacks. It will also help develop medications that can either prevent it or treat it better than just waiting for the body to heal itself.
Researchers at the Imperial College London found that elevated levels of certain types of microRNAs—molecules involved in protein production—increase the chances of developing takotsubo.
In one study, researchers tried treating takotsubo in mice with a drug called suberanilohydroxamic acid, or SAHA, typically used for cancer treatment. The drug improved cardiac health and reversed the broken heart in rodents. It remains to be seen if the drug would have a similar effect on humans. But identifying a drug that shows promise is progress, Merz says. "I'm glad that there's research in this area."
This article was originally published by Leaps.org on July 28, 2021.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
Did Anton the AI find a new treatment for a deadly cancer?
Researchers used a supercomputer to learn about the subtle movement of a cancer-causing molecule, and then they found the precise drug that can recognize that motion.
Bile duct cancer is a rare and aggressive form of cancer that is often difficult to diagnose. Patients with advanced forms of the disease have an average life expectancy of less than two years.
Many patients who get cancer in their bile ducts – the tubes that carry digestive fluid from the liver to the small intestine – have mutations in the protein FGFR2, which leads cells to grow uncontrollably. One treatment option is chemotherapy, but it’s toxic to both cancer cells and healthy cells, failing to distinguish between the two. Increasingly, cancer researchers are focusing on biomarker directed therapy, or making drugs that target a particular molecule that causes the disease – FGFR2, in the case of bile duct cancer.
A problem is that in targeting FGFR2, these drugs inadvertently inhibit the FGFR1 protein, which looks almost identical. This causes elevated phosphate levels, which is a sign of kidney damage, so doses are often limited to prevent complications.
In recent years, though, a company called Relay has taken a unique approach to picking out FGFR2, using a powerful supercomputer to simulate how proteins move and change shape. The team, leveraging this AI capability, discovered that FGFR2 and FGFR1 move differently, which enabled them to create a more precise drug.
Preliminary studies have shown robust activity of this drug, called RLY-4008, in FGFR2 altered tumors, especially in bile duct cancer. The drug did not inhibit FGFR1 or cause significant side effects. “RLY-4008 is a prime example of a precision oncology therapeutic with its highly selective and potent targeting of FGFR2 genetic alterations and resistance mutations,” says Lipika Goyal, assistant professor of medicine at Harvard Medical School. She is a principal investigator of Relay’s phase 1-2 clinical trial.
Boosts from AI and a billionaire
Traditional drug design has been very much a case of trial and error, as scientists investigate many molecules to see which ones bind to the intended target and bind less to other targets.
“It’s being done almost blindly, without really being guided by structure, so it fails very often,” says Olivier Elemento, associate director of the Institute for Computational Biomedicine at Cornell. “The issue is that they are not sampling enough molecules to cover some of the chemical space that would be specific to the target of interest and not specific to others.”
Relay’s unique hardware and software allow simulations that could never be achieved through traditional experiments, Elemento says.
Some scientists have tried to use X-rays of crystallized proteins to look at the structure of proteins and design better drugs. But they have failed to account for an important factor: proteins are moving and constantly folding into different shapes.
David Shaw, a hedge fund billionaire, wanted to help improve drug discovery and understood that a key obstacle was that computer models of molecular dynamics were limited; they simulated motion for less than 10 millionths of a second.
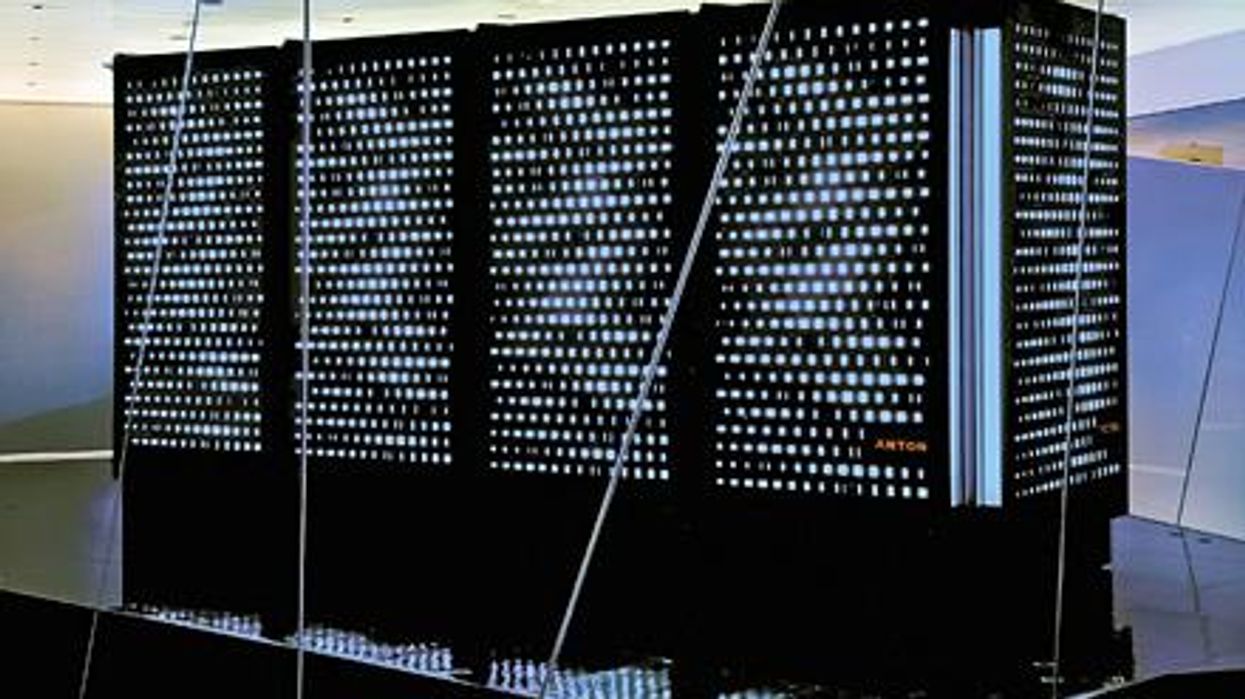
In 2001, Shaw set up his own research facility, D.E. Shaw Research, to create a supercomputer that would be specifically designed to simulate protein motion. Seven years later, he succeeded in firing up a supercomputer that can now conduct high speed simulations roughly 100 times faster than others. Called Anton, it has special computer chips to enable this speed, and its software is powered by AI to conduct many simulations.
After creating the supercomputer, Shaw teamed up with leading scientists who were interested in molecular motion, and they founded Relay Therapeutics.
Elemento believes that Relay’s approach is highly beneficial in designing a better drug for bile duct cancer. “Relay Therapeutics has a cutting-edge approach for molecular dynamics that I don’t believe any other companies have, at least not as advanced.” Relay’s unique hardware and software allow simulations that could never be achieved through traditional experiments, Elemento says.
How it works
Relay used both experimental and computational approaches to design RLY-4008. The team started out by taking X-rays of crystallized versions of both their intended target, FGFR2, and the almost identical FGFR1. This enabled them to get a 3D snapshot of each of their structures. They then fed the X-rays into the Anton supercomputer to simulate how the proteins were likely to move.
Anton’s simulations showed that the FGFR1 protein had a flap that moved more frequently than FGFR2. Based on this distinct motion, the team tried to design a compound that would recognize this flap shifting around and bind to FGFR2 while steering away from its more active lookalike.
For that, they went back Anton, using the supercomputer to simulate the behavior of thousands of potential molecules for over a year, looking at what made a particular molecule selective to the target versus another molecule that wasn’t. These insights led them to determine the best compounds to make and test in the lab and, ultimately, they found that RLY-4008 was the most effective.
Promising results so far
Relay began phase 1-2 trials in 2020 and will continue until 2024. Preliminary results showed that, in the 17 patients taking a 70 mg dose of RLY-4008, the drug worked to shrink tumors in 88 percent of patients. This was a significant increase compared to other FGFR inhibitors. For instance, Futibatinib, which recently got FDA approval, had a response rate of only 42 percent.
Across all dose levels, RLY-4008 shrank tumors by 63 percent in 38 patients. In more good news, the drug didn’t elevate their phosphate levels, which suggests that it could be taken without increasing patients’ risk for kidney disease.
“Objectively, this is pretty remarkable,” says Elemento. “In a small patient study, you have a molecule that is able to shrink tumors in such a high fraction of patients. It is unusual to see such good results in a phase 1-2 trial.”
A simulated future
The research team is continuing to use molecular dynamic simulations to develop other new drug, such as one that is being studied in patients with solid tumors and breast cancer.
As for their bile duct cancer drug, RLY-4008, Relay plans by 2024 to have tested it in around 440 patients. “The mature results of the phase 1-2 trial are highly anticipated,” says Goyal, the principal investigator of the trial.
Sameek Roychowdhury, an oncologist and associate professor of internal medicine at Ohio State University, highlights the need for caution. “This has early signs of benefit, but we will look forward to seeing longer term results for benefit and side effect profiles. We need to think a few more steps ahead - these treatments are like the ’Whack-a-Mole game’ where cancer finds a way to become resistant to each subsequent drug.”
“I think the issue is going to be how durable are the responses to the drug and what are the mechanisms of resistance,” says Raymond Wadlow, an oncologist at the Inova Medical Group who specializes in gastrointestinal and haematological cancer. “But the results look promising. It is a much more selective inhibitor of the FGFR protein and less toxic. It’s been an exciting development.”