Health breakthroughs of 2022 that should have made bigger news

Nine experts break down the biggest biotech and health breakthroughs that didn't get the attention they deserved in 2022.
As the world has attempted to move on from COVID-19 in 2022, attention has returned to other areas of health and biotech with major regulatory approvals such as the Alzheimer's drug lecanemab – which can slow the destruction of brain cells in the early stages of the disease – being hailed by some as momentous breakthroughs.
This has been a year where psychedelic medicines have gained the attention of mainstream researchers with a groundbreaking clinical trial showing that psilocybin treatment can help relieve some of the symptoms of major depressive disorder. And with messenger RNA (mRNA) technology still very much capturing the imagination, the readouts of cancer vaccine trials have made headlines around the world.
But at the same time there have been vital advances which will likely go on to change medicine, and yet have slipped beneath the radar. I asked nine forward-thinking experts on health and biotech about the most important, but underappreciated, breakthrough of 2022.
Their descriptions, below, were lightly edited by Leaps.org for style and format.
New drug targets for Alzheimer’s disease

Professor Julie Williams, Director, Dementia Research Institute, Cardiff University
Genetics has changed our view of Alzheimer’s disease in the last five to six years. The beta amyloid hypothesis has dominated Alzheimer’s research for a long time, but there are multiple components to this complex disease, of which getting rid of amyloid plaques is one, but it is not the whole story. In April 2022, Nature published a paper which is the culmination of a decade’s worth of work - groups all over the world working together to identify 75 genes associated with risk of developing Alzheimer’s. This provides us with a roadmap for understanding the disease mechanisms.
For example, it is showing that there is something different about the immune systems of people who develop Alzheimer’s disease. There is something different about the way they process lipids in the brain, and very specific processes of how things travel through cells called endocytosis. When it comes to immunity, it indicates that the complement system is affecting whether synapses, which are the connections between neurons, get eliminated or not. In Alzheimer’s this process is more severe, so patients are losing more synapses, and this is correlated with cognition.
The genetics also implicates very specific tissues like microglia, which are the housekeepers in the brain. One of their functions is to clear away beta amyloid, but they also prune and nibble away at parts of the brain that are indicated to be diseased. If you have these risk genes, it seems that you are likely to prune more tissue, which may be part of the cell death and neurodegeneration that we observe in Alzheimer’s patients.
Genetics is telling us that we need to be looking at multiple causes of this complex disease, and we are doing that now. It is showing us that there are a number of different processes which combine to push patients into a disease state which results in the death of connections between nerve cells. These findings around the complement system and other immune-related mechanisms are very interesting as there are already drugs which are available for other diseases which could be repurposed in clinical trials. So it is really a turning point for us in the Alzheimer’s disease field.
Preventing Pandemics with Organ-Tissue Equivalents

Anthony Atala, Director of the Wake Forest Institute for Regenerative Medicine
COVID-19 has shown us that we need to be better prepared ahead of future pandemics and have systems in place where we can quickly catalogue a new virus and have an idea of which treatment agents would work best against it.
At Wake Forest Institute, our scientists have developed what we call organ-tissue equivalents. These are miniature tissues and organs, created using the same regenerative medicine technologies which we have been using to create tissues for patients. For example, if we are making a miniature liver, we will recreate this structure using the six different cell types you find in the liver, in the right proportions, and then the right extracellular matrix which holds the structure together. You're trying to replicate all the characteristics of the liver, but just in a miniature format.
We can now put these organ-tissue equivalents in a chip-like device, where we can expose them to different types of viral infections, and start to get a realistic idea of how the human body reacts to these viruses. We can use artificial intelligence and machine learning to map the pathways of the body’s response. This will allow us to catalogue known viruses far more effectively, and begin storing information on them.
Powering Deep Brain Stimulators with Breath

Islam Mosa, Co-Founder and CTO of VoltXon
Deep brain stimulation (DBS) devices are becoming increasingly common with 150,000 new devices being implanted every year for people with Parkinson’s disease, but also psychiatric conditions such as treatment-resistant depression and obsessive-compulsive disorders. But one of the biggest limitations is the power source – I call DBS devices energy monsters. While cardiac pacemakers use similar technology, their batteries last seven to ten years, but DBS batteries need changing every two to three years. This is because they are generating between 60-180 pulses per second.
Replacing the batteries requires surgery which costs a lot of money, and with every repeat operation comes a risk of infection, plus there is a lot of anxiety on behalf of the patient that the battery is running out.
My colleagues at the University of Connecticut and I, have developed a new way of charging these devices using the person’s own breathing movements, which would mean that the batteries never need to be changed. As the patient breathes in and out, their chest wall presses on a thin electric generator, which converts that movement into static electricity, charging a supercapacitor. This discharges the electricity required to power the DBS device and send the necessary pulses to the brain.
So far it has only been tested in a simulated pig, using a pig lung connected to a pump, but there are plans now to test it in a real animal, and then progress to clinical trials.
Smartwatches for Disease Detection
Jessilyn Dunn, Assistant Professor in Duke Biomedical Engineering
A group of researchers recently showed that digital biomarkers of infection can reveal when someone is sick, often before they feel sick. The team, which included Duke biomedical engineers, used information from smartwatches to detect Covid-19 cases five to 10 days earlier than diagnostic tests. Smartwatch data included aspects of heart rate, sleep quality and physical activity. Based on this data, we developed an algorithm to decide which people have the most need to take the diagnostic tests. With this approach, the percent of tests that come back positive are about four- to six-times higher, depending on which factors we monitor through the watches.
Our study was one of several showing the value of digital biomarkers, rather than a single blockbuster paper. With so many new ideas and technologies coming out around Covid, it’s hard to be that signal through the noise. More studies are needed, but this line of research is important because, rather than treat everyone as equally likely to have an infectious disease, we can use prior knowledge from smartwatches. With monkeypox, for example, you've got many more people who need to be tested than you have tests available. Information from the smartwatches enables you to improve how you allocate those tests.
Smartwatch data could also be applied to chronic diseases. For viruses, we’re looking for information about anomalies – a big change point in people’s health. For chronic diseases, it’s more like a slow, steady change. Our research lays the groundwork for the signals coming from smartwatches to be useful in a health setting, and now it’s up to us to detect more of these chronic cases. We want to go from the idea that we have this single change point, like a heart attack or stroke, and focus on the part before that, to see if we can detect it.
A Vaccine For RSV

Norbert Pardi, Vaccines Group Lead, Penn Institute for RNA Innovation, University of Pennsylvania
Scientists have long been trying to develop a vaccine for respiratory syncytial virus (RSV), and it looks like Pfizer are closing in on this goal, based on the latest clinical trial data in newborns which they released in November. Pfizer have developed a protein-based vaccine against the F protein of RSV, which they are giving to pregnant women. It turns out that it induces a robust immune response after the administration of a single shot and it seems to be highly protective in newborns. The efficacy was over 80% after 90 days, so it protected very well against severe disease, and even though this dropped a little after six month, it was still pretty high.
I think this has been a very important breakthrough, and very timely at the moment with both COVID-19, influenza and RSV circulating, which just shows the importance of having a vaccine which works well in both the very young and the very old.
The road to an RSV vaccine has also illustrated the importance of teamwork in 21st century vaccine development. You need people with different backgrounds to solve these challenges – microbiologists, immunologists and structural biologists working together to understand how viruses work, and how our immune system induces protective responses against certain viruses. It has been this kind of teamwork which has yielded the findings that targeting the prefusion stabilized form of the F protein in RSV induces much stronger and highly protective immune responses.
Gene therapy shows its potential

Nicole Paulk, Assistant Professor of Gene Therapy at the University of California, San Francisco
The recent US Food and Drug Administration (FDA) approval of Hemgenix, a gene therapy for hemophilia B, is big for a lot of reasons. While hemophilia is absolutely a rare disease, it is astronomically more common than the first two approvals – Luxturna for RPE65-meidated inherited retinal dystrophy and Zolgensma for spinal muscular atrophy - so many more patients will be treated with this. In terms of numbers of patients, we are now starting to creep up into things that are much more common, which is a huge step in terms of our ability to scale the production of an adeno-associated virus (AAV) vector for gene therapy.
Hemophilia is also a really special patient population because this has been the darling indication for AAV gene therapy for the last 20 to 30 years. AAV trafficks to the liver so well, it’s really easy for us to target the tissues that we want. If you look at the numbers, there have been more gene therapy scientists working on hemophilia than any other condition. There have just been thousands and thousands of us working on gene therapy indications for the last 20 or 30 years, so to see the first of these approvals make it, feels really special.
I am sure it is even more special for the patients because now they have a choice – do I want to stay on my recombinant factor drug that I need to take every day for the rest of my life, or right now I could get a one-time infusion of this virus and possibly experience curative levels of expression for the rest of my life. And this is just the first one for hemophilia, there’s going to end up being a dozen gene therapies within the next five years, targeted towards different hemophilias.
Every single approval is momentous for the entire field because it gets investors excited, it gets companies and physicians excited, and that helps speed things up. Right now, it's still a challenge to produce enough for double digit patients. But with more interest comes the experiments and trials that allow us to pick up the knowledge to scale things up, so that we can go after bigger diseases like diabetes, congestive heart failure, cancer, all of these much bigger afflictions.
Treating Thickened Hearts

John Spertus, Professor in Metabolic and Vascular Disease Research, UMKC School of Medicine
Hypertrophic cardiomyopathy (HCM) is a disease that causes your heart muscle to enlarge, and the walls of your heart chambers thicken and reduce in size. Because of this, they cannot hold as much blood and may stiffen, causing some sufferers to experience progressive shortness of breath, fatigue and ultimately heart failure.
So far we have only had very crude ways of treating it, using beta blockers, calcium channel blockers or other medications which cause the heart to beat less strongly. This works for some patients but a lot of time it does not, which means you have to consider removing part of the wall of the heart with surgery.
Earlier this year, a trial of a drug called mavacamten, became the first study to show positive results in treating HCM. What is remarkable about mavacamten is that it is directed at trying to block the overly vigorous contractile proteins in the heart, so it is a highly targeted, focused way of addressing the key problem in these patients. The study demonstrated a really large improvement in patient quality of life where they were on the drug, and when they went off the drug, the quality of life went away.
Some specialists are now hypothesizing that it may work for other cardiovascular diseases where the heart either beats too strongly or it does not relax well enough, but just having a treatment for HCM is a really big deal. For years we have not been very aggressive in identifying and treating these patients because there have not been great treatments available, so this could lead to a new era.
Regenerating Organs

David Andrijevic, Associate Research Scientist in neuroscience at Yale School of Medicine
As soon as the heartbeat stops, a whole chain of biochemical processes resulting from ischemia – the lack of blood flow, oxygen and nutrients – begins to destroy the body’s cells and organs. My colleagues and I at Yale School of Medicine have been investigating whether we can recover organs after prolonged ischemia, with the main goal of expanding the organ donor pool.
Earlier this year we published a paper in which we showed that we could use technology to restore blood circulation, other cellular functions and even heart activity in pigs, one hour after their deaths. This was done using a perfusion technology to substitute heart, lung and kidney function, and deliver an experimental cell protective fluid to these organs which aimed to stop cell death and aid in the recovery.
One of the aims of this technology is that it can be used in future to lengthen the time window for recovering organs for donation after a person has been declared dead, a logistical hurdle which would allow us to substantially increase the donor pool. We might also be able to use this cell protective fluid in studies to see if it can help people who have suffered from strokes and myocardial infarction. In future, if we managed to achieve an adequate brain recovery – and the brain, out of all the organs, is the most susceptible to ischemia – this might also change some paradigms in resuscitation medicine.
Antibody-Drug Conjugates for Cancer

Yosi Shamay, Cancer Nanomedicine and Nanoinformatics researcher at the Technion Israel Institute of Technology
For the past four or five years, antibody-drug conjugates (ADCs) - a cancer drug where you have an antibody conjugated to a toxin - have been used only in patients with specific cancers that display high expression of a target protein, for example HER2-positive breast cancer. But in 2022, there have been clinical trials where ADCs have shown remarkable results in patients with low expression of HER2, which is something we never expected to see.
In July 2022, AstraZeneca published the results of a clinical trial, which showed that an ADC called trastuzumab deruxtecan can offer a very big survival benefit to breast cancer patients with very little expression of HER2, levels so low that they would be borderline undetectable for a pathologist. They got a strong survival signal for patients with very aggressive, metastatic disease.
I think this is very interesting and important because it means that it might pave the way to include more patients in clinical trials looking at ADCs for other cancers, for example lymphoma, colon cancer, lung cancers, even if they have low expression of the protein target. It also holds implications for CAR-T cells - where you genetically engineer a T cell to attack the cancer - because the concept is very similar. If we now know that an ADC can have a survival benefit, even in patients with very low target expression, the same might be true for T cells.
Look back further: Breakthroughs of 2021
https://leaps.org/6-biotech-breakthroughs-of-2021-that-missed-the-attention-they-deserved/
Story by Big Think
We live in strange times, when the technology we depend on the most is also that which we fear the most. We celebrate cutting-edge achievements even as we recoil in fear at how they could be used to hurt us. From genetic engineering and AI to nuclear technology and nanobots, the list of awe-inspiring, fast-developing technologies is long.
However, this fear of the machine is not as new as it may seem. Technology has a longstanding alliance with power and the state. The dark side of human history can be told as a series of wars whose victors are often those with the most advanced technology. (There are exceptions, of course.) Science, and its technological offspring, follows the money.
This fear of the machine seems to be misplaced. The machine has no intent: only its maker does. The fear of the machine is, in essence, the fear we have of each other — of what we are capable of doing to one another.
How AI changes things
Sure, you would reply, but AI changes everything. With artificial intelligence, the machine itself will develop some sort of autonomy, however ill-defined. It will have a will of its own. And this will, if it reflects anything that seems human, will not be benevolent. With AI, the claim goes, the machine will somehow know what it must do to get rid of us. It will threaten us as a species.
Well, this fear is also not new. Mary Shelley wrote Frankenstein in 1818 to warn us of what science could do if it served the wrong calling. In the case of her novel, Dr. Frankenstein’s call was to win the battle against death — to reverse the course of nature. Granted, any cure of an illness interferes with the normal workings of nature, yet we are justly proud of having developed cures for our ailments, prolonging life and increasing its quality. Science can achieve nothing more noble. What messes things up is when the pursuit of good is confused with that of power. In this distorted scale, the more powerful the better. The ultimate goal is to be as powerful as gods — masters of time, of life and death.
Should countries create a World Mind Organization that controls the technologies that develop AI?
Back to AI, there is no doubt the technology will help us tremendously. We will have better medical diagnostics, better traffic control, better bridge designs, and better pedagogical animations to teach in the classroom and virtually. But we will also have better winnings in the stock market, better war strategies, and better soldiers and remote ways of killing. This grants real power to those who control the best technologies. It increases the take of the winners of wars — those fought with weapons, and those fought with money.
A story as old as civilization
The question is how to move forward. This is where things get interesting and complicated. We hear over and over again that there is an urgent need for safeguards, for controls and legislation to deal with the AI revolution. Great. But if these machines are essentially functioning in a semi-black box of self-teaching neural nets, how exactly are we going to make safeguards that are sure to remain effective? How are we to ensure that the AI, with its unlimited ability to gather data, will not come up with new ways to bypass our safeguards, the same way that people break into safes?
The second question is that of global control. As I wrote before, overseeing new technology is complex. Should countries create a World Mind Organization that controls the technologies that develop AI? If so, how do we organize this planet-wide governing board? Who should be a part of its governing structure? What mechanisms will ensure that governments and private companies do not secretly break the rules, especially when to do so would put the most advanced weapons in the hands of the rule breakers? They will need those, after all, if other actors break the rules as well.
As before, the countries with the best scientists and engineers will have a great advantage. A new international détente will emerge in the molds of the nuclear détente of the Cold War. Again, we will fear destructive technology falling into the wrong hands. This can happen easily. AI machines will not need to be built at an industrial scale, as nuclear capabilities were, and AI-based terrorism will be a force to reckon with.
So here we are, afraid of our own technology all over again.
What is missing from this picture? It continues to illustrate the same destructive pattern of greed and power that has defined so much of our civilization. The failure it shows is moral, and only we can change it. We define civilization by the accumulation of wealth, and this worldview is killing us. The project of civilization we invented has become self-cannibalizing. As long as we do not see this, and we keep on following the same route we have trodden for the past 10,000 years, it will be very hard to legislate the technology to come and to ensure such legislation is followed. Unless, of course, AI helps us become better humans, perhaps by teaching us how stupid we have been for so long. This sounds far-fetched, given who this AI will be serving. But one can always hope.
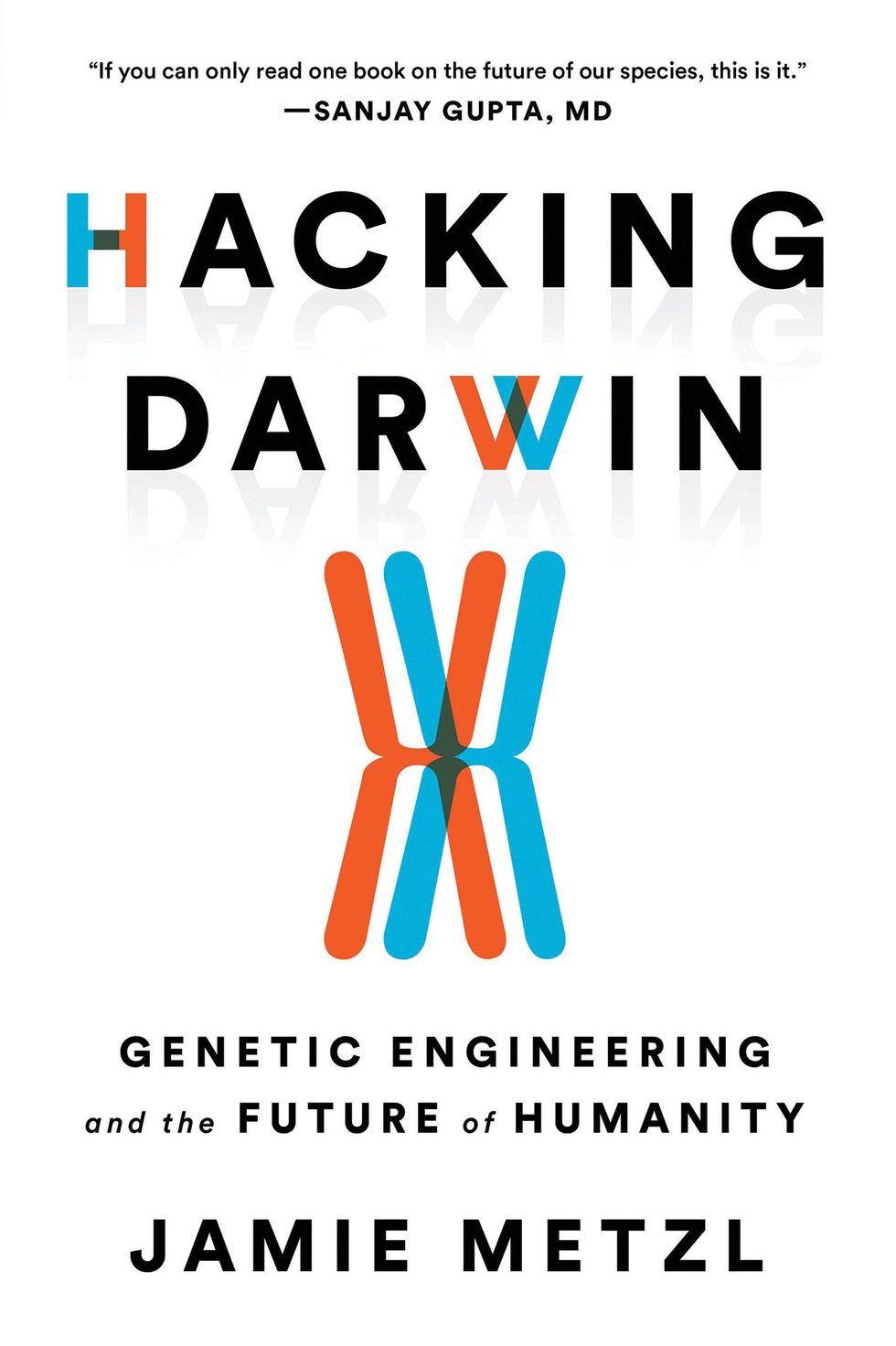
Interview with Jamie Metzl: We need a global OS upgrade
Jamie Metzl, author of Hacking Darwin, shares his views with Leaps.org on the future of genetics, tech, healthcare and more.
In this Q&A, leading technology and healthcare futurist Jamie Metzl discusses a range of topics and trend lines that will unfold over the next several decades: whether a version of Moore's Law applies to genetic technologies, the ethics of genetic engineering, the dangers of gene hacking, the end of sex, and much more.
Metzl is a member of the WHO expert advisory committee on human genome editing and the bestselling author of Hacking Darwin.
The conversation was lightly edited by Leaps.org for style and length.
In Hacking Darwin, you describe how we may modify the human body with CRISPR technologies, initially to obtain unsurpassed sports performance and then to enhance other human characteristics. What would such power over human biology mean for the future of our civilization?
After nearly four billion years of evolution, our one species suddenly has the increasing ability to read, write, and hack the code of life. This will have massive implications across the board, including in human health and reproduction, plant and animal agriculture, energy and advanced materials, and data storage and computing, just to name a few. My book Hacking Darwin: Genetic Engineering and the Future of Humanity primarly explored how we are currently deploying and will increasingly use our capabilities to transform human life in novel ways. My next book, The Great Biohack: Recasting Life in an Age of Revolutionary Technology, coming out in May 2024, will examine the broader implications for all of life on Earth.
We humans will, over time, use these technologies on ourselves to solve problems and eventually to enhance our capabilities. We need to be extremely conservative, cautious, and careful in doing so, but doing so will almost certainly be part of our future as a species.
In electronics, Moore's law is an established theory that computing power doubles every 18 months. Is there any parallel to be drawn with genetic technologies?
The increase in speed and decrease in costs of genome sequencing have progressed far faster than Moore’s law. It took thirteen years and cost about a billion dollars to sequence the first human genome. Today it takes just a few hours and can cost as little as a hundred dollars to do a far better job. In 2012, Jennifer Doudna and Emmanuel Charpentier published the basic science paper outlining the CRISPR-cas9 genome editing tool that would eventually win them the Nobel prize. Only six years later, the first CRISPR babies were born in China. If it feels like technology is moving ever-faster, that’s because it is.
Let's turn to the topic of aging. Do you think that the field of genetics will advance fast enough to eventually increase maximal lifespan for a child born this year? How about for a person who is currently age 50?
The science of aging is definitely real, but that doesn’t mean we will live forever. Aging is a biological process subject to human manipulation. Decades of animal research shows that. This does not mean we will live forever, but it does me we will be able to do more to expand our healthspans, the period of our lives where we are able to live most vigorously.
The first thing we need to do is make sure everyone on earth has access to the resources necessary to live up to their potential. I live in New York City, and I can take a ten minute subway ride to a neighborhood where the average lifespan is over a decade shorter than in mine. This is true within societies and between countries as well. Secondly, we all can live more like people in the Blue Zones, parts of the world where people live longer, on average, than the rest of us. They get regular exercise, eat healthy foods, have strong social connections, etc. Finally, we will all benefit, over time, from more scientific interventions to extend our healthspan. This may include small molecule drugs like metformin, rapamycin, and NAD+ boosters, blood serum infusions, and many other things.
Science fiction has depicted a future where we will never get sick again, stay young longer or become immortal. Assuming that any of this is remotely possible, should we be afraid of such changes, even if they seem positive in some regards, because we can’t understand the full implications at this point?
Not all of these promises will be realized in full, but we will use these technologies to help us live healthier, longer lives. We will never become immortal becasue nothing lasts forever. We will always get sick, even if the balance of diseases we face shifts over time, as it has always done. It is healthy, and absolutely necessary, that we feel both hope and fear about this future. If we only feel hope, we will blind ourselves to the very real potential downsides. If we only feel fear, we will deny ourselves the very meaningful benefits these technologies have the potential to provide.
A fascinating chapter in Hacking Darwin is entitled The End of Sex. And you see that as a good thing?
We humans will always be a sexually reproducing species, it’s just that we’ll reproduce increasingly less through the physical act of sex. We’re already seeing this with IVF. As the benefits of technology assisted reproduction increase relative to reproduction through the act of sex, many people will come to see assisted reproduction as a better way to reduce risk and, over time, possibly increase benefits. We’ll still have sex for all the other wonderful reasons we have it today, just less for reproduction. There will always be a critical place in our world for Italian romantics!
What are dangers of genetic hackers, perhaps especially if everyone’s DNA is eventually transcribed for medical purposes and available on the internet and in the cloud?
The sky is really the limit for how we can use gentic technologies to do things we may want, and the sky is also the limit for potential harms. It’s quite easy to imagine scenarios in which malevolent actors create synthetic pathogens designed to wreak havoc, or where people steal and abuse other people’s genetic information. It wouldn’t even need to be malevolent actors. Even well-intentioned researchers making unintended mistakes could cause real harm, as we may have seen with COVID-19 if, as appears likely to me, the pandemic stems for a research related incident]. That’s why we need strong governance and regulatory systems to optimize benefits and minimize potential harms. I was honored to have served on the World Health Organization Expert Advisory Committee on Human Genome Editing, were we developed a proposed framework for how this might best be achieved.
You foresee the equivalent of a genetic arms race between the world's most powerful countries. In what sense are genetic technologies similar to weapons?
Genetic technologies could be used to create incredibly powerful bioweapons or to build gene drives with the potential to crash entire ecosystems. That’s why thoughtful regulation is in order. Because the benefits of mastering and deploying these technologies are so great, there’s also a real danger of a genetics arms race. This could be extremely dangerous and will need to be prevented.
In your book, you express concern that states lacking Western conceptions of human rights are especially prone to misusing the science of genetics. Does this same concern apply to private companies? How much can we trust them to control and wield these technologies?
This is a conversation about science and technology but it’s really a conversation about values. If we don’t agree on what core values should be promoted, it will be nearly impossible to agree on what actions do and do not make sense. We need norms, laws, and values frameworks that apply to everyone, including governments, corporations, researchers, healthcare providers, DiY bio hobbyists, and everyone else.
We have co-evolved with our technology for a very long time. Many of our deepest beliefs have formed in that context and will continue to do so. But as we take for ourselves the powers we have attributed to our various gods, many of these beliefs will be challenged. We can not and must not jettison our beliefs in the face of technology, and must instead make sure our most cherished values guide the application of our most powerful technologies.
A conversation on international norms is in full swing in the field of AI, prompted by the release of ChatGPT4 earlier this year. Are there ways in which it’s inefficient, shortsighted or otherwise problematic for these discussions on gene technologies, AI and other advances to be occurring in silos? In addition to more specific guidelines, is there something to be gained from developing a universal set of norms and values that applies more broadly to all innovation?
AI is yet another technology where the potential to do great good is tied to the potential to inflict signifcant harm. It makes no sense that we tend to treat each technology on its own rather than looking at the entire category of challenges. For sure, we need to very rapidly ramp up our efforts with regard to AI norm-setting, regulations, and governance at all levels. But just doing that will be kind of like generating a flu vaccine for each individual flu strain. Far better to build a universal flu vaccine addressing common elements of all flu viruses of concern.
That’s why we also need to be far more deliberate in both building a global operating systems based around the mutual responsibilities of our global interdependence and, under that umbrella, a broader system for helping us govern and regulate revolutionary technologies. Such a process might begin with a large international conference, the equivalent of Rio 1992 for climate change, but then quickly work to establish and share best practices, help build parallel institutions in all countries so people and governamts can talk with each other, and do everything possible to maximize benefits and minimize risks at all levels in an ongoing and dynamic way.
At what point might genetic enhancements lead to a reclassfication of modified humans as another species?
We’ll still all be fellow humans for a very, very long time. We already have lots of variation between us. That is the essence of biology. Will some humans, at some point in the future, leave Earth and spend generations elsewhere? I believe so. In those new environments, humans will evolve, over time, differently than those if us who remain on this planet? This may sound like science fiction, but the sci-fi future is coming at us faster than most people realize.
Is the concept of human being changing?
Yes. It always has and always will.
Another big question raised in your book: what limits should we impose on the freedom to manipulate genetics?
Different societies will come to different conclusion on this critical question. I am sympathetic to the argument that people should have lots of say over their own bodies, which why I support abortion rights even though I recognize that an abortion can be a violent procedure. But it would be insane and self-defeating to say that individuals have an unlimited right to manipulate their own or their future children’s heritable genetics. The future of human life is all of our concern and must be regulated, albeit wisely.
In some cases, such as when we have the ability to prevent a deadly genetic disroder, it might be highly ethical to manipulate other human beings. In other circumstances, the genetic engineering of humans might be highly unethical. The key point is to avoid asking this question in a binary manner. We need to weigh the costs and benefits of each type of intervention. We need societal and global infrastrucutres to do that well. We don’t yet have those but we need them badly.
Can you tell us more about your next book?
The Great Biohack: Recasting Lifee in an Age of Revolutionary Technology, will come out in May 2024. It explores what the intersecting AI, genetics, and biotechnology revolutions will mean for the future of life on earth, including our healthcare, agriculture, industry, computing, and everything else. We are at a transitional moment for life on earth, equivalent to the dawn of agriculture, electricity, and industrialization. The key differentiator between better and worse outcomes is what we do today, at this early stage of this new transformation. The book describes what’s happening, what’s at stake, and what we each and all can and, frankly, must do to build the type of future we’d like to inhabit.
You’ve been a leader of international efforts calling for a full investigation into COVID-19 origins and are the founder of the global movement OneShared.World. What problem are you trying to solve through OneShared.World?
The biggest challenge we face today is the mismatch between the nature of our biggest problems, global and common, and the absence of a sufficient framework for addressing that entire category of challenges. The totally avoidable COVID-19 pandemic is one example of the extremet costs of the status quo. OneShared.World is our effort to fight for an upgrade in our world’s global operating system, based around the mutual responsibilities of interdependence. We’ve had global OS upgrades before after the Thirty Years War and after World War II, but wouldn’t it be better to make the necessary changes now to prevent a crisis of that level stemming from a nuclear war, ecosystem collapse, or deadlier synthetic biology pandemic rather than waiting until after? Revolutionary science is a global issue that must be wisely managed at every level if it is to be wisely managed at all.
How do we ensure that revolutionary technologies benefit humanity instead of undermining it?
That is the essential question. It’s why I’ve written Hacking Darwin, am writing The Great Biohack, and doing the rest of my work. If we want scietific revolutions to help, rather than hurt, us, we must all play a role building that future. This isn’t just a conversation about science, it’s about how we can draw on our most cherished values to guide the optimal development of science and technology for the common good. That must be everyone’s business.
Portions of this interview were first published in Grassia (Italy) and Zen Portugal.
Jamie Metzl is one of the world’s leading technology and healthcare futurists and author of the bestselling book, Hacking Darwin: Genetic Engineering and the Future of Humanity, which has been translated into 15 languages. In 2019, he was appointed to the World Health Organization expert advisory committee on human genome editing. Jamie is a faculty member of Singularity University and NextMed Health, a Senior Fellow of the Atlantic Council, and Founder and Chair of the global social movement, OneShared.World.
Called “the original COVID-19 whistleblower,” his pioneering role advocating for a full investigation into the origins of the COVID-19 pandemic has been featured in 60 Minutes, the New York Times, and most major media across the globe, and he was the lead witness in the first congressional hearings on this topic. Jamie previously served in the U.S. National Security Council, State Department, and Senate Foreign Relations Committee and with the United Nations in Cambodia. Jamie appears regularly on national and international media and his syndicated columns and other writing in science, technology, and global affairs are featured in publications around the world.
Jamie sits on advisory boards for multiple biotechnology and other companies and is Special Strategist to the WisdomTree BioRevolution Exchange Traded Fund. In addition to Hacking Darwin, he is author of a history of the Cambodian genocide, the historical novel The Depths of the Sea, and the genetics sci-fi thrillers Genesis Code and Eternal Sonata. His next book, The Great Biohack: Recasting Life in an age of Revolutionary Technology, will be published by Hachette in May 2024. Jamie holds a Ph.D. from Oxford, a law degree from Harvard, and an undergraduate degree from Brown and is an avid ironman triathlete and ultramarathon runner.