Health breakthroughs of 2022 that should have made bigger news

Nine experts break down the biggest biotech and health breakthroughs that didn't get the attention they deserved in 2022.
As the world has attempted to move on from COVID-19 in 2022, attention has returned to other areas of health and biotech with major regulatory approvals such as the Alzheimer's drug lecanemab – which can slow the destruction of brain cells in the early stages of the disease – being hailed by some as momentous breakthroughs.
This has been a year where psychedelic medicines have gained the attention of mainstream researchers with a groundbreaking clinical trial showing that psilocybin treatment can help relieve some of the symptoms of major depressive disorder. And with messenger RNA (mRNA) technology still very much capturing the imagination, the readouts of cancer vaccine trials have made headlines around the world.
But at the same time there have been vital advances which will likely go on to change medicine, and yet have slipped beneath the radar. I asked nine forward-thinking experts on health and biotech about the most important, but underappreciated, breakthrough of 2022.
Their descriptions, below, were lightly edited by Leaps.org for style and format.
New drug targets for Alzheimer’s disease

Professor Julie Williams, Director, Dementia Research Institute, Cardiff University
Genetics has changed our view of Alzheimer’s disease in the last five to six years. The beta amyloid hypothesis has dominated Alzheimer’s research for a long time, but there are multiple components to this complex disease, of which getting rid of amyloid plaques is one, but it is not the whole story. In April 2022, Nature published a paper which is the culmination of a decade’s worth of work - groups all over the world working together to identify 75 genes associated with risk of developing Alzheimer’s. This provides us with a roadmap for understanding the disease mechanisms.
For example, it is showing that there is something different about the immune systems of people who develop Alzheimer’s disease. There is something different about the way they process lipids in the brain, and very specific processes of how things travel through cells called endocytosis. When it comes to immunity, it indicates that the complement system is affecting whether synapses, which are the connections between neurons, get eliminated or not. In Alzheimer’s this process is more severe, so patients are losing more synapses, and this is correlated with cognition.
The genetics also implicates very specific tissues like microglia, which are the housekeepers in the brain. One of their functions is to clear away beta amyloid, but they also prune and nibble away at parts of the brain that are indicated to be diseased. If you have these risk genes, it seems that you are likely to prune more tissue, which may be part of the cell death and neurodegeneration that we observe in Alzheimer’s patients.
Genetics is telling us that we need to be looking at multiple causes of this complex disease, and we are doing that now. It is showing us that there are a number of different processes which combine to push patients into a disease state which results in the death of connections between nerve cells. These findings around the complement system and other immune-related mechanisms are very interesting as there are already drugs which are available for other diseases which could be repurposed in clinical trials. So it is really a turning point for us in the Alzheimer’s disease field.
Preventing Pandemics with Organ-Tissue Equivalents

Anthony Atala, Director of the Wake Forest Institute for Regenerative Medicine
COVID-19 has shown us that we need to be better prepared ahead of future pandemics and have systems in place where we can quickly catalogue a new virus and have an idea of which treatment agents would work best against it.
At Wake Forest Institute, our scientists have developed what we call organ-tissue equivalents. These are miniature tissues and organs, created using the same regenerative medicine technologies which we have been using to create tissues for patients. For example, if we are making a miniature liver, we will recreate this structure using the six different cell types you find in the liver, in the right proportions, and then the right extracellular matrix which holds the structure together. You're trying to replicate all the characteristics of the liver, but just in a miniature format.
We can now put these organ-tissue equivalents in a chip-like device, where we can expose them to different types of viral infections, and start to get a realistic idea of how the human body reacts to these viruses. We can use artificial intelligence and machine learning to map the pathways of the body’s response. This will allow us to catalogue known viruses far more effectively, and begin storing information on them.
Powering Deep Brain Stimulators with Breath

Islam Mosa, Co-Founder and CTO of VoltXon
Deep brain stimulation (DBS) devices are becoming increasingly common with 150,000 new devices being implanted every year for people with Parkinson’s disease, but also psychiatric conditions such as treatment-resistant depression and obsessive-compulsive disorders. But one of the biggest limitations is the power source – I call DBS devices energy monsters. While cardiac pacemakers use similar technology, their batteries last seven to ten years, but DBS batteries need changing every two to three years. This is because they are generating between 60-180 pulses per second.
Replacing the batteries requires surgery which costs a lot of money, and with every repeat operation comes a risk of infection, plus there is a lot of anxiety on behalf of the patient that the battery is running out.
My colleagues at the University of Connecticut and I, have developed a new way of charging these devices using the person’s own breathing movements, which would mean that the batteries never need to be changed. As the patient breathes in and out, their chest wall presses on a thin electric generator, which converts that movement into static electricity, charging a supercapacitor. This discharges the electricity required to power the DBS device and send the necessary pulses to the brain.
So far it has only been tested in a simulated pig, using a pig lung connected to a pump, but there are plans now to test it in a real animal, and then progress to clinical trials.
Smartwatches for Disease Detection
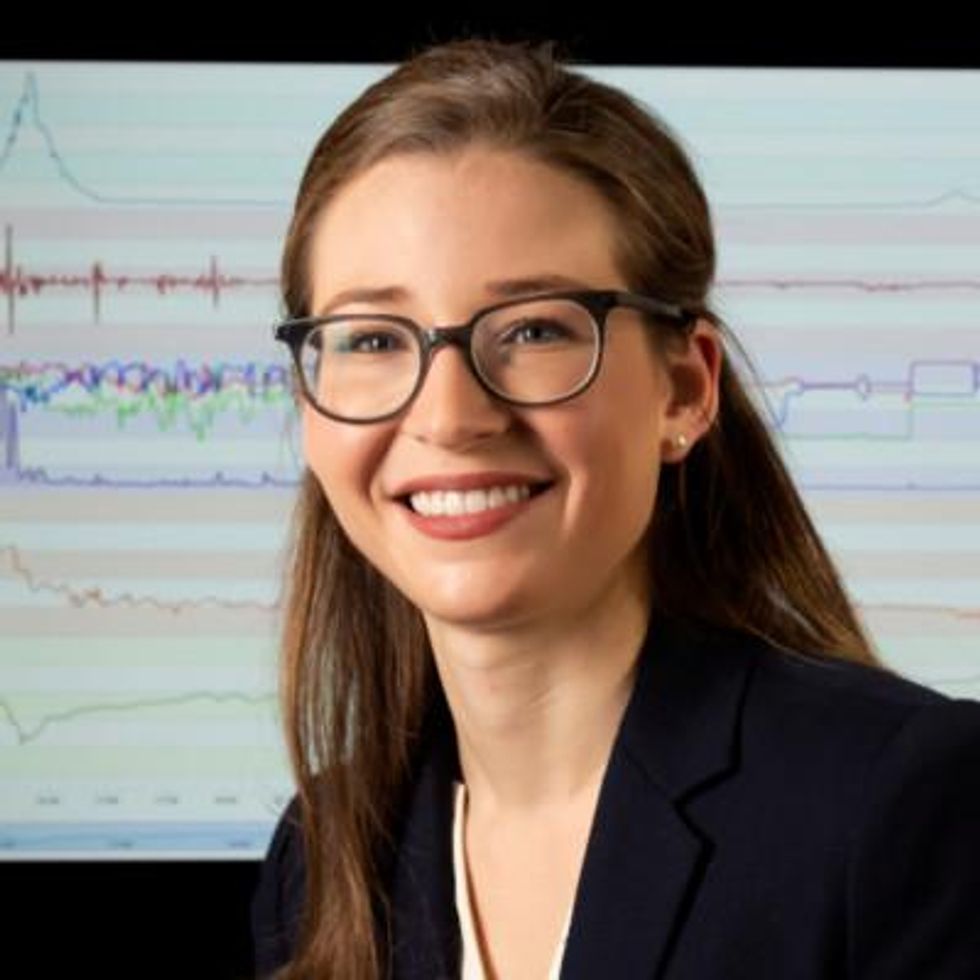
Jessilyn Dunn, Assistant Professor in Duke Biomedical Engineering
A group of researchers recently showed that digital biomarkers of infection can reveal when someone is sick, often before they feel sick. The team, which included Duke biomedical engineers, used information from smartwatches to detect Covid-19 cases five to 10 days earlier than diagnostic tests. Smartwatch data included aspects of heart rate, sleep quality and physical activity. Based on this data, we developed an algorithm to decide which people have the most need to take the diagnostic tests. With this approach, the percent of tests that come back positive are about four- to six-times higher, depending on which factors we monitor through the watches.
Our study was one of several showing the value of digital biomarkers, rather than a single blockbuster paper. With so many new ideas and technologies coming out around Covid, it’s hard to be that signal through the noise. More studies are needed, but this line of research is important because, rather than treat everyone as equally likely to have an infectious disease, we can use prior knowledge from smartwatches. With monkeypox, for example, you've got many more people who need to be tested than you have tests available. Information from the smartwatches enables you to improve how you allocate those tests.
Smartwatch data could also be applied to chronic diseases. For viruses, we’re looking for information about anomalies – a big change point in people’s health. For chronic diseases, it’s more like a slow, steady change. Our research lays the groundwork for the signals coming from smartwatches to be useful in a health setting, and now it’s up to us to detect more of these chronic cases. We want to go from the idea that we have this single change point, like a heart attack or stroke, and focus on the part before that, to see if we can detect it.
A Vaccine For RSV

Norbert Pardi, Vaccines Group Lead, Penn Institute for RNA Innovation, University of Pennsylvania
Scientists have long been trying to develop a vaccine for respiratory syncytial virus (RSV), and it looks like Pfizer are closing in on this goal, based on the latest clinical trial data in newborns which they released in November. Pfizer have developed a protein-based vaccine against the F protein of RSV, which they are giving to pregnant women. It turns out that it induces a robust immune response after the administration of a single shot and it seems to be highly protective in newborns. The efficacy was over 80% after 90 days, so it protected very well against severe disease, and even though this dropped a little after six month, it was still pretty high.
I think this has been a very important breakthrough, and very timely at the moment with both COVID-19, influenza and RSV circulating, which just shows the importance of having a vaccine which works well in both the very young and the very old.
The road to an RSV vaccine has also illustrated the importance of teamwork in 21st century vaccine development. You need people with different backgrounds to solve these challenges – microbiologists, immunologists and structural biologists working together to understand how viruses work, and how our immune system induces protective responses against certain viruses. It has been this kind of teamwork which has yielded the findings that targeting the prefusion stabilized form of the F protein in RSV induces much stronger and highly protective immune responses.
Gene therapy shows its potential

Nicole Paulk, Assistant Professor of Gene Therapy at the University of California, San Francisco
The recent US Food and Drug Administration (FDA) approval of Hemgenix, a gene therapy for hemophilia B, is big for a lot of reasons. While hemophilia is absolutely a rare disease, it is astronomically more common than the first two approvals – Luxturna for RPE65-meidated inherited retinal dystrophy and Zolgensma for spinal muscular atrophy - so many more patients will be treated with this. In terms of numbers of patients, we are now starting to creep up into things that are much more common, which is a huge step in terms of our ability to scale the production of an adeno-associated virus (AAV) vector for gene therapy.
Hemophilia is also a really special patient population because this has been the darling indication for AAV gene therapy for the last 20 to 30 years. AAV trafficks to the liver so well, it’s really easy for us to target the tissues that we want. If you look at the numbers, there have been more gene therapy scientists working on hemophilia than any other condition. There have just been thousands and thousands of us working on gene therapy indications for the last 20 or 30 years, so to see the first of these approvals make it, feels really special.
I am sure it is even more special for the patients because now they have a choice – do I want to stay on my recombinant factor drug that I need to take every day for the rest of my life, or right now I could get a one-time infusion of this virus and possibly experience curative levels of expression for the rest of my life. And this is just the first one for hemophilia, there’s going to end up being a dozen gene therapies within the next five years, targeted towards different hemophilias.
Every single approval is momentous for the entire field because it gets investors excited, it gets companies and physicians excited, and that helps speed things up. Right now, it's still a challenge to produce enough for double digit patients. But with more interest comes the experiments and trials that allow us to pick up the knowledge to scale things up, so that we can go after bigger diseases like diabetes, congestive heart failure, cancer, all of these much bigger afflictions.
Treating Thickened Hearts

John Spertus, Professor in Metabolic and Vascular Disease Research, UMKC School of Medicine
Hypertrophic cardiomyopathy (HCM) is a disease that causes your heart muscle to enlarge, and the walls of your heart chambers thicken and reduce in size. Because of this, they cannot hold as much blood and may stiffen, causing some sufferers to experience progressive shortness of breath, fatigue and ultimately heart failure.
So far we have only had very crude ways of treating it, using beta blockers, calcium channel blockers or other medications which cause the heart to beat less strongly. This works for some patients but a lot of time it does not, which means you have to consider removing part of the wall of the heart with surgery.
Earlier this year, a trial of a drug called mavacamten, became the first study to show positive results in treating HCM. What is remarkable about mavacamten is that it is directed at trying to block the overly vigorous contractile proteins in the heart, so it is a highly targeted, focused way of addressing the key problem in these patients. The study demonstrated a really large improvement in patient quality of life where they were on the drug, and when they went off the drug, the quality of life went away.
Some specialists are now hypothesizing that it may work for other cardiovascular diseases where the heart either beats too strongly or it does not relax well enough, but just having a treatment for HCM is a really big deal. For years we have not been very aggressive in identifying and treating these patients because there have not been great treatments available, so this could lead to a new era.
Regenerating Organs

David Andrijevic, Associate Research Scientist in neuroscience at Yale School of Medicine
As soon as the heartbeat stops, a whole chain of biochemical processes resulting from ischemia – the lack of blood flow, oxygen and nutrients – begins to destroy the body’s cells and organs. My colleagues and I at Yale School of Medicine have been investigating whether we can recover organs after prolonged ischemia, with the main goal of expanding the organ donor pool.
Earlier this year we published a paper in which we showed that we could use technology to restore blood circulation, other cellular functions and even heart activity in pigs, one hour after their deaths. This was done using a perfusion technology to substitute heart, lung and kidney function, and deliver an experimental cell protective fluid to these organs which aimed to stop cell death and aid in the recovery.
One of the aims of this technology is that it can be used in future to lengthen the time window for recovering organs for donation after a person has been declared dead, a logistical hurdle which would allow us to substantially increase the donor pool. We might also be able to use this cell protective fluid in studies to see if it can help people who have suffered from strokes and myocardial infarction. In future, if we managed to achieve an adequate brain recovery – and the brain, out of all the organs, is the most susceptible to ischemia – this might also change some paradigms in resuscitation medicine.
Antibody-Drug Conjugates for Cancer

Yosi Shamay, Cancer Nanomedicine and Nanoinformatics researcher at the Technion Israel Institute of Technology
For the past four or five years, antibody-drug conjugates (ADCs) - a cancer drug where you have an antibody conjugated to a toxin - have been used only in patients with specific cancers that display high expression of a target protein, for example HER2-positive breast cancer. But in 2022, there have been clinical trials where ADCs have shown remarkable results in patients with low expression of HER2, which is something we never expected to see.
In July 2022, AstraZeneca published the results of a clinical trial, which showed that an ADC called trastuzumab deruxtecan can offer a very big survival benefit to breast cancer patients with very little expression of HER2, levels so low that they would be borderline undetectable for a pathologist. They got a strong survival signal for patients with very aggressive, metastatic disease.
I think this is very interesting and important because it means that it might pave the way to include more patients in clinical trials looking at ADCs for other cancers, for example lymphoma, colon cancer, lung cancers, even if they have low expression of the protein target. It also holds implications for CAR-T cells - where you genetically engineer a T cell to attack the cancer - because the concept is very similar. If we now know that an ADC can have a survival benefit, even in patients with very low target expression, the same might be true for T cells.
Look back further: Breakthroughs of 2021
https://leaps.org/6-biotech-breakthroughs-of-2021-that-missed-the-attention-they-deserved/
The U.S. must fund more biotech innovation – or other countries will catch up faster than you think
In the coming years, U.S. market share in biotech will decline unless the federal government makes investments to improve the quality and quantity of U.S. research, writes the author.
The U.S. has approximately 58 percent of the market share in the biotech sector, followed by China with 11 percent. However, this market share is the result of several years of previous research and development (R&D) – it is a present picture of what happened in the past. In the future, this market share will decline unless the federal government makes investments to improve the quality and quantity of U.S. research in biotech.
The effectiveness of current R&D can be evaluated in a variety of ways such as monies invested and the number of patents filed. According to the UNESCO Institute for Statistics, the U.S. spends approximately 2.7 percent of GDP on R&D ($476,459.0M), whereas China spends 2 percent ($346,266.3M). However, investment levels do not necessarily translate into goods that end up contributing to innovation.
Patents are a better indication of innovation. The biotech industry relies on patents to protect their investments, making patenting a key tool in the process of translating scientific discoveries that can ultimately benefit patients. In 2020, China filed 1,497,159 patents, a 6.9 percent increase in growth rate. In contrast, the U.S. filed 597,172, a 3.9 percent decline. When it comes to patents filed, China has approximately 45 percent of the world share compared to 18 percent for the U.S.
So how did we get here? The nature of science in academia allows scientists to specialize by dedicating several years to advance discovery research and develop new inventions that can then be licensed by biotech companies. This makes academic science critical to innovation in the U.S. and abroad.
Academic scientists rely on government and foundation grants to pay for R&D, which includes salaries for faculty, investigators and trainees, as well as monies for infrastructure, support personnel and research supplies. Of particular interest to academic scientists to cover these costs is government support such as Research Project Grants, also known as R01 grants, the oldest grant mechanism from the National Institutes of Health. Unfortunately, this funding mechanism is extremely competitive, as applications have a success rate of only about 20 percent. To maximize the chances of getting funded, investigators tend to limit the innovation of their applications, since a project that seems overambitious is discouraged by grant reviewers.
Considering the difficulty in obtaining funding, the limited number of opportunities for scientists to become independent investigators capable of leading their own scientific projects, and the salaries available to pay for scientists with a doctoral degree, it is not surprising that the U.S. is progressively losing its workforce for innovation.
This approach affects the future success of the R&D enterprise in the U.S. Pursuing less innovative work tends to produce scientific results that are more obvious than groundbreaking, and when a discovery is obvious, it cannot be patented, resulting in fewer inventions that go on to benefit patients. Even though there are governmental funding options available for scientists in academia focused on more groundbreaking and translational projects, those options are less coveted by academic scientists who are trying to obtain tenure and long-term funding to cover salaries and other associated laboratory expenses. Therefore, since only a small percent of projects gets funded, the likelihood of scientists interested in pursuing academic science or even research in general keeps declining over time.
Efforts to raise the number of individuals who pursue a scientific education are paying off. However, the number of job openings for those trainees to carry out independent scientific research once they graduate has proved harder to increase. These limitations are not just in the number of faculty openings to pursue academic science, which are in part related to grant funding, but also the low salary available to pay those scientists after they obtain their doctoral degree, which ranges from $53,000 to $65,000, depending on years of experience.
Thus, considering the difficulty in obtaining funding, the limited number of opportunities for scientists to become independent investigators capable of leading their own scientific projects, and the salaries available to pay for scientists with a doctoral degree, it is not surprising that the U.S. is progressively losing its workforce for innovation, which results in fewer patents filed.
Perhaps instead of encouraging scientists to propose less innovative projects in order to increase their chances of getting grants, the U.S. government should give serious consideration to funding investigators for their potential for success -- or the success they have already achieved in contributing to the advancement of science. Such a funding approach should be tiered depending on career stage or years of experience, considering that 42 years old is the median age at which the first R01 is obtained. This suggests that after finishing their training, scientists spend 10 years before they establish themselves as independent academic investigators capable of having the appropriate funds to train the next generation of scientists who will help the U.S. maintain or even expand its market share in the biotech industry for years to come. Patenting should be given more weight as part of the academic endeavor for promotion purposes, or governmental investment in research funding should be increased to support more than just 20 percent of projects.
Remaining at the forefront of biotech innovation will give us the opportunity to not just generate more jobs, but it will also allow us to attract the brightest scientists from all over the world. This talented workforce will go on to train future U.S. scientists and will improve our standard of living by giving us the opportunity to produce the next generation of therapies intended to improve human health.
This problem cannot rely on just one solution, but what is certain is that unless there are more creative changes in funding approaches for scientists in academia, eventually we may be saying “remember when the U.S. was at the forefront of biotech innovation?”
New gene therapy helps patients with rare disease. One mother wouldn't have it any other way.
A biotech in Cambridge, Mass., is targeting a rare disease called cystinosis with gene therapy. It's been effective for five patients in a clinical trial that's still underway.
Three years ago, Jordan Janz of Consort, Alberta, knew his gene therapy treatment for cystinosis was working when his hair started to darken. Pigmentation or melanin production is just one part of the body damaged by cystinosis.
“When you have cystinosis, you’re either a redhead or a blonde, and you are very pale,” attests Janz, 23, who was diagnosed with the disease just eight months after he was born. “After I got my new stem cells, my hair came back dark, dirty blonde, then it lightened a little bit, but before it was white blonde, almost bleach blonde.”
According to Cystinosis United, about 500 to 600 people have the rare genetic disease in the U.S.; an estimated 20 new cases are diagnosed each year.
Located in Cambridge, Mass., AVROBIO is a gene therapy company that targets cystinosis and other lysosomal storage disorders, in which toxic materials build up in the cells. Janz is one of five patients in AVROBIO’s ongoing Phase 1/2 clinical trial of a gene therapy for cystinosis called AVR-RD-04.
Recently, AVROBIO compiled positive clinical data from this first and only gene therapy trial for the disease. The data show the potential of the therapy to genetically modify the patients’ own hematopoietic stem cells—a certain type of cell that’s capable of developing into all different types of blood cells—to express the functional protein they are deficient in. It stabilizes or reduces the impact of cystinosis on multiple tissues with a single dose.
Medical researchers have found that more than 80 different mutations to a gene called CTNS are responsible for causing cystinosis. The most common mutation results in a deficiency of the protein cystinosin. That protein functions as a transporter that regulates a lot metabolic processes in the cells.
“One of the first things we see in patients clinically is an accumulation of a particular amino acid called cystine, which grows toxic cystine crystals in the cells that cause serious complications,” explains Essra Rihda, chief medical officer for AVROBIO. “That happens in the cells across the tissues and organs of the body, so the disease affects many parts of the body.”

Jordan Janz, 23, meets Stephanie Cherqui, the principal investigator of his gene therapy trial, before the trial started in 2019.
Jordan Janz
According to Rihda, although cystinosis can occur in kids and adults, the most severe form of the disease affects infants and makes up about 95 percent of overall cases. Children typically appear healthy at birth, but around six to 18 months, they start to present for medical attention with failure to thrive.
Additionally, infants with cystinosis often urinate frequently, a sign of polyuria, and they are thirsty all the time, since the disease usually starts in the kidneys. Many develop chronic kidney disease that ultimately progresses to the point where the kidney no longer supports the body’s needs. At that stage, dialysis is required and then a transplant. From there the disease spreads to many other organs, including the eyes, muscles, heart, nervous system, etc.
“The gene for cystinosis is expressed in every single tissue we have, and the accumulation of this toxic buildup alters all of the organs of the patient, so little by little all of the organs start to fail,” says Stephanie Cherqui, principal investigator of Cherqui Lab, which is part of UC San Diego’s Department of Pediatrics.
Since the 1950s, a drug called cysteamine showed some therapeutic effect on cystinosis. It was approved by the FDA in 1994 to prevent damage that may be caused by the buildup of cystine crystals in organs. Prior to FDA approval, Cherqui says, children were dying of the disease before they were ten-years-old or after a kidney transplant. By taking oral cysteamine, they can live from 20 to 50 years longer. But it’s a challenging drug because it has to be taken every 6 or 12 hours, and there are serious gastric side effects such as nausea and diarrhea.
“With all of the complications they develop, the typical patient takes 40 to 60 pills a day around the clock,” Cherqui says. “They literally have a suitcase of medications they have to carry everywhere, and all of those medications don’t stop the progression of the disease, and they still die from it.”
Cherqui has been a proponent of gene therapy to treat children’s disorders since studying cystinosis while earning her doctorate in 2002. Today, her lab focuses on developing stem cell and gene therapy strategies for degenerative, hereditary disorders such as cystinosis that affect multiple systems of the body. “Because cystinosis expresses in every tissue in the body, I decided to use the blood-forming stem cells that we have in our bone marrow,” she explains. “These cells can migrate to anywhere in the body where the person has an injury from the disease.”
AVROBIO’s hematopoietic stem cell gene therapy approach collects stem cells from the patient’s bone marrow. They then genetically modify the stem cells to give the patient a copy of the healthy CTNS gene, which the person either doesn’t have or it’s defective.
The patient first undergoes apheresis, a medical procedure in which their blood is passed through an apparatus that separates out the diseased stem cells, and a process called conditioning is used to help eliminate the damaged cells so they can be replaced by the infusion of the patient’s genetically modified stem cells. Once they become engrafted into the patient’s bone marrow, they reproduce into a lot of daughter cells, and all of those daughter cells contain the CTNS gene. Those cells are able to express the healthy, functional, active protein throughout the body to correct the metabolic problem caused by cystinosis.
“What we’re seeing in the adult patients who have been dosed to date is the consistent and sustained engraftment of our genetically modified cells, 17 to 27 months post-gene therapy, so that’s very encouraging and positive,” says Rihda, the chief medical officer at AVROBIO.
When Janz was 11-years-old, his mother got him enrolled in the trial of a new form of cysteamine that would only need to be taken every 12 hours instead of every six. Two years later, she made sure he was the first person on the list for Cherqui’s current stem cell gene therapy trial.
AVROBIO researchers have also confirmed stabilization or improvement in motor coordination and visual perception in the trial participants, suggesting a potential impact on the neuropathology of the disease. Data from five dosed patients show strong safety and tolerability as well as reduced accumulation of cystine crystals in cells across multiple tissues in the first three patients. None of the five patients need to take oral cysteamine.
Janz’s mother, Barb Kulyk, whom he credits with always making him take his medications and keeping him hydrated, had been following Cherqui’s research since his early childhood. When Janz was 11-years-old, she got him enrolled in the trial of a new form of cysteamine that would only need to be taken every 12 hours instead of every six. When he was 17, the FDA approved that drug. Two years later, his mother made sure he was the first person on the list for Cherqui’s current stem cell gene therapy trial. He received his new stem cells on October 7th, 2019, went home in January 2020, and returned to working full time in February.

Jordan Janz, pictured here with his girlfriend, has a new lease on life, plus a new hair color.
Jordan Janz
He notes that his energy level is significantly better, and his mother has noticed much improvement in him and his daily functioning: He rarely vomits or gets nauseous in the morning, and he has more color in his face as well as his hair. Although he could finish his participation at any time, he recently decided to continue in the clinical trial.
Before the trial, Janz was taking 56 pills daily. He is completely off all of those medications and only takes pills to keep his kidneys working. Because of the damage caused by cystinosis over the course of his life, he’s down to about 20 percent kidney function and will eventually need a transplant.
“Some day, though, thanks to Dr. Cherqui’s team and AVROBIO’s work, when I get a new kidney, cystinosis won’t destroy it,” he concludes.