If New Metal Legs Let You Run 20 Miles/Hour, Would You Amputate Your Own?
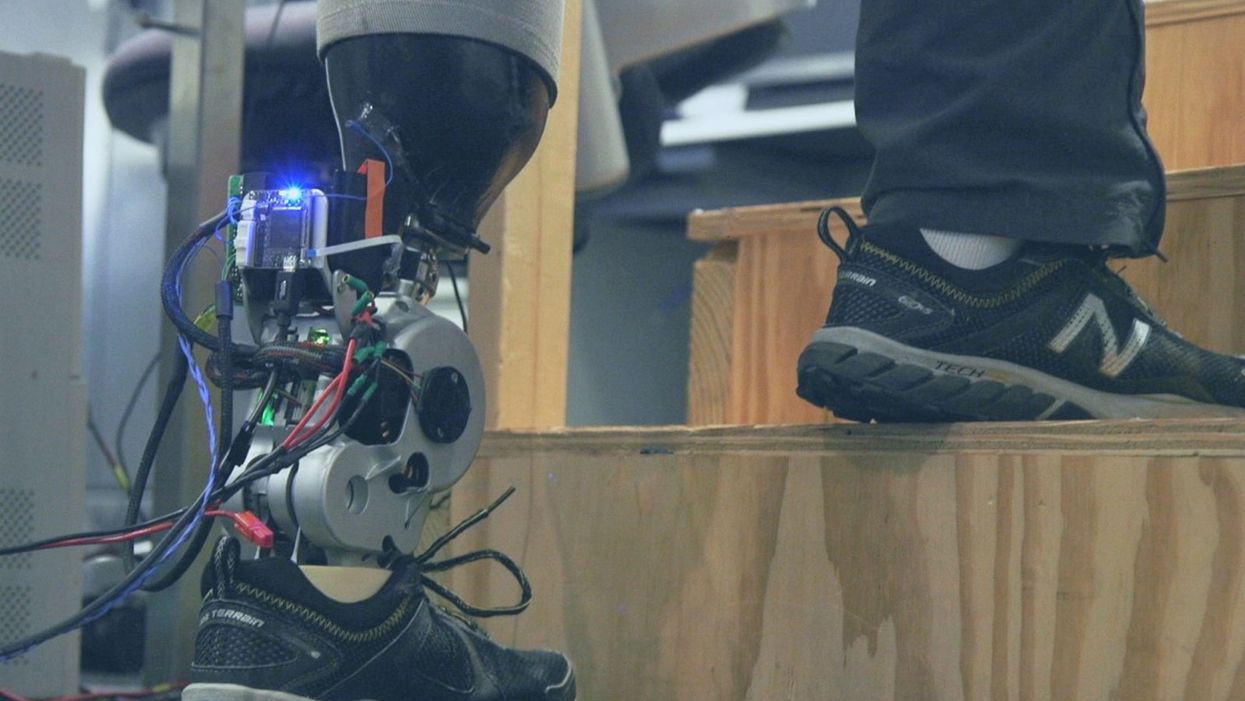
A patient with below-knee AMI amputation walks up the stairs.
"Here's a question for you," I say to our dinner guests, dodging a knowing glance from my wife. "Imagine a future in which you could surgically replace your legs with robotic substitutes that had all the functionality and sensation of their biological counterparts. Let's say these new legs would allow you to run all day at 20 miles per hour without getting tired. Would you have the surgery?"
Why are we so married to the arbitrary distinction between rehabilitating and augmenting?
Like most people I pose this question to, our guests respond with some variation on the theme of "no way"; the idea of undergoing a surgical procedure with the sole purpose of augmenting performance beyond traditional human limits borders on the unthinkable.
"Would your answer change if you had arthritis in your knees?" This is where things get interesting. People think differently about intervention when injury or illness is involved. The idea of a major surgery becomes more tractable to us in the setting of rehabilitation.
Consider the simplistic example of human walking speed. The average human walks at a baseline three miles per hour. If someone is only able to walk at one mile per hour, we do everything we can to increase their walking ability. However, to take a person who is already able to walk at three miles per hour and surgically alter their body so that they can walk twice as fast seems, to us, unreasonable.
What fascinates me about this is that the three-mile-per-hour baseline is set by arbitrary limitations of the healthy human body. If we ignore this reference point altogether, and consider that each case simply offers an improvement in walking ability, the line between augmentation and rehabilitation all but disappears. Why, then, are we so married to this arbitrary distinction between rehabilitating and augmenting? What makes us hold so tightly to baseline human function?
Where We Stand Now
As the functionality of advanced prosthetic devices continues to increase at an astounding rate, questions like these are becoming more relevant. Experimental prostheses, intended for the rehabilitation of people with amputation, are now able to replicate the motions of biological limbs with high fidelity. Neural interfacing technologies enable a person with amputation to control these devices with their brain and nervous system. Before long, synthetic body parts will outperform biological ones.
Our approach allows people to not only control a prosthesis with their brain, but also to feel its movements as if it were their own limb.
Against this backdrop, my colleagues and I developed a methodology to improve the connection between the biological body and a synthetic limb. Our approach, known as the agonist-antagonist myoneural interface ("AMI" for short), enables us to reflect joint movement sensations from a prosthetic limb onto the human nervous system. In other words, the AMI allows people to not only control a prosthesis with their brain, but also to feel its movements as if it were their own limb. The AMI involves a reimagining of the amputation surgery, so that the resultant residual limb is better suited to interact with a neurally-controlled prosthesis. In addition to increasing functionality, the AMI was designed with the primary goal of enabling adoption of a prosthetic limb as part of a patient's physical identity (known as "embodiment").
Early results have been remarkable. Patients with below-knee AMI amputation are better able to control an experimental prosthetic leg, compared to people who had their legs amputated in the traditional way. In addition, the AMI patients show increased evidence of embodiment. They identify with the device, and describe feeling as though it is part of them, part of self.
Where We're Going
True embodiment of robotic devices has the potential to fundamentally alter humankind's relationship with the built world. Throughout history, humans have excelled as tool builders. We innovate in ways that allow us to design and augment the world around us. However, tools for augmentation are typically external to our body identity; there is a clean line drawn between smart phone and self. As we advance our ability to integrate synthetic systems with physical identity, humanity will have the capacity to sculpt that very identity, rather than just the world in which it exists.
For this potential to be realized, we will need to let go of our reservations about surgery for augmentation. In reality, this shift has already begun. Consider the approximately 17.5 million surgical and minimally invasive cosmetic procedures performed in the United States in 2017 alone. Many of these represent patients with no demonstrated medical need, who have opted to undergo a surgical procedure for the sole purpose of synthetically enhancing their body. The ethical basis for such a procedure is built on the individual perception that the benefits of that procedure outweigh its costs.
At present, it seems absurd that amputation would ever reach this point. However, as robotic technology improves and becomes more integrated with self, the balance of cost and benefit will shift, lending a new perspective on what now seems like an unfathomable decision to electively amputate a healthy limb. When this barrier is crossed, we will collide head-on with the question of whether it is acceptable for a person to "upgrade" such an essential part of their body.
At a societal level, the potential benefits of physical augmentation are far-reaching. The world of robotic limb augmentation will be a world of experienced surgeons whose hands are perfectly steady, firefighters whose legs allow them to kick through walls, and athletes who never again have to worry about injury. It will be a world in which a teenage boy and his grandmother embark together on a four-hour sprint through the woods, for the sheer joy of it. It will be a world in which the human experience is fundamentally enriched, because our bodies, which play such a defining role in that experience, are truly malleable.
This is not to say that such societal benefits stand without potential costs. One justifiable concern is the misuse of augmentative technologies. We are all quite familiar with the proverbial supervillain whose nervous system has been fused to that of an all-powerful robot.
The world of robotic limb augmentation will be a world of experienced surgeons whose hands are perfectly steady.
In reality, misuse is likely to be both subtler and more insidious than this. As with all new technology, careful legislation will be necessary to work against those who would hijack physical augmentations for violent or oppressive purposes. It will also be important to ensure broad access to these technologies, to protect against further socioeconomic stratification. This particular issue is helped by the tendency of the cost of a technology to scale inversely with market size. It is my hope that when robotic augmentations are as ubiquitous as cell phones, the technology will serve to equalize, rather than to stratify.
In our future bodies, when we as a society decide that the benefits of augmentation outweigh the costs, it will no longer matter whether the base materials that make us up are biological or synthetic. When our AMI patients are connected to their experimental prosthesis, it is irrelevant to them that the leg is made of metal and carbon fiber; to them, it is simply their leg. After our first patient wore the experimental prosthesis for the first time, he sent me an email that provides a look at the immense possibility the future holds:
What transpired is still slowly sinking in. I keep trying to describe the sensation to people. Then this morning my daughter asked me if I felt like a cyborg. The answer was, "No, I felt like I had a foot."
Stronger psychedelics that rewire the brain, with Doug Drysdale
Today's podcast episode features Doug Drysdale, CEO of Cybin, a company that is leading innovations in psilocybin, mushrooms that may help people with anxiety and depression.
A promising development in science in recent years has been the use technology to optimize something natural. One-upping nature's wisdom isn't easy. In many cases, we haven't - and maybe we can't - figure it out. But today's episode features a fascinating example: using tech to optimize psychedelic mushrooms.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
These mushrooms have been used for religious, spiritual and medicinal purposes for thousands of years, but only in the past several decades have scientists brought psychedelics into the lab to enhance them and maximize their therapeutic value.
Today’s podcast guest, Doug Drysdale, is doing important work to lead this effort. Drysdale is the CEO of a company called Cybin that has figured out how to make psilocybin more potent, so it can be administered in smaller doses without side effects.
The natural form of psilocybin has been studied increasingly in the realm of mental health. Taking doses of these mushrooms appears to help people with anxiety and depression by spurring the development of connections in the brain, an example of neuroplasticity. The process basically shifts the adult brain from being fairly rigid like dried clay into a malleable substance like warm wax - the state of change that's constantly underway in the developing brains of children.
Neuroplasticity in adults seems to unlock some of our default ways of of thinking, the habitual thought patterns that’ve been associated with various mental health problems. Some promising research suggests that psilocybin causes a reset of sorts. It makes way for new, healthier thought patterns.
So what is Drysdale’s secret weapon to bring even more therapeutic value to psilocybin? It’s a process called deuteration. It focuses on the hydrogen atoms in psilocybin. These atoms are very light and don’t stick very well to carbon, which is another atom in psilocybin. As a result, our bodies can easily breaks down the bonds between the hydrogen and carbon atoms. For many people, that means psilocybin gets cleared from the body too quickly, before it can have a therapeutic benefit.
In deuteration, scientists do something simple but ingenious: they replace the hydrogen atoms with a molecule called deuterium. It’s twice as heavy as hydrogen and forms tighter bonds with the carbon. Because these pairs are so rock-steady, they slow down the rate at which psilocybin is metabolized, so it has more sustained effects on our brains.
Cybin isn’t Drysdale’s first go around at this - far from it. He has over 30 years of experience in the healthcare sector. During this time he’s raised around $4 billion of both public and private capital, and has been named Ernst and Young Entrepreneur of the Year. Before Cybin, he was the founding CEO of a pharmaceutical company called Alvogen, leading it from inception to around $500 million in revenues, across 35 countries. Drysdale has also been the head of mergers and acquisitions at Actavis Group, leading 15 corporate acquisitions across three continents.
In this episode, Drysdale walks us through the promising research of his current company, Cybin, and the different therapies he’s developing for anxiety and depression based not just on psilocybin but another psychedelic compound found in plants called DMT. He explains how they seem to have such powerful effects on the brain, as well as the potential for psychedelics to eventually support other use cases, including helping us strive toward higher levels of well-being. He goes on to discuss his views on mindfulness and lifestyle factors - such as optimal nutrition - that could help bring out hte best in psychedelics.
Show links:
Doug Drysdale full bio
Doug Drysdale twitter
Cybin website
Cybin development pipeline
Cybin's promising phase 2 research on depression
Johns Hopkins psychedelics research and psilocybin research
Mets owner Steve Cohen invests in psychedelic therapies

Doug Drysdale, CEO of Cybin
How the body's immune resilience affects our health and lifespan
Immune cells battle an infection.
Story by Big Think
It is a mystery why humans manifest vast differences in lifespan, health, and susceptibility to infectious diseases. However, a team of international scientists has revealed that the capacity to resist or recover from infections and inflammation (a trait they call “immune resilience”) is one of the major contributors to these differences.
Immune resilience involves controlling inflammation and preserving or rapidly restoring immune activity at any age, explained Weijing He, a study co-author. He and his colleagues discovered that people with the highest level of immune resilience were more likely to live longer, resist infection and recurrence of skin cancer, and survive COVID and sepsis.
Measuring immune resilience
The researchers measured immune resilience in two ways. The first is based on the relative quantities of two types of immune cells, CD4+ T cells and CD8+ T cells. CD4+ T cells coordinate the immune system’s response to pathogens and are often used to measure immune health (with higher levels typically suggesting a stronger immune system). However, in 2021, the researchers found that a low level of CD8+ T cells (which are responsible for killing damaged or infected cells) is also an important indicator of immune health. In fact, patients with high levels of CD4+ T cells and low levels of CD8+ T cells during SARS-CoV-2 and HIV infection were the least likely to develop severe COVID and AIDS.
Individuals with optimal levels of immune resilience were more likely to live longer.
In the same 2021 study, the researchers identified a second measure of immune resilience that involves two gene expression signatures correlated with an infected person’s risk of death. One of the signatures was linked to a higher risk of death; it includes genes related to inflammation — an essential process for jumpstarting the immune system but one that can cause considerable damage if left unbridled. The other signature was linked to a greater chance of survival; it includes genes related to keeping inflammation in check. These genes help the immune system mount a balanced immune response during infection and taper down the response after the threat is gone. The researchers found that participants who expressed the optimal combination of genes lived longer.
Immune resilience and longevity
The researchers assessed levels of immune resilience in nearly 50,000 participants of different ages and with various types of challenges to their immune systems, including acute infections, chronic diseases, and cancers. Their evaluation demonstrated that individuals with optimal levels of immune resilience were more likely to live longer, resist HIV and influenza infections, resist recurrence of skin cancer after kidney transplant, survive COVID infection, and survive sepsis.
However, a person’s immune resilience fluctuates all the time. Study participants who had optimal immune resilience before common symptomatic viral infections like a cold or the flu experienced a shift in their gene expression to poor immune resilience within 48 hours of symptom onset. As these people recovered from their infection, many gradually returned to the more favorable gene expression levels they had before. However, nearly 30% who once had optimal immune resilience did not fully regain that survival-associated profile by the end of the cold and flu season, even though they had recovered from their illness.
Intriguingly, some people who are 90+ years old still have optimal immune resilience, suggesting that these individuals’ immune systems have an exceptional capacity to control inflammation and rapidly restore proper immune balance.
This could suggest that the recovery phase varies among people and diseases. For example, young female sex workers who had many clients and did not use condoms — and thus were repeatedly exposed to sexually transmitted pathogens — had very low immune resilience. However, most of the sex workers who began reducing their exposure to sexually transmitted pathogens by using condoms and decreasing their number of sex partners experienced an improvement in immune resilience over the next 10 years.
Immune resilience and aging
The researchers found that the proportion of people with optimal immune resilience tended to be highest among the young and lowest among the elderly. The researchers suggest that, as people age, they are exposed to increasingly more health conditions (acute infections, chronic diseases, cancers, etc.) which challenge their immune systems to undergo a “respond-and-recover” cycle. During the response phase, CD8+ T cells and inflammatory gene expression increase, and during the recovery phase, they go back down.
However, over a lifetime of repeated challenges, the immune system is slower to recover, altering a person’s immune resilience. Intriguingly, some people who are 90+ years old still have optimal immune resilience, suggesting that these individuals’ immune systems have an exceptional capacity to control inflammation and rapidly restore proper immune balance despite the many respond-and-recover cycles that their immune systems have faced.
Public health ramifications could be significant. Immune cell and gene expression profile assessments are relatively simple to conduct, and being able to determine a person’s immune resilience can help identify whether someone is at greater risk for developing diseases, how they will respond to treatment, and whether, as well as to what extent, they will recover.