If New Metal Legs Let You Run 20 Miles/Hour, Would You Amputate Your Own?
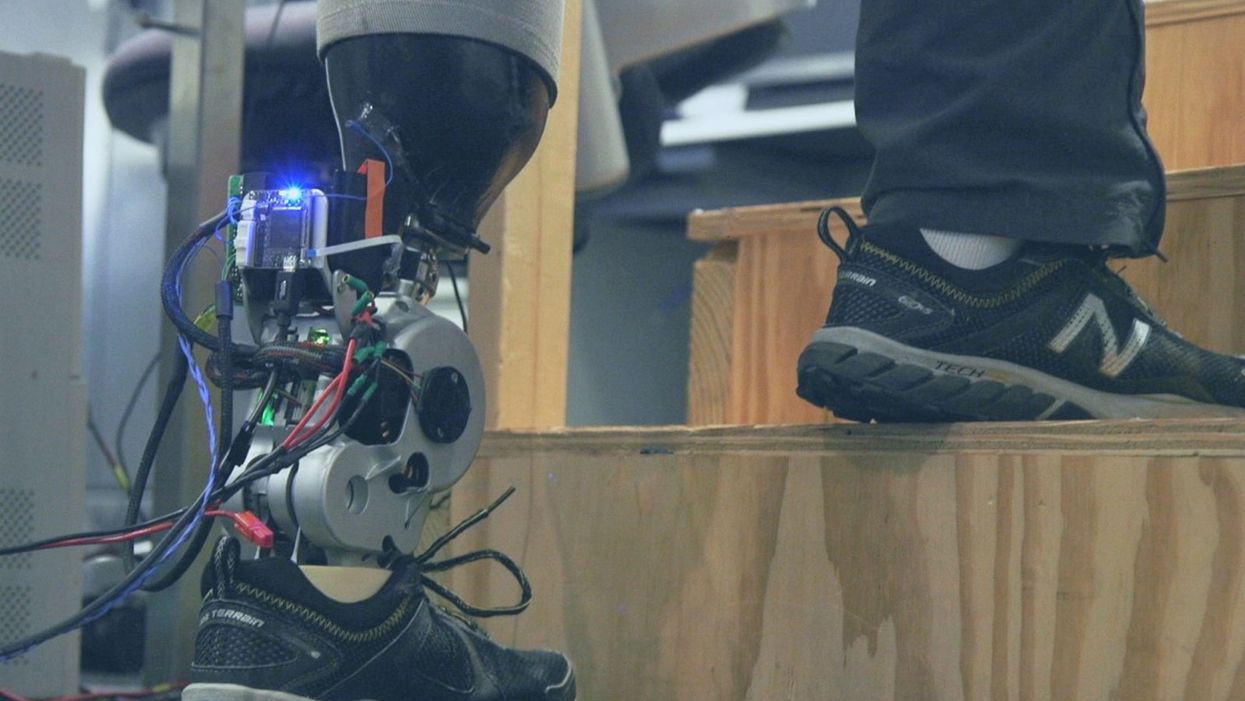
A patient with below-knee AMI amputation walks up the stairs.
"Here's a question for you," I say to our dinner guests, dodging a knowing glance from my wife. "Imagine a future in which you could surgically replace your legs with robotic substitutes that had all the functionality and sensation of their biological counterparts. Let's say these new legs would allow you to run all day at 20 miles per hour without getting tired. Would you have the surgery?"
Why are we so married to the arbitrary distinction between rehabilitating and augmenting?
Like most people I pose this question to, our guests respond with some variation on the theme of "no way"; the idea of undergoing a surgical procedure with the sole purpose of augmenting performance beyond traditional human limits borders on the unthinkable.
"Would your answer change if you had arthritis in your knees?" This is where things get interesting. People think differently about intervention when injury or illness is involved. The idea of a major surgery becomes more tractable to us in the setting of rehabilitation.
Consider the simplistic example of human walking speed. The average human walks at a baseline three miles per hour. If someone is only able to walk at one mile per hour, we do everything we can to increase their walking ability. However, to take a person who is already able to walk at three miles per hour and surgically alter their body so that they can walk twice as fast seems, to us, unreasonable.
What fascinates me about this is that the three-mile-per-hour baseline is set by arbitrary limitations of the healthy human body. If we ignore this reference point altogether, and consider that each case simply offers an improvement in walking ability, the line between augmentation and rehabilitation all but disappears. Why, then, are we so married to this arbitrary distinction between rehabilitating and augmenting? What makes us hold so tightly to baseline human function?
Where We Stand Now
As the functionality of advanced prosthetic devices continues to increase at an astounding rate, questions like these are becoming more relevant. Experimental prostheses, intended for the rehabilitation of people with amputation, are now able to replicate the motions of biological limbs with high fidelity. Neural interfacing technologies enable a person with amputation to control these devices with their brain and nervous system. Before long, synthetic body parts will outperform biological ones.
Our approach allows people to not only control a prosthesis with their brain, but also to feel its movements as if it were their own limb.
Against this backdrop, my colleagues and I developed a methodology to improve the connection between the biological body and a synthetic limb. Our approach, known as the agonist-antagonist myoneural interface ("AMI" for short), enables us to reflect joint movement sensations from a prosthetic limb onto the human nervous system. In other words, the AMI allows people to not only control a prosthesis with their brain, but also to feel its movements as if it were their own limb. The AMI involves a reimagining of the amputation surgery, so that the resultant residual limb is better suited to interact with a neurally-controlled prosthesis. In addition to increasing functionality, the AMI was designed with the primary goal of enabling adoption of a prosthetic limb as part of a patient's physical identity (known as "embodiment").
Early results have been remarkable. Patients with below-knee AMI amputation are better able to control an experimental prosthetic leg, compared to people who had their legs amputated in the traditional way. In addition, the AMI patients show increased evidence of embodiment. They identify with the device, and describe feeling as though it is part of them, part of self.
Where We're Going
True embodiment of robotic devices has the potential to fundamentally alter humankind's relationship with the built world. Throughout history, humans have excelled as tool builders. We innovate in ways that allow us to design and augment the world around us. However, tools for augmentation are typically external to our body identity; there is a clean line drawn between smart phone and self. As we advance our ability to integrate synthetic systems with physical identity, humanity will have the capacity to sculpt that very identity, rather than just the world in which it exists.
For this potential to be realized, we will need to let go of our reservations about surgery for augmentation. In reality, this shift has already begun. Consider the approximately 17.5 million surgical and minimally invasive cosmetic procedures performed in the United States in 2017 alone. Many of these represent patients with no demonstrated medical need, who have opted to undergo a surgical procedure for the sole purpose of synthetically enhancing their body. The ethical basis for such a procedure is built on the individual perception that the benefits of that procedure outweigh its costs.
At present, it seems absurd that amputation would ever reach this point. However, as robotic technology improves and becomes more integrated with self, the balance of cost and benefit will shift, lending a new perspective on what now seems like an unfathomable decision to electively amputate a healthy limb. When this barrier is crossed, we will collide head-on with the question of whether it is acceptable for a person to "upgrade" such an essential part of their body.
At a societal level, the potential benefits of physical augmentation are far-reaching. The world of robotic limb augmentation will be a world of experienced surgeons whose hands are perfectly steady, firefighters whose legs allow them to kick through walls, and athletes who never again have to worry about injury. It will be a world in which a teenage boy and his grandmother embark together on a four-hour sprint through the woods, for the sheer joy of it. It will be a world in which the human experience is fundamentally enriched, because our bodies, which play such a defining role in that experience, are truly malleable.
This is not to say that such societal benefits stand without potential costs. One justifiable concern is the misuse of augmentative technologies. We are all quite familiar with the proverbial supervillain whose nervous system has been fused to that of an all-powerful robot.
The world of robotic limb augmentation will be a world of experienced surgeons whose hands are perfectly steady.
In reality, misuse is likely to be both subtler and more insidious than this. As with all new technology, careful legislation will be necessary to work against those who would hijack physical augmentations for violent or oppressive purposes. It will also be important to ensure broad access to these technologies, to protect against further socioeconomic stratification. This particular issue is helped by the tendency of the cost of a technology to scale inversely with market size. It is my hope that when robotic augmentations are as ubiquitous as cell phones, the technology will serve to equalize, rather than to stratify.
In our future bodies, when we as a society decide that the benefits of augmentation outweigh the costs, it will no longer matter whether the base materials that make us up are biological or synthetic. When our AMI patients are connected to their experimental prosthesis, it is irrelevant to them that the leg is made of metal and carbon fiber; to them, it is simply their leg. After our first patient wore the experimental prosthesis for the first time, he sent me an email that provides a look at the immense possibility the future holds:
What transpired is still slowly sinking in. I keep trying to describe the sensation to people. Then this morning my daughter asked me if I felt like a cyborg. The answer was, "No, I felt like I had a foot."
A startup aims to make medicines in space
A company is looking to improve medicines by making them in the nearly weightless environment of space.
Story by Big Think
On June 12, a SpaceX Falcon 9 rocket deployed 72 small satellites for customers — including the world’s first space factory.
The challenge: In 2019, pharma giant Merck revealed that an experiment on the International Space Station had shown how to make its blockbuster cancer drug Keytruda more stable. That meant it could now be administered via a shot rather than through an IV infusion.
The key to the discovery was the fact that particles behave differently when freed from the force of gravity — seeing how its drug crystalized in microgravity helped Merck figure out how to tweak its manufacturing process on Earth to produce the more stable version.
Microgravity research could potentially lead to many more discoveries like this one, or even the development of brand-new drugs, but ISS astronauts only have so much time for commercial experiments.
“There are many high-performance products that are only possible to make in zero-gravity, which is a manufacturing capability that cannot be replicated in any factory on Earth.”-- Will Bruey.
The only options for accessing microgravity (or free fall) outside of orbit, meanwhile, are parabolic airplane flights and drop towers, and those are only useful for experiments that require less than a minute in microgravity — Merck’s ISS experiment took 18 days.
The idea: In 2021, California startup Varda Space Industries announced its intention to build the world’s first space factory, to manufacture not only pharmaceuticals but other products that could benefit from being made in microgravity, such as semiconductors and fiber optic cables.
This factory would consist of a commercial satellite platform attached to two Varda-made modules. One module would contain equipment capable of autonomously manufacturing a product. The other would be a reentry capsule to bring the finished goods back to Earth.
“There are many high-performance products that are only possible to make in zero-gravity, which is a manufacturing capability that cannot be replicated in any factory on Earth,” said CEO Will Bruey, who’d previously developed and flown spacecraft for SpaceX.
“We have a team stacked with aerospace talent in the prime of their careers, focused on getting working hardware to orbit as quickly as possible,” he continued.
“[Pharmaceuticals] are the most valuable chemicals per unit mass. And they also have a large market on Earth.” -- Will Bruey, CEO of Varda Space.
What’s new? At the time, Varda said it planned to launch its first space factory in 2023, and, in what feels like a first for a space startup, it has actually hit that ambitious launch schedule.
“We have ACQUISITION OF SIGNAL,” the startup tweeted soon after the Falcon 9 launch on June 12. “The world’s first space factory’s solar panels have found the sun and it’s beginning to de-tumble.”
During the satellite’s first week in space, Varda will focus on testing its systems to make sure everything works as hoped. The second week will be dedicated to heating and cooling the old HIV-AIDS drug ritonavir repeatedly to study how its particles crystalize in microgravity.
After about a month in space, Varda will attempt to bring its first space factory back to Earth, sending it through the atmosphere at hypersonic speeds and then using a parachute system to safely land at the Department of Defense’s Utah Test and Training Range.
Looking ahead: Ultimately, Varda’s space factories could end up serving dual purposes as manufacturing facilities and hypersonic testbeds — the Air Force has already awarded the startup a contract to use its next reentry capsule to test hardware for hypersonic missiles.
But as for manufacturing other types of goods, Varda plans to stick with drugs for now.
“[Pharmaceuticals] are the most valuable chemicals per unit mass,” Bruey told CNN. “And they also have a large market on Earth.”
“You’re not going to see Varda do anything other than pharmaceuticals for the next minimum of six, seven years,” added Delian Asparouhov, Varda’s co-founder and president.
This article originally appeared on Big Think, home of the brightest minds and biggest ideas of all time.
Genes that protect health with Dr. Nir Barzilai
Centenarians essentially won the genetic lottery, says Nir Barzilai of Albert Einstein College of Medicine. He is studying their genes to see how the rest of us can benefit from understanding how they work.
In today’s podcast episode, I talk with Nir Barzilai, a geroscientist, which means he studies the biology of aging. Barzilai directs the Institute for Aging Research at the Albert Einstein College of Medicine.
My first question for Dr. Barzilai was: why do we age? And is there anything to be done about it? His answers were encouraging. We can’t live forever, but we have some control over the process, as he argues in his book, Age Later.
Dr. Barzilai told me that centenarians differ from the rest of us because they have unique gene mutations that help them stay healthy longer. For most of us, the words “gene mutations” spell trouble - we associate these words with cancer or neurodegenerative diseases, but apparently not all mutations are bad.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Centenarians may have essentially won the genetic lottery, but that doesn’t mean the rest of us are predestined to have a specific lifespan and health span, or the amount of time spent living productively and enjoyably. “Aging is a mother of all diseases,” Dr. Barzilai told me. And as a disease, it can be targeted by therapeutics. Dr. Barzilai’s team is already running clinical trials on such therapeutics — and the results are promising.
More about Dr. Barzilai: He is scientific director of AFAR, American Federation for Aging Research. As part of his work, Dr. Barzilai studies families of centenarians and their genetics to learn how the rest of us can learn and benefit from their super-aging. He also organizing a clinical trial to test a specific drug that may slow aging.
Show Links
Age Later: Health Span, Life Span, and the New Science of Longevity https://www.amazon.com/Age-Later-Healthiest-Sharpest-Centenarians/dp/1250230853
American Federation for Aging Research https://www.afar.org
https://www.afar.org/nir-barzilai
https://www.einsteinmed.edu/faculty/484/nir-barzilai/
Metformin as a Tool to Target Aging
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5943638/
Benefits of Metformin in Attenuating the Hallmarks of Aging https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7347426/
The Longevity Genes Project https://www.einsteinmed.edu/centers/aging/longevity-genes-project/
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.