How 30 Years of Heart Surgeries Taught My Dad How to Live
A mid-1970s photo of the author's father, and him holding a grandchild in 2012.
[Editor's Note: This piece is the winner of our 2019 essay contest, which prompted readers to reflect on the question: "How has an advance in science or medicine changed your life?"]
My father did not expect to live past the age of 50. Neither of his parents had done so. And he also knew how he would die: by heart attack, just as his father did.
In July of 1976, he had his first heart attack, days before his 40th birthday.
My dad lived the first 40 years of his life with this knowledge buried in his bones. He started smoking at the age of 12, and was drinking before he was old enough to enlist in the Navy. He had a sarcastic, often cruel, sense of humor that could drive my mother, my sister and me into tears. He was not an easy man to live with, but that was okay by him - he didn't expect to live long.
In July of 1976, he had his first heart attack, days before his 40th birthday. I was 13, and my sister was 11. He needed quadruple bypass surgery. Our small town hospital was not equipped to do this type of surgery; he would have to be transported 40 miles away to a heart center. I understood this journey to mean that my father was seriously ill, and might die in the hospital, away from anyone he knew. And my father knew a lot of people - he was a popular high school English teacher, in a town with only three high schools. He knew generations of students and their parents. Our high school football team did a blood drive in his honor.

During a trip to Disney World in 1974, Dad was suffering from angina the entire time but refused to tell me (left) and my sister, Kris.
Quadruple bypass surgery in 1976 meant that my father's breastbone was cut open by a sternal saw. His ribcage was spread wide. After the bypass surgery, his bones would be pulled back together, and tied in place with wire. The wire would later be pulled out of his body when the bones knitted back together. It would take months before he was fully healed.
Dad was in the hospital for the rest of the summer and into the start of the new school year. Going to visit him was farther than I could ride my bicycle; it meant planning a trip in the car and going onto the interstate. The first time I was allowed to visit him in the ICU, he was lying in bed, and then pushed himself to sit up. The heart monitor he was attached to spiked up and down, and I fainted. I didn't know that heartbeats change when you move; television medical dramas never showed that - I honestly thought that I had driven my father into another heart attack.
Only a few short years after that, my father returned to the big hospital to have his heart checked with a new advance in heart treatment: a CT scan. This would allow doctors to check for clogged arteries and treat them before a fatal heart attack. The procedure identified a dangerous blockage, and my father was admitted immediately. This time, however, there was no need to break bones to get to the problem; my father was home within a month.
During the late 1970's, my father changed none of his habits. He was still smoking, and he continued to drink. But now, he was also taking pills - pills to manage the pain. He would pop a nitroglycerin tablet under his tongue whenever he was experiencing angina (I have a vivid memory of him doing this during my driving lessons), but he never mentioned that he was in pain. Instead, he would snap at one of us, or joke that we were killing him.
I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count.
Being the kind of guy he was, my father never wanted to talk about his health. Any admission of pain implied that he couldn't handle pain. He would try to "muscle through" his angina, as if his willpower would be stronger than his heart muscle. His efforts would inevitably fail, leaving him angry and ready to lash out at anyone or anything. He would blame one of us as a reason he "had" to take valium or pop a nitro tablet. Dinners often ended in shouts and tears, and my father stalking to the television room with a bottle of red wine.
In the 1980's while I was in college, my father had another heart attack. But now, less than 10 years after his first, medicine had changed: our hometown hospital had the technology to run dye through my father's blood stream, identify the blockages, and do preventative care that involved statins and blood thinners. In one case, the doctors would take blood vessels from my father's legs, and suture them to replace damaged arteries around his heart. New advances in cholesterol medication and treatments for angina could extend my father's life by many years.
My father decided it was time to quit smoking. It was the first significant health step I had ever seen him take. Until then, he treated his heart issues as if they were inevitable, and there was nothing that he could do to change what was happening to him. Quitting smoking was the first sign that my father was beginning to move out of his fatalistic mindset - and the accompanying fatal behaviors that all pointed to an early death.
In 1986, my father turned 50. He had now lived longer than either of his parents. The habits he had learned from them could be changed. He had stopped smoking - what else could he do?
It was a painful decade for all of us. My parents divorced. My sister quit college. I moved to the other side of the country and stopped speaking to my father for almost 10 years. My father remarried, and divorced a second time. I stopped counting the number of times he was in and out of the hospital with heart-related issues.
In the early 1990's, my father reached out to me. I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count. He traveled across the country to spend a week with me, to meet my friends, and to rebuild his relationship with me. He did the same with my sister. He stopped drinking. He was more forthcoming about his health, and admitted that he was taking an antidepressant. His humor became less cruel and sadistic. He took an active interest in the world. He became part of my life again.
The 1990's was also the decade of angioplasty. My father explained it to me like this: during his next surgery, the doctors would place balloons in his arteries, and inflate them. The balloons would then be removed (or dissolve), leaving the artery open again for blood. He had several of these surgeries over the next decade.
When my father was in his 60's, he danced at with me at my wedding. It was now 10 years past the time he had expected to live, and his life was transformed. He was living with a woman I had known since I was a child, and my wife and I would make regular visits to their home. My father retired from teaching, became an avid gardener, and always had a home project underway. He was a happy man.

Dancing with my father at my wedding in 1998.
Then, in the mid 2000's, my father faced another serious surgery. Years of arterial surgery, angioplasty, and damaged heart muscle were taking their toll. He opted to undergo a life-saving surgery at Cleveland Clinic. By this time, I was living in New York and my sister was living in Arizona. We both traveled to the Midwest to be with him. Dad was unconscious most of the time. We took turns holding his hand in the ICU, encouraging him to regain his will to live, and making outrageous threats if he didn't listen to us.
The nursing staff were wonderful. I remember telling them that my father had never expected to live this long. One of the nurses pointed out that most of the patients in their ward were in their 70's and 80's, and a few were in their 90's. She reminded me that just a decade earlier, most hospitals were unwilling to do the kind of surgery my father had received on patients his age. In the first decade of the 21st century, however, things were different: 90-year-olds could now undergo heart surgery and live another decade. My father was on the "young" side of their patients.
The Cleveland Clinic visit would be the last major heart surgery my father would have. Not that he didn't return to his local hospital a few times after that: he broke his neck -- not once, but twice! -- slipping on ice. And in the 2010's, he began to show signs of dementia, and needed more home care. His partner, who had her own health issues, was not able to provide the level of care my father needed. My sister invited him to move in with her, and in 2015, I traveled with him to Arizona to get him settled in.
After a few months, he accepted home hospice. We turned off his pacemaker when the hospice nurse explained to us that the job of a pacemaker is to literally jolt a patient's heart back into beating. The jolts were happening more and more frequently, causing my Dad additional, unwanted pain.

My father in 2015, a few months before his death.
My father died in February 2016. His body carried the scars and implants of 30 years of cardiac surgeries, from the ugly breastbone scar from the 1970's to scars on his arms and legs from borrowed blood vessels, to the tiny red circles of robotic incisions from the 21st century. The arteries and veins feeding his heart were a patchwork of transplanted leg veins and fragile arterial walls pressed thinner by balloons.
And my father died with no regrets or unfinished business. He died in my sister's home, with his long-time partner by his side. Medical advancements had given him the opportunity to live 30 years longer than he expected. But he was the one who decided how to live those extra years. He was the one who made the years matter.
Employers can create a culture of “Excellence From Anywhere” to reduce the risk of inequality among office-centric, hybrid, and fully remote employees.
COVID-19 prompted numerous companies to reconsider their approach to the future of work. Many leaders felt reluctant about maintaining hybrid and remote work options after vaccines became widely available. Yet the emergence of dangerous COVID variants such as Omicron has shown the folly of this mindset.
To mitigate the risks of new variants and other public health threats, as well as to satisfy the desires of a large majority of employees who express a strong desire in multiple surveys for a flexible hybrid or fully remote schedule, leaders are increasingly accepting that hybrid and remote options represent the future of work. No wonder that a February 2022 survey by the Federal Reserve Bank of Richmond showed that more and more firms are offering hybrid and fully-remote work options. The firms expect to have more remote workers next year and more geographically-distributed workers.
Although hybrid and remote work mitigates public health risks, it poses another set of health concerns relevant to employee wellbeing, due to the threat of proximity bias. This term refers to the negative impact on work culture from the prospect of inequality among office-centric, hybrid, and fully remote employees.
The difference in time spent in the office leads to concerns ranging from decreased career mobility for those who spend less facetime with their supervisor to resentment building up against the staff who have the most flexibility in where to work. In fact, a January 2022 survey by the company Slack of over 10,000 knowledge workers and their leaders shows that proximity bias is the top concern – expressed by 41% of executives - about hybrid and remote work.
To address this problem requires using best practices based on cognitive science for creating a culture of “Excellence From Anywhere.” This solution is based on guidance that I developed for leaders at 17 pioneering organizations for a company culture fit for the future of work.
Protect from proximity bias via the "Excellence From Anywhere" strategy
So why haven’t firms addressed the obvious problem of proximity bias? Any reasonable external observer could predict the issues arising from differences of time spent in the office.
Unfortunately, leaders often fail to see the clear threat in front of their nose. You might have heard of black swans: low-probability, high-impact threats. Well, the opposite kind of threats are called gray rhinos: obvious dangers that we fail to see because of our mental blindspots. The scientific name for these blindspots is cognitive biases, which cause leaders to resist best practices in transitioning to a hybrid-first model.
The core idea is to get all of your workforce to pull together to achieve business outcomes: the location doesn’t matter.
Leaders can address this by focusing on a shared culture of “Excellence From Anywhere.” This term refers to a flexible organizational culture that takes into account the nature of an employee's work and promotes evaluating employees based on task completion, allowing remote work whenever possible.
Addressing Resentments Due to Proximity Bias
The “Excellence From Anywhere” strategy addresses concerns about treatment of remote workers by focusing on deliverables, regardless of where you work. Doing so also involves adopting best practices for hybrid and remote collaboration and innovation.
By valuing deliverables, collaboration, and innovation through a focus on a shared work culture of “Excellence From Anywhere,” you can instill in your employees a focus on deliverables. The core idea is to get all of your workforce to pull together to achieve business outcomes: the location doesn’t matter.
This work culture addresses concerns about fairness by reframing the conversation to focus on accomplishing shared goals, rather than the method of doing so. After all, no one wants their colleagues to have to commute out of spite.
This technique appeals to the tribal aspect of our brains. We are evolutionarily adapted to living in small tribal groups of 50-150 people. Spending different amounts of time in the office splits apart the work tribe into different tribes. However, cultivating a shared focus on business outcomes helps mitigate such divisions and create a greater sense of unity, alleviating frustrations and resentments. Doing so helps improve employee emotional wellbeing and facilitates good collaboration.
Solving the facetime concerns of proximity bias
But what about facetime with the boss? To address this problem necessitates shifting from the traditional, high-stakes, large-scale quarterly or even annual performance evaluations to much more frequent weekly or biweekly, low-stakes, brief performance evaluation through one-on-one in-person or videoconference check-ins.
Supervisees agree with their supervisor on three to five weekly or biweekly performance goals. Then, 72 hours before their check-in meeting, they send a brief report, under a page, to their boss of how they did on these goals, what challenges they faced and how they overcame them, a quantitative self-evaluation, and proposed goals for next week. Twenty-four hours before the meeting, the supervisor responds in a paragraph-long response with their initial impressions of the report.
It’s hard to tell how much any employee should worry about not being able to chat by the watercooler with their boss: knowing exactly where they stand is the key concern for employees, and they can take proactive action if they see their standing suffer.
At the one-on-one, the supervisor reinforces positive aspects of performance and coaches the supervisee on how to solve challenges better, agrees or revises the goals for next time, and affirms or revises the performance evaluation. That performance evaluation gets fed into a constant performance and promotion review system, which can replace or complement a more thorough annual evaluation.
This type of brief and frequent performance evaluation meeting ensures that the employee’s work is integrated with efforts by the supervisor’s other employees, thereby ensuring more unity in achieving business outcomes. It also mitigates concerns about facetime, since all get at least some personalized attention from their team leader. But more importantly, it addresses the underlying concerns about career mobility by giving all staff a clear indication of where they stand at all times. After all, it’s hard to tell how much any employee should worry about not being able to chat by the watercooler with their boss: knowing exactly where they stand is the key concern for employees, and they can take proactive action if they see their standing suffer.
Such best practices help integrate employees into a work culture fit for the future of work while fostering good relationships with managers. Research shows supervisor-supervisee relationships are the most critical ones for employee wellbeing, engagement, and retention.
Conclusion
You don’t have to be the CEO to implement these techniques. Lower-level leaders of small rank-and-file teams can implement these shifts within their own teams, adapting their culture and performance evaluations. And if you are a staff member rather than a leader, send this article to your supervisor and other employees at your company: start a conversation about the benefits of addressing proximity bias using such research-based best practices.
Scientists at Baylor College of Medicine developed a vaccine called Corbevax that, unlike mRNA vaccines, can be mass produced using technology already in place in low- and middle-income countries. It's now being administered in India to children aged 12-14.
When the COVID-19 pandemic began invading the world in late 2019, Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. The scientists, with their prior experience of developing inexpensive vaccines for the world’s poor, had anticipated that the global rollout of Covid-19 jabs would be marked with several inequities. They wanted to create a patent-free vaccine to bridge this gap, but the U.S. government did not seem impressed, forcing the researchers to turn to private philanthropies for funds.
Hotez and Bottazzi, both scientists at the Texas Children’s Hospital Center for Vaccine Development at Baylor College of Medicine, raised about $9 million in private funds. Meanwhile, the U.S. government’s contribution stood at $400,000.
“That was a very tough time early on in the pandemic, you know, trying to do the work and raise the money for it at the same time,” says Hotez, who was nominated in February for a Nobel Peace Prize with Bottazzi for their COVID-19 vaccine. He adds that at the beginning of the pandemic, governments emphasized speed, innovation and rapidly immunizing populations in North America and Europe with little consideration for poorer countries. “We knew this [vaccine] was going to be the answer to global vaccine inequality, but I just wish the policymakers had felt the same,” says Hotez.
Over the past two years, the world has witnessed 488 million COVID-19 infections and over 61 million deaths. Over 11 billion vaccine doses have been administered worldwide; however, the global rollout of COVID-19 vaccines is marked with alarming socio-economic inequities. For instance, 72 percent of the population in high-income countries has received at least one dose of the vaccine, whereas the number stands at 15 percent in low-income countries.
This inequity is worsening vulnerabilities across the world, says Lawrence Young, a virologist and co-lead of the Warwick Health Global Research Priority at the UK-based University of Warwick. “As long as the virus continues to spread and replicate, particularly in populations who are under-vaccinated, it will throw up new variants and these will remain a continual threat even to those countries with high rates of vaccination,” says Young, “Therefore, it is in all our interests to ensure that vaccines are distributed equitably across the world.”
“When your house is on fire, you don't call the patent attorney,” says Hotez. “We wanted to be the fire department.”
The vaccine developed by Hotez and Bottazzi recently received emergency use authorisation in India, which plans to manufacture 100 million doses every month. Dubbed ‘Corbevax’ by its Indian maker, Biological E Limited, the vaccine is now being administered in India to children aged 12-14. The patent-free arrangement means that other low- and middle-income countries could also produce and distribute the vaccine locally.
“When your house is on fire, you don't call the patent attorney, you call the fire department,” says Hotez, commenting on the intellectual property rights waiver. “We wanted to be the fire department.”
The Inequity
Vaccine equity simply means that all people, irrespective of their location, should have equal access to vaccines. However, data suggests that the global COVID-19 vaccine rollout has favoured those in richer countries. For instance, high-income countries like the UAE, Portugal, Chile, Singapore, Australia, Malta, Hong Kong and Canada have partially vaccinated over 85 percent of their populations. This percentage in poorer countries, meanwhile, is abysmally low – 2.1 percent in Yemen, 4.6 in South Sudan, 5 in Cameroon, 9.9 in Burkina Faso, 10 in Nigeria, 12 in Somalia, 12 in Congo, 13 in Afghanistan and 21 in Ethiopia.

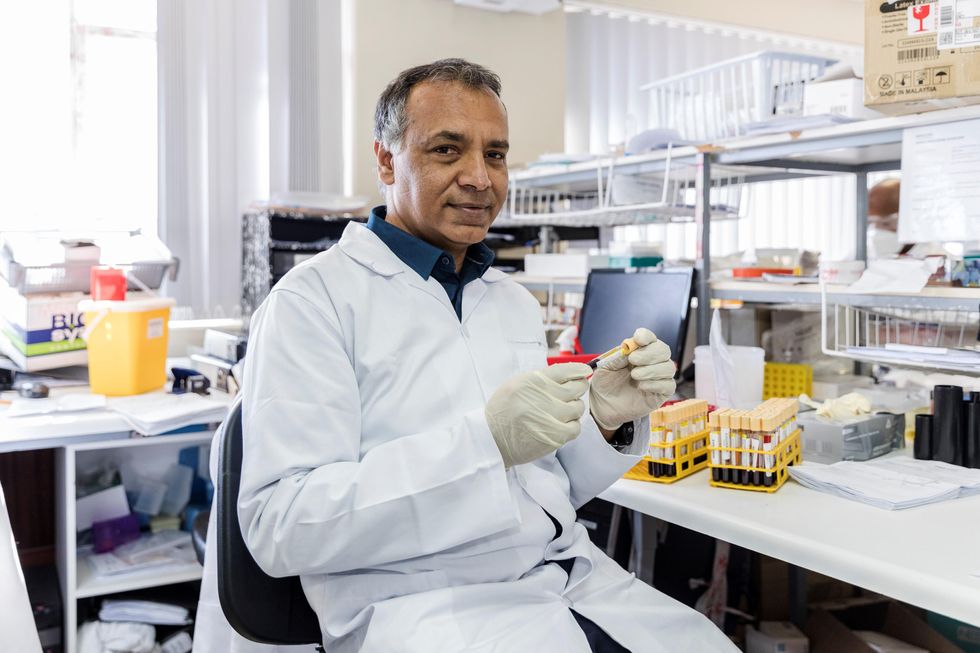
In late 2019, scientists Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. In February, they were nominated for a Nobel Peace Prize.
Texas Children's Hospital
The COVID-19 vaccination coverage is particularly low in African countries, and according to Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of African Local Initiative for Vaccinology Expertise, vaccine access and inequity remains a challenge in Africa. Madhi adds that a lack of vaccine access has affected the pandemic’s trajectory on the continent, but a majority of its people have now developed immunity through natural infection. “This has come at a high cost of loss of lives,” he says.
COVID-19 vaccines mean a significant financial burden for poorer countries, which spend an average of $41 per capita annually on health, while the average cost of every COVID-19 vaccine dose ranges between $2 and $40 in addition to a distribution cost of $3.70 per person for two doses. In December last year, the World Health Organisation (WHO) set a goal of immunizing 70 percent of the population of all countries by mid-2022. This, however, means that low-income countries would have to increase their health expenditure by an average of 56.6 percent to cover the cost, as opposed to 0.8 per cent in high-income countries.
Reflecting on the factors that have driven global inequity in COVID-19 vaccine distribution, Andrea Taylor, assistant director of programs at the Duke Global Health Innovation Center, says that wealthy nations took the risk of investing heavily in the development and scaling up of COVID-19 vaccines – at a time when there was little evidence to show that vaccines would work. This reserved a place for these nations at the front of the queue when doses started rolling off production lines. Lower-income countries, meanwhile, could not afford such investments.
“Now, however, global supply is not the issue,” says Taylor. “We are making plenty of doses to meet global need. The main problem is infrastructure to get the vaccine where it is most needed in a predictable and timely way and to ensure that countries have all the support they need to store, transport, and use the vaccine once it is received.”

Taufique Joarder, vice-chairperson of Bangladesh's Public Health Foundation, sees the need for more trials and data before Corbevax is made available to the general population.
In addition to global inequities in vaccination coverage, there are inequities within nations. Taufique Joarder, vice-chairperson of Bangladesh’s Public Health Foundation, points to the situation in his country, where vaccination coverage in rural and economically disadvantaged communities has suffered owing to weak vaccine-promotion initiatives and the difficulty many people face in registering online for jabs.
Joarder also cites the example of the COVID-19 immunization drive for children aged 12 years and above. “[Children] are given the Pfizer vaccine, which requires an ultralow temperature for storage. This is almost impossible to administer in many parts of the country, especially the rural areas. So, a large proportion of the children are being left out of vaccination,” says Joarder, adding that Corbevax, which is cheaper and requires regular temperature refrigeration “can be an excellent alternative to Pfizer for vaccinating rural children.”
Corbevax vs. mRNA Vaccines
As opposed to most other COVID-19 vaccines, which use the new Messenger RNA (mRNA) vaccine technology, Corbevax is an “old school” vaccine, says Hotez. The vaccine is made through microbial fermentation in yeast, similar to the process used to produce the recombinant hepatitis B vaccine, which has been administered to children in several countries for decades. Hence, says Hotez, the technology to produce Corbevax at large scales is already in place in countries like Vietnam, Bangladesh, India, Indonesia, Brazil, Argentina, among many others.
“So if you want to rapidly develop and produce and empower low- and middle-income countries, this is the technology to do it,” he says.
“Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines," says Andrea Taylor.
The COVID-19 vaccines created by Pfizer-BioNTech and Moderna marked the first time that mRNA vaccine technology was approved for use. However, scientists like Young feel that there is “a need to be pragmatic and not seduced by new technologies when older, tried and tested approaches can also be effective.” Taylor, meanwhile, says that although mRNA vaccines have dominated the COVID-19 vaccine market in the U.S., “there is no clear grounding for this preference in the data we have so far.” She adds that there is also growing evidence that the immunity from these shots may not hold up as well over time as that of vaccines using different platforms.
“The mRNA vaccines are well suited to wealthy countries with sufficient ultra-cold storage and transportation infrastructure, but these vaccines are divas and do not travel well in the rest of the world,” says Taylor. “Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines, such as the protein subunit platform used by Novavax and Corbevax. These require only standard refrigeration, can be manufactured using existing facilities all over the world, and are easy to transport.”
Joarder adds that Corbevax is cheaper due to the developers’ waived intellectual rights. It could also be used as a booster vaccine in Bangladesh, where only five per cent of the population has currently received booster doses. “If this vaccine is proved effective for heterologous boosting, [meaning] it works well and is well tolerated as a booster with other vaccines that are available in Bangladesh, this can be useful,” says Joarder.
According to Hotez, Corbevax can play several important roles - as a standalone adult or paediatric vaccine, and as a booster for other vaccines. Studies are underway to determine Corbevax’s effectiveness in these regards, he says.
Need for More Data
Biological E conducted two clinical trials involving 3000 subjects in India, and found Corbevax to be “safe and immunogenic,” with 90 percent effectiveness in preventing symptomatic infections from the original strain of COVID-19 and over 80 percent effectiveness against the Delta variant. The vaccine is currently in use in India, and according to Hotez, it’s in the pipeline at different stages in Indonesia, Bangladesh and Botswana.
However, Corbevax is yet to receive emergency use approval from the WHO. Experts such as Joarder see the need for more trials and data before it is made available to the general population. He says that while the WHO’s emergency approval is essential for global scale-up of the vaccine, we need data to determine age-stratified efficacy of the vaccine and whether it can be used for heterologous boosting with other vaccines. “According to the most recent data, the 100 percent circulating variant in Bangladesh is Omicron. We need to know how effective is Corbevax against the Omicron variant,” says Joarder.
Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of the African Local Initiative for Vaccinology Expertise, says that a majority of people in Africa have now developed immunity through natural infection. “This has come at a high cost of loss of lives."
Shivan Parusnath
Others, meanwhile, believe that availing vaccines to poorer countries is not enough to resolve the inequity. Young, the Warwick virologist, says that the global vaccination rollout has also suffered from a degree of vaccine hesitancy, echoing similar observations by President Biden and Pfizer’s CEO. The problem can be blamed on poor communication about the benefits of vaccination. “The Corbevax vaccine [helps with the issues of] patent protection, vaccine storage and distribution, but governments need to ensure that their people are clearly informed.” Notably, however, some research has found higher vaccine willingness in lower-income countries than in the U.S.
Young also emphasized the importance of establishing local vaccination stations to improve access. For some countries, meanwhile, it may be too late. Speaking about the African continent, Madhi says that Corbevax has arrived following the peak of the crisis and won’t reverse the suffering and death that has transpired because of vaccine hoarding by high-income countries.
“The same goes for all the sudden donations from countries such as France - pretty much of little to no value when the pandemic is at its tail end,” says Madhi. “This, unfortunately, is a repeat of the swine flu pandemic in 2009, when vaccines only became available to Africa after the pandemic had very much subsided.”

