How 30 Years of Heart Surgeries Taught My Dad How to Live
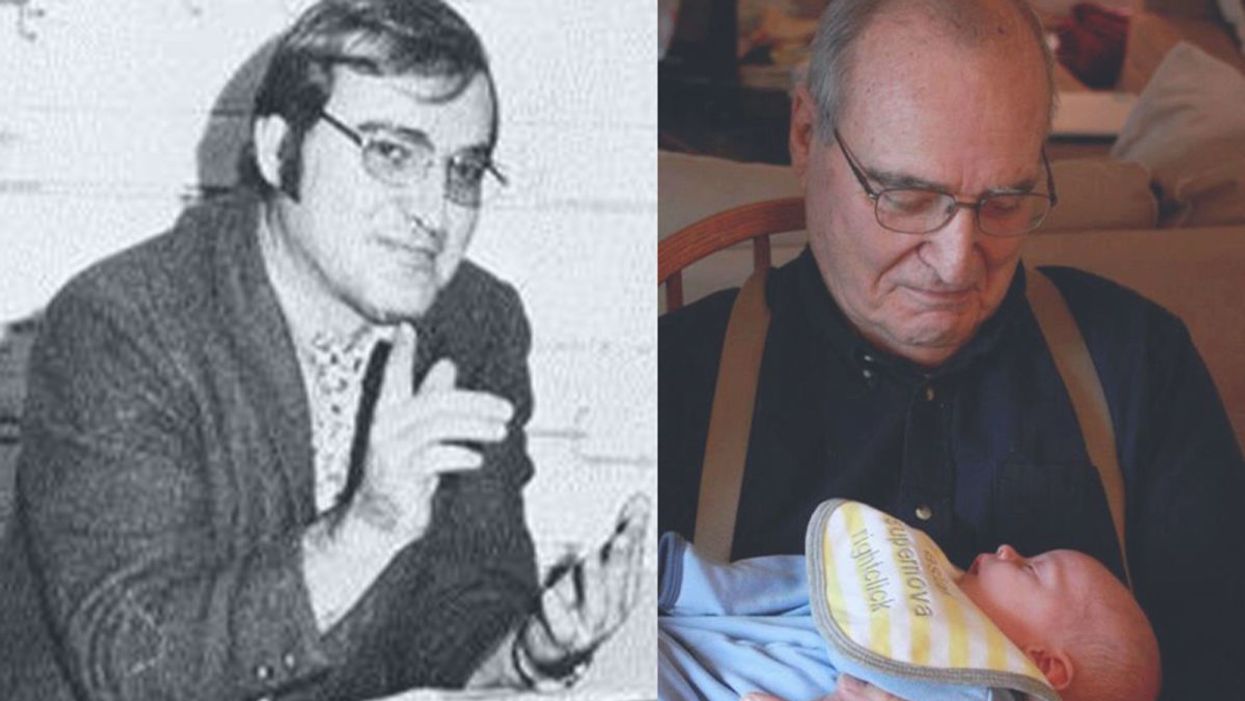
A mid-1970s photo of the author's father, and him holding a grandchild in 2012.
[Editor's Note: This piece is the winner of our 2019 essay contest, which prompted readers to reflect on the question: "How has an advance in science or medicine changed your life?"]
My father did not expect to live past the age of 50. Neither of his parents had done so. And he also knew how he would die: by heart attack, just as his father did.
In July of 1976, he had his first heart attack, days before his 40th birthday.
My dad lived the first 40 years of his life with this knowledge buried in his bones. He started smoking at the age of 12, and was drinking before he was old enough to enlist in the Navy. He had a sarcastic, often cruel, sense of humor that could drive my mother, my sister and me into tears. He was not an easy man to live with, but that was okay by him - he didn't expect to live long.
In July of 1976, he had his first heart attack, days before his 40th birthday. I was 13, and my sister was 11. He needed quadruple bypass surgery. Our small town hospital was not equipped to do this type of surgery; he would have to be transported 40 miles away to a heart center. I understood this journey to mean that my father was seriously ill, and might die in the hospital, away from anyone he knew. And my father knew a lot of people - he was a popular high school English teacher, in a town with only three high schools. He knew generations of students and their parents. Our high school football team did a blood drive in his honor.

During a trip to Disney World in 1974, Dad was suffering from angina the entire time but refused to tell me (left) and my sister, Kris.
Quadruple bypass surgery in 1976 meant that my father's breastbone was cut open by a sternal saw. His ribcage was spread wide. After the bypass surgery, his bones would be pulled back together, and tied in place with wire. The wire would later be pulled out of his body when the bones knitted back together. It would take months before he was fully healed.
Dad was in the hospital for the rest of the summer and into the start of the new school year. Going to visit him was farther than I could ride my bicycle; it meant planning a trip in the car and going onto the interstate. The first time I was allowed to visit him in the ICU, he was lying in bed, and then pushed himself to sit up. The heart monitor he was attached to spiked up and down, and I fainted. I didn't know that heartbeats change when you move; television medical dramas never showed that - I honestly thought that I had driven my father into another heart attack.
Only a few short years after that, my father returned to the big hospital to have his heart checked with a new advance in heart treatment: a CT scan. This would allow doctors to check for clogged arteries and treat them before a fatal heart attack. The procedure identified a dangerous blockage, and my father was admitted immediately. This time, however, there was no need to break bones to get to the problem; my father was home within a month.
During the late 1970's, my father changed none of his habits. He was still smoking, and he continued to drink. But now, he was also taking pills - pills to manage the pain. He would pop a nitroglycerin tablet under his tongue whenever he was experiencing angina (I have a vivid memory of him doing this during my driving lessons), but he never mentioned that he was in pain. Instead, he would snap at one of us, or joke that we were killing him.
I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count.
Being the kind of guy he was, my father never wanted to talk about his health. Any admission of pain implied that he couldn't handle pain. He would try to "muscle through" his angina, as if his willpower would be stronger than his heart muscle. His efforts would inevitably fail, leaving him angry and ready to lash out at anyone or anything. He would blame one of us as a reason he "had" to take valium or pop a nitro tablet. Dinners often ended in shouts and tears, and my father stalking to the television room with a bottle of red wine.
In the 1980's while I was in college, my father had another heart attack. But now, less than 10 years after his first, medicine had changed: our hometown hospital had the technology to run dye through my father's blood stream, identify the blockages, and do preventative care that involved statins and blood thinners. In one case, the doctors would take blood vessels from my father's legs, and suture them to replace damaged arteries around his heart. New advances in cholesterol medication and treatments for angina could extend my father's life by many years.
My father decided it was time to quit smoking. It was the first significant health step I had ever seen him take. Until then, he treated his heart issues as if they were inevitable, and there was nothing that he could do to change what was happening to him. Quitting smoking was the first sign that my father was beginning to move out of his fatalistic mindset - and the accompanying fatal behaviors that all pointed to an early death.
In 1986, my father turned 50. He had now lived longer than either of his parents. The habits he had learned from them could be changed. He had stopped smoking - what else could he do?
It was a painful decade for all of us. My parents divorced. My sister quit college. I moved to the other side of the country and stopped speaking to my father for almost 10 years. My father remarried, and divorced a second time. I stopped counting the number of times he was in and out of the hospital with heart-related issues.
In the early 1990's, my father reached out to me. I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count. He traveled across the country to spend a week with me, to meet my friends, and to rebuild his relationship with me. He did the same with my sister. He stopped drinking. He was more forthcoming about his health, and admitted that he was taking an antidepressant. His humor became less cruel and sadistic. He took an active interest in the world. He became part of my life again.
The 1990's was also the decade of angioplasty. My father explained it to me like this: during his next surgery, the doctors would place balloons in his arteries, and inflate them. The balloons would then be removed (or dissolve), leaving the artery open again for blood. He had several of these surgeries over the next decade.
When my father was in his 60's, he danced at with me at my wedding. It was now 10 years past the time he had expected to live, and his life was transformed. He was living with a woman I had known since I was a child, and my wife and I would make regular visits to their home. My father retired from teaching, became an avid gardener, and always had a home project underway. He was a happy man.

Dancing with my father at my wedding in 1998.
Then, in the mid 2000's, my father faced another serious surgery. Years of arterial surgery, angioplasty, and damaged heart muscle were taking their toll. He opted to undergo a life-saving surgery at Cleveland Clinic. By this time, I was living in New York and my sister was living in Arizona. We both traveled to the Midwest to be with him. Dad was unconscious most of the time. We took turns holding his hand in the ICU, encouraging him to regain his will to live, and making outrageous threats if he didn't listen to us.
The nursing staff were wonderful. I remember telling them that my father had never expected to live this long. One of the nurses pointed out that most of the patients in their ward were in their 70's and 80's, and a few were in their 90's. She reminded me that just a decade earlier, most hospitals were unwilling to do the kind of surgery my father had received on patients his age. In the first decade of the 21st century, however, things were different: 90-year-olds could now undergo heart surgery and live another decade. My father was on the "young" side of their patients.
The Cleveland Clinic visit would be the last major heart surgery my father would have. Not that he didn't return to his local hospital a few times after that: he broke his neck -- not once, but twice! -- slipping on ice. And in the 2010's, he began to show signs of dementia, and needed more home care. His partner, who had her own health issues, was not able to provide the level of care my father needed. My sister invited him to move in with her, and in 2015, I traveled with him to Arizona to get him settled in.
After a few months, he accepted home hospice. We turned off his pacemaker when the hospice nurse explained to us that the job of a pacemaker is to literally jolt a patient's heart back into beating. The jolts were happening more and more frequently, causing my Dad additional, unwanted pain.

My father in 2015, a few months before his death.
My father died in February 2016. His body carried the scars and implants of 30 years of cardiac surgeries, from the ugly breastbone scar from the 1970's to scars on his arms and legs from borrowed blood vessels, to the tiny red circles of robotic incisions from the 21st century. The arteries and veins feeding his heart were a patchwork of transplanted leg veins and fragile arterial walls pressed thinner by balloons.
And my father died with no regrets or unfinished business. He died in my sister's home, with his long-time partner by his side. Medical advancements had given him the opportunity to live 30 years longer than he expected. But he was the one who decided how to live those extra years. He was the one who made the years matter.
Can Radical Transparency Overcome Resistance to COVID-19 Vaccines?
Secretive panels of independent experts called Data Safety and Monitoring Boards examine clinical trials' data for safety and efficacy.
When historians look back on the COVID-19 pandemic, they may mark November 9, 2020 as the day the tide began to turn. That's when the New York-based pharmaceutical giant Pfizer announced that clinical trials showed its experimental vaccine, developed with the German firm BioNTech, to be 90 percent effective in preventing the disease.
A week later, Massachusetts biotech startup Moderna declared its vaccine to be 95 percent effective. By early December, Great Britain had begun mass inoculations, followed—once the Food and Drug Administration gave the thumbs-up—by the United States. In this scenario, the worst global health crisis in a century was on the cusp of resolution.
Yet future chroniclers may instead peg November 9 as the day false hope dawned. That could happen if serious safety issues, undetected so far, arise after millions of doses are administered. Experts consider it unlikely, however, that such problems alone (as opposed to the panic they might spark) would affect enough people to thwart a victory over the coronavirus. A more immediate obstacle is vaccine hesitancy—the prospect that much of the populace will refuse to roll up their sleeves.
To achieve "herd immunity" for COVID-19 (the point at which a vaccine reduces transmission rates enough to protect those who can't or won't take it, or for whom it doesn't work), epidemiologists estimate that up to 85 percent of the population will have to be vaccinated. Alarmingly, polls suggest that 40 to 50 percent of Americans intend to decline, judging the risks to be more worrisome than those posed by the coronavirus itself.
COVID vaccine skeptics occupy various positions on a spectrum of doubt. Some are committed anti-vaxxers, or devotees of conspiracy theories that view the pandemic as a hoax. Others belong to minority groups that have historically been used as guinea pigs in unethical medical research (for horrific examples, Google "Tuskegee syphilis experiment" or "Henrietta Lacks"). Still others simply mistrust Big Pharma and/or Big Government. A common fear is that the scramble to find a vaccine—intensified by partisan and profit motives—has led to corner-cutting in the testing and approval process. "They really rushed," an Iowa trucker told The Washington Post. "I'll probably wait a couple of months after they start to see how everyone else is handling it."
The COVID crisis has spurred calls for secretive Data Safety and Monitoring Boards to come out of the shadows.
The consensus among scientists, by contrast, is that the process has been rigorous enough, given the exigency of the situation, that the public can feel reasonably confident in any vaccine that has earned the imprimatur of the FDA. For those of us who share that assessment, finding ways to reassure the hesitant-but-persuadable is an urgent matter.
Vax-positive public health messaging is one obvious tactic, but a growing number of experts say it's not enough. They prescribe a regimen of radical transparency throughout the system that regulates research—in particular, regarding the secretive panels that oversee vaccine trials.
The Crucial Role of the Little-Known Panels
Like other large clinical trials involving potentially high-demand or controversial products, studies of COVID-19 vaccines in most countries are supervised by groups of independent observers. Known in the United States as data safety and monitoring boards (DSMBs), and elsewhere as data monitoring committees, these panels consist of scientists, clinicians, statisticians, and other authorities with no ties to the sponsor of the study.
The six trials funded by the federal program known as Operation Warp Speed (including those of newly approved Moderna and frontrunner AstraZeneca) share a DSMB, whose members are selected by the National Institutes of Health; other companies (including Pfizer) appoint their own. The panel's job is to monitor the safety and efficacy of a treatment while the trial is ongoing, and to ensure that data is being collected and analyzed correctly.
Vaccine studies are "double-blinded," which means neither the participants nor the doctors running the trial know who's getting the real thing and who's getting a placebo. But the DSMB can access that information if a study volunteer has what might be a serious side effect—and if the participant was in the vaccine group, the board can ask that the trial be paused for further investigation.
The DSMB also checks for efficacy at pre-determined intervals. If it finds that the vaccine group and the placebo group are getting sick at similar rates, the panel can recommend stopping the trial due to "futility." And if the results look overwhelmingly positive, the DSMB can recommend that the study sponsor apply for FDA approval before the scheduled end of the trial, in order to hurry the product to market.
With this kind of inside dope and high-level influence, DSMBs could easily become targets for outside pressure. That's why, since the 1980s, their membership has typically been kept secret.
During the early days of the AIDS crisis, researchers working on HIV drugs feared for the safety of the experts on their boards. "They didn't want them to be besieged and harassed by members of the community," explains Susan Ellenberg, a professor of biostatistics, medical ethics and health policy at the University of Pennsylvania, and co-author of Data Monitoring Committees in Clinical Trials, the DSMB bible. "You can understand why people would very much want to know how things were looking in a given trial. They wanted to save their own lives; they wanted to save their friends' lives." Ellenberg, who was founding director of the biostatistics branch of the AIDS division at the National Institute of Allergy and Infectious Diseases (NIAID), helped shape a range of policies designed to ensure that DSMBs made decisions based on data and nothing else.
Confidentiality also shields DSMB members from badgering by patient advocacy groups, who might urge that a drug be presented for approval before trial results are conclusive, or by profit-hungry investors. "It prevents people from trying to pry out information to get an edge in the stock market," says Art Caplan, a bioethicist at New York University.
Yet the COVID crisis has spurred calls for DSMBs to come out of the shadows. One triggering event came in March 2020, when the FDA approved hydroxychloroquine for COVID-19—a therapy that President Donald J. Trump touted, despite scant evidence for its efficacy. (Approval was rescinded in June.) If the agency could bow to political pressure on these medications, critics warned, it might do so with vaccines as well. In the end, that didn't happen; the Pfizer approval was issued well after Election Day, despite Trump's goading, and most experts agree that it was based on solid science. Still, public suspicion lingers.
Another shock came in September, after British-based AstraZeneca announced it was pausing its vaccine trial globally due to a "suspected adverse rection" in a volunteer. The company shared no details with the press. Instead, AstraZeneca's CEO divulged them in a private call with J.P. Morgan investors the next day, confirming that the volunteer was suffering from transverse myelitis, a rare and serious spinal inflammation—and that the study had also been halted in July, when another volunteer displayed neurological symptoms. STAT News broke the story after talking to tipsters.
Although both illnesses were found to be unrelated to the vaccine, and the trial was restarted, the incident had a paradoxical effect: while it confirmed for experts that the oversight system was working, AstraZeneca's initial lack of candor added to many laypeople's sense that it wasn't. "If you were seeking to undermine trust, that's kind of how you would go about doing it," says Charles Weijer, a bioethicist at Western University in Ontario, who has helped develop clinical trial guidelines for the World Health Organization.
Both Caplan and Weijer have served on many DSMBs; they believe the boards are generally trustworthy, and that those overseeing COVID vaccine trials are performing their jobs well. But the secrecy surrounding these groups, they and others argue, has become counterproductive. Shining a light on the statistical sausage-makers would help dispel doubts about the finished product.
"I'm not suggesting that any of these companies are doing things unethically," Weijer explains. "But the circumstances of a global pandemic are sufficiently challenging that perhaps they ought to be doing some things differently. I believe it would be trust-producing for data monitoring committees to be more forthcoming than usual."
Building Trust: More Transparency
Just how forthcoming is a matter of debate. Caplan suggests that each COVID vaccine DSMB reveal the name of its chair; that would enable the scientific community, as well as the media and the general public, to get a sense of the integrity and qualifications of the board as a whole while preserving the anonymity of the other members.
Indeed, when Operation Warp Speed's DSMB chair, Richard Whitley, was outed through a website slip-up, many observers applauded his selection for the role; a professor of pediatrics, microbiology, medicine and neurosurgery at the University of Alabama at Birmingham, he is "an exceptionally experienced and qualified individual," Weijer says. (Reporters with ProPublica later identified two other members: Susan Ellenberg and immunologist William Makgoba, known for his work on the South African AIDS Vaccine Initiative.)
Caplan would also like to see more details of the protocols DSMBs are using to make decisions, such as the statistical threshold for efficacy that would lead them to seek approval from the FDA. And he wishes the NIH would spell out specific responsibilities for these monitoring boards. "They don't really have clear, government-mandated charters," he notes. For example, there's no requirement that DSMBs include an ethicist or patient advocate—both of which Caplan considers essential for vaccine trials. "Rough guidelines," he says, "would be useful."
Weijer, for his part, thinks DSMBs should disclose all their members. "When you only disclose the chair, you leave questions unanswered," he says. "What expertise do [the others] bring to the table? Are they similarly free of relevant conflicts of interest? And it doesn't answer the question that will be foremost on many people's minds: are these people in the pocket of pharma?"
Weijer and Caplan both want to see greater transparency around the trial results themselves. Because the FDA approved the Pfizer and Moderna vaccines with emergency use authorizations rather than full licensure, which requires more extensive safety testing, these products reached the market without the usual paper trail of peer-reviewed publications. The same will likely be true of any future COVID vaccines that the agency greenlights. To add another level of scrutiny, both ethicists suggest, each company should publicly release its data at the end of a trial. "That offers the potential for academic groups to go in and do an analysis," Weijer explains, "to verify the claims about the safety and efficacy of the vaccine." The point, he says, is not only to ensure that the approval was justified, but to provide evidence to counter skeptics' qualms.
Caplan may differ on some of the details, but he endorses the premise. "It's all a matter of trust," he says. "You're always watching that, because a vaccine is only as good as the number of people who take it."
Scientists Attempt to Make Human Cells Resistant to Coronaviruses and Ebola
Scientists are experimenting with turning certain genes on and off to make cells better fight viral infection.
Under the electronic microscope, the Ebola particles looked like tiny round bubbles floating inside human cells. Except these Ebola particles couldn't get free from their confinement.
They were trapped inside their bubbles, unable to release their RNA into the human cells to start replicating. These cells stopped the Ebola infection. And they did it on their own, without any medications, albeit in a petri dish of immunologist Adam Lacy-Hulbert. He studies how cells fight infections at the Benaroya Research Institute in Seattle, Washington.
These weren't just any ordinary human cells. They had a specific gene turned on—namely CD74, which typically wouldn't be on. Lacy-Hulbert's team was experimenting with turning various genes on and off to see what made cells fight viral infections better. One particular form of the CD74 gene did the trick. Normally, the Ebola particles would use the cells' own proteases—enzymes that are often called "molecular scissors" because they slice proteins—to cut the bubbles open. But CD74 produced a protein that blocked the scissors from cutting the bubbles, leaving Ebola trapped.
"When that gene turns on, it makes the protein that interferes with Ebola replication," Lacy-Hulbert says. "The protein binds to those molecular scissors and stops them from working." Even better, the protein interfered with coronaviruses too, including SARS-CoV-2, as the team published in the journal Science.
This begs the question: If one can turn on cells' viral resistance in a lab, can this be done in a human body so we that we can better fight Ebola, coronaviruses and other viral scourges?
Recent research indeed shows that our ability to fight viral infections is written in our genes. Genetic variability is at least one reason why some coronavirus-infected people don't develop symptoms while others stay on ventilators for weeks—often due to the aberrant response of their immune system, which went on overdrive to kill the pathogen. But if cells activate certain genes early in the infection, they might successfully stop viruses from replicating before the immune system spirals out of control.
"If my father who is 70 years old tests positive, I would recommend he takes interferon as early as possible."
When we talk about fighting infections, we tend to think in terms of highly specialized immune system cells—B-cells that release antibodies and T-cells that stimulate inflammatory responses, says Lacy-Hulbert. But all other cells in the body have the ability to fight infections too via different means. When cells detect the presence of a pathogen, they release interferons—small protein molecules named so because they set off a genetic chain reaction that interferes with viral replication. These molecules work as alarm signals to other cells around them. The neighboring cells transduce these signals inside themselves and turn on genes responsible for cellular defenses.
"There are at least 300 to 400 genes that are stimulated by type I interferons," says professor Jean-Laurent Casanova at Rockefeller University.
Scientists don't yet know exactly what all of these genes do, but they change the molecular behavior of the cells. "The cells go into a dramatic change and start producing hundreds of proteins that interfere with viral replication on the inside," explains Qian Zhang, a researcher at Casanova's lab. "Some block the proteins the virus needs and some physically tether the virus."
Some cells produce only small amount of interferon, enough to alert their neighbors. Others, such microphages and monocytes, whose jobs are to detect foreign invaders, produce a lot, injecting interferons into the blood to sound the alarm throughout the body. "They are professional cells so their jobs [are] to detect a viral or bacterial infection," Zhang explains.
People with impaired interferon responses are more vulnerable to infections, including influenza and coronaviruses. In two recent studies published in the journal Science, Casanova, Zhang and their colleagues found that patients who lacked a certain type of interferon had more severe Covid-19 symptoms and some died from it. The team ran a genetic comparison of blood samples from patients hospitalized with severe coronavirus cases against those with the asymptomatic infections.
They found that people with severe disease had rare variants in the 13 genes responsible for interferon production. More than three percent of them had a genetic mutation resulting in non-functioning genes. And over ten percent had an autoimmune condition, in which misguided antibodies neutralized their interferons, dampening their bodies' defenses—and these patients were predominantly men. These discoveries help explain why some young and seemingly healthy individuals require life support, while others have mild symptoms or none. The findings also offer ways of stimulating cellular resistance.
A New Frontier in the Making
The idea of making human cells genetically resistant to infections—and possibly other stressors like cancer or aging—has been considered before. It is the concept behind the Genome Project-write or GP-write project, which aims to create "ultra-safe" versions of human cells that resist a variety of pathogens by way of "recoding" or rewriting the cells' genes.
To build proteins, cells use combinations of three DNA bases called codons to represent amino acids—the proteins' building blocks. But biologists find that many of the codons are redundant so if they were removed from all genes, the human cells would still make all their proteins. However, the viruses, whose genes would still include these eliminated redundant codons, would no longer successfully be able to replicate inside human cells.
In 2016, the GP-Write team successfully reduced the number of Escherichia coli's codons from 64 to 57. Recoding genes in all human cells would be harder, but some recoded cells may be transplanted into the body, says Harvard Medical School geneticist George Church, the GP-Write core founding member.
"You can recode a subset of the body, such as all of your blood," he says. "You can also grow an organ inside a recoded pig and transplant it."
Church adds that these methods are still in stages that are too early to help us with this pandemic.
LeapsMag exclusively interviewed Church in 2019 about his latest progress with DNA recoding:
The Push for Clinical Trials
In the meantime, interferons may prove an easier medicine. Lacy-Hulbert thinks that interferon gamma might play a role in activating the CD74 gene, which gums up the molecular scissors. There also may be other ways to activate that gene. "So we are now thinking, can we develop a drug that mimics that actual activity?" he says.
Some interferons are already manufactured and used for treating certain diseases, including multiple sclerosis. Theoretically, nothing prevents doctors from prescribing interferons to Covid patients, but it must be done in the early stages of infection—to stimulate genes that trigger cellular defenses before the virus invades too many cells and before the immune systems mobilizes its big guns.
"If my father who is 70 years old tests positive, I would recommend he takes interferon as early as possible," says Zhang. But to make it a mainstream practice, doctors need clear prescription guidelines. "What would really help doctors make these decisions is clinical trials," says Casanova, so that such guidelines can be established. "We are now starting to push for clinical trials," he adds.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

