How 30 Years of Heart Surgeries Taught My Dad How to Live
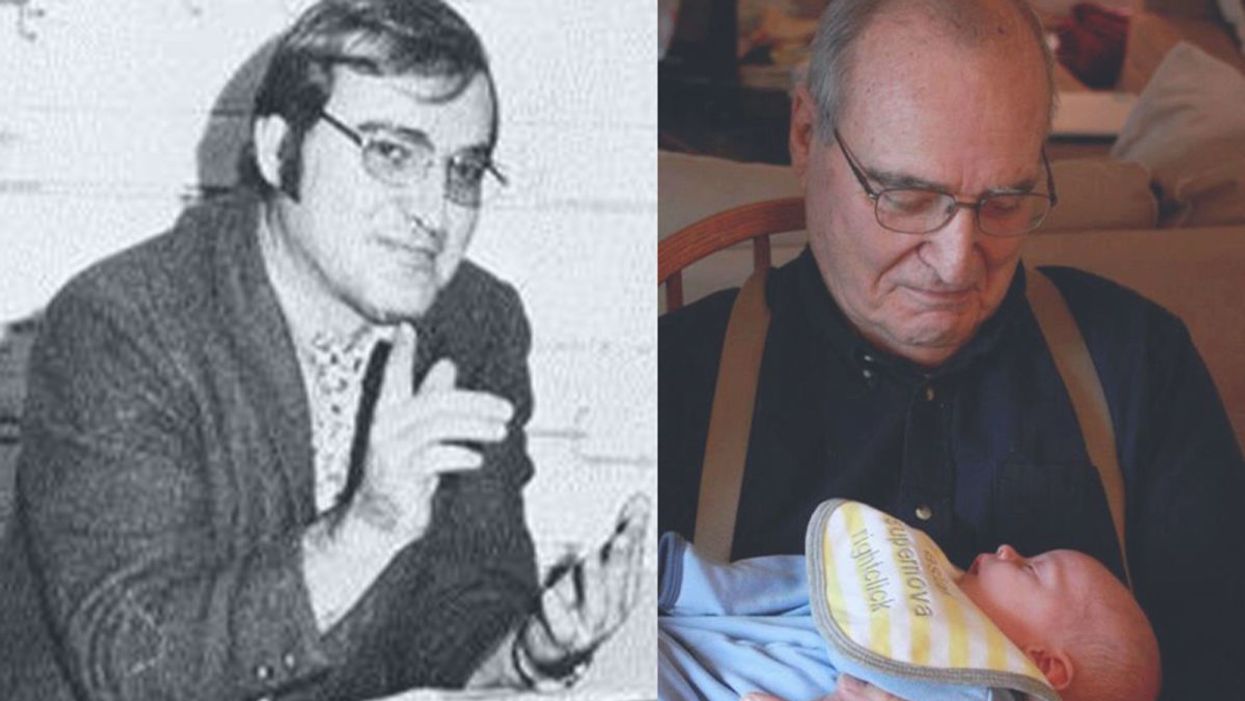
A mid-1970s photo of the author's father, and him holding a grandchild in 2012.
[Editor's Note: This piece is the winner of our 2019 essay contest, which prompted readers to reflect on the question: "How has an advance in science or medicine changed your life?"]
My father did not expect to live past the age of 50. Neither of his parents had done so. And he also knew how he would die: by heart attack, just as his father did.
In July of 1976, he had his first heart attack, days before his 40th birthday.
My dad lived the first 40 years of his life with this knowledge buried in his bones. He started smoking at the age of 12, and was drinking before he was old enough to enlist in the Navy. He had a sarcastic, often cruel, sense of humor that could drive my mother, my sister and me into tears. He was not an easy man to live with, but that was okay by him - he didn't expect to live long.
In July of 1976, he had his first heart attack, days before his 40th birthday. I was 13, and my sister was 11. He needed quadruple bypass surgery. Our small town hospital was not equipped to do this type of surgery; he would have to be transported 40 miles away to a heart center. I understood this journey to mean that my father was seriously ill, and might die in the hospital, away from anyone he knew. And my father knew a lot of people - he was a popular high school English teacher, in a town with only three high schools. He knew generations of students and their parents. Our high school football team did a blood drive in his honor.

During a trip to Disney World in 1974, Dad was suffering from angina the entire time but refused to tell me (left) and my sister, Kris.
Quadruple bypass surgery in 1976 meant that my father's breastbone was cut open by a sternal saw. His ribcage was spread wide. After the bypass surgery, his bones would be pulled back together, and tied in place with wire. The wire would later be pulled out of his body when the bones knitted back together. It would take months before he was fully healed.
Dad was in the hospital for the rest of the summer and into the start of the new school year. Going to visit him was farther than I could ride my bicycle; it meant planning a trip in the car and going onto the interstate. The first time I was allowed to visit him in the ICU, he was lying in bed, and then pushed himself to sit up. The heart monitor he was attached to spiked up and down, and I fainted. I didn't know that heartbeats change when you move; television medical dramas never showed that - I honestly thought that I had driven my father into another heart attack.
Only a few short years after that, my father returned to the big hospital to have his heart checked with a new advance in heart treatment: a CT scan. This would allow doctors to check for clogged arteries and treat them before a fatal heart attack. The procedure identified a dangerous blockage, and my father was admitted immediately. This time, however, there was no need to break bones to get to the problem; my father was home within a month.
During the late 1970's, my father changed none of his habits. He was still smoking, and he continued to drink. But now, he was also taking pills - pills to manage the pain. He would pop a nitroglycerin tablet under his tongue whenever he was experiencing angina (I have a vivid memory of him doing this during my driving lessons), but he never mentioned that he was in pain. Instead, he would snap at one of us, or joke that we were killing him.
I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count.
Being the kind of guy he was, my father never wanted to talk about his health. Any admission of pain implied that he couldn't handle pain. He would try to "muscle through" his angina, as if his willpower would be stronger than his heart muscle. His efforts would inevitably fail, leaving him angry and ready to lash out at anyone or anything. He would blame one of us as a reason he "had" to take valium or pop a nitro tablet. Dinners often ended in shouts and tears, and my father stalking to the television room with a bottle of red wine.
In the 1980's while I was in college, my father had another heart attack. But now, less than 10 years after his first, medicine had changed: our hometown hospital had the technology to run dye through my father's blood stream, identify the blockages, and do preventative care that involved statins and blood thinners. In one case, the doctors would take blood vessels from my father's legs, and suture them to replace damaged arteries around his heart. New advances in cholesterol medication and treatments for angina could extend my father's life by many years.
My father decided it was time to quit smoking. It was the first significant health step I had ever seen him take. Until then, he treated his heart issues as if they were inevitable, and there was nothing that he could do to change what was happening to him. Quitting smoking was the first sign that my father was beginning to move out of his fatalistic mindset - and the accompanying fatal behaviors that all pointed to an early death.
In 1986, my father turned 50. He had now lived longer than either of his parents. The habits he had learned from them could be changed. He had stopped smoking - what else could he do?
It was a painful decade for all of us. My parents divorced. My sister quit college. I moved to the other side of the country and stopped speaking to my father for almost 10 years. My father remarried, and divorced a second time. I stopped counting the number of times he was in and out of the hospital with heart-related issues.
In the early 1990's, my father reached out to me. I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count. He traveled across the country to spend a week with me, to meet my friends, and to rebuild his relationship with me. He did the same with my sister. He stopped drinking. He was more forthcoming about his health, and admitted that he was taking an antidepressant. His humor became less cruel and sadistic. He took an active interest in the world. He became part of my life again.
The 1990's was also the decade of angioplasty. My father explained it to me like this: during his next surgery, the doctors would place balloons in his arteries, and inflate them. The balloons would then be removed (or dissolve), leaving the artery open again for blood. He had several of these surgeries over the next decade.
When my father was in his 60's, he danced at with me at my wedding. It was now 10 years past the time he had expected to live, and his life was transformed. He was living with a woman I had known since I was a child, and my wife and I would make regular visits to their home. My father retired from teaching, became an avid gardener, and always had a home project underway. He was a happy man.

Dancing with my father at my wedding in 1998.
Then, in the mid 2000's, my father faced another serious surgery. Years of arterial surgery, angioplasty, and damaged heart muscle were taking their toll. He opted to undergo a life-saving surgery at Cleveland Clinic. By this time, I was living in New York and my sister was living in Arizona. We both traveled to the Midwest to be with him. Dad was unconscious most of the time. We took turns holding his hand in the ICU, encouraging him to regain his will to live, and making outrageous threats if he didn't listen to us.
The nursing staff were wonderful. I remember telling them that my father had never expected to live this long. One of the nurses pointed out that most of the patients in their ward were in their 70's and 80's, and a few were in their 90's. She reminded me that just a decade earlier, most hospitals were unwilling to do the kind of surgery my father had received on patients his age. In the first decade of the 21st century, however, things were different: 90-year-olds could now undergo heart surgery and live another decade. My father was on the "young" side of their patients.
The Cleveland Clinic visit would be the last major heart surgery my father would have. Not that he didn't return to his local hospital a few times after that: he broke his neck -- not once, but twice! -- slipping on ice. And in the 2010's, he began to show signs of dementia, and needed more home care. His partner, who had her own health issues, was not able to provide the level of care my father needed. My sister invited him to move in with her, and in 2015, I traveled with him to Arizona to get him settled in.
After a few months, he accepted home hospice. We turned off his pacemaker when the hospice nurse explained to us that the job of a pacemaker is to literally jolt a patient's heart back into beating. The jolts were happening more and more frequently, causing my Dad additional, unwanted pain.

My father in 2015, a few months before his death.
My father died in February 2016. His body carried the scars and implants of 30 years of cardiac surgeries, from the ugly breastbone scar from the 1970's to scars on his arms and legs from borrowed blood vessels, to the tiny red circles of robotic incisions from the 21st century. The arteries and veins feeding his heart were a patchwork of transplanted leg veins and fragile arterial walls pressed thinner by balloons.
And my father died with no regrets or unfinished business. He died in my sister's home, with his long-time partner by his side. Medical advancements had given him the opportunity to live 30 years longer than he expected. But he was the one who decided how to live those extra years. He was the one who made the years matter.
5 Key Questions to Consider Before Sending Your Child Back to School
Consider community, school district policies, family health, risks/benefits, and necessity of schools before making the difficult decision.
[Editor's Note: This essay is in response to our current Big Question, which we posed to several experts: "Under what circumstances would you send a child back to school, given that the virus is not going away anytime soon?"]
It is August. The start date of school is quickly approaching. Decisions must be made about whether to send our children back. As a physician, a public health researcher, and the mother of two school-aged children, I have few clear answers.
To add insult to injury, a spate of recent new data suggests that - as many of us suspected all along - kids are susceptible to COVID-19, they transmit COVID-19, and they can get really sick from COVID-19.
Let me start with the obvious. My kids, and all kids, deserve a safe, in-person school year. We know the data on the adverse effects of school closure on kids, particularly for those who are already vulnerable. I also know, on a personal level, that distance learning is no substitute for in-person schooling. Homeschooling may be great for those with the privilege to do it, but I - like many Americans - am unable to quit my job, and children need more than a screen to learn.
Moreover, safe school reopening should not be an impossible dream. I and many other physicians, teachers, and scientists have described the bare minimum that we need to safely reopen schools: a stable, low rate of COVID-19 in the community; funding and mandates for basic public health precautions (like universal masking and small, stable classes) in the schools; and easy access to testing for kids and teachers. This has been achieved, successfully, in other countries.
Unfortunately, the United States has squandered its opportunity to do right by families. Across our country, rates of COVID-19 are rising. Few states have been able to sustain a test positivity rate of less than 5 percent - the maximum that most of us, in the public health world, would tolerate. Delays in testing are rampant. Systemic under-funding of public schools means that many schools simply can't afford to put basic public health measures in place. Worst, science denialism (and the spread of quack conspiracy theories online) means that many communities are fighting even the most basic of safety precautions.
To add insult to injury, a spate of recent new data suggests that - as many of us suspected all along - kids are susceptible to COVID-19, they transmit COVID-19, and they can get really sick from COVID-19. This data increases the risk calculus. Our kids are not immune, and neither are we.
Given that the necessary societal interventions simply have not happened, most American families are therefore left making an individual choice: do I send my kid to school? Or not? There are five key questions for parents to ponder when making the difficult choice about what to do.
First, we must look at our community. Knowing that testing is difficult to obtain, a true estimate of community prevalence of COVID-19 is nearly impossible. But with a test positivity rate of more than 5 percent, it's safe to assume that in a school of 500 people, at least 1 will be positive for COVID-19. That is too high for safety. Whether or not the local government does the right thing, I would not send my child to in-person school if my community had these high rates of test positivity.
Second, we must look at our school district's policies. Will the school mandate masks? Are they cohorting students and teachers in small, stable groups? Do they have contact tracing and isolation policies in place for when a student or teacher inevitably tests positive? Do they have procedures to protect vulnerable teachers and staff? If not, I would not send my child to school. If the district is doing all of the above, I would consider it.
Third, we must look at the health profile of our own kids and families. If my child had chronic medical issues, or if I lived with my elderly parents or were myself at high risk of severe disease, I would not send my child to in-person school.
It is therefore unlikely that schools anywhere in the U.S. will be open by October.
Fourth, we must do the difficult, ethical weighing of the non-zero risk of infection (even in the safest communities) with the needs of our children. Even in low-prevalence states, there will be infections in the school setting. That said, the small risk of a severe infection may be outweighed by the social, emotional, and financial risk of keeping a child home. This decision must be made on a family-by-family basis. I know my answer; but I cannot provide this answer for others.
Finally, we must call attention to the fact that many kids and families have no options. There are far too many American children who literally depend on their school system for physical, nutritional, emotional, and academic safety. There are too many parents who have no way to earn an income and keep their kids safe without in-person learning. If anyone deserves to be prioritized for in-person schooling, it should be them. (And yes, we should also work to fix the social safety net that leaves these children high and dry.)
As I write this on August 2nd, 2020, I am planning to send my two children back to our public schools for in-person education. We have low rates of infection in our community, we have masking and stable cohorts in place, and my family is relatively healthy. We also depend on the schools to keep my children safe and engaged while I'm working in the ER! I will not hesitate, however, to pull my children out of school should any of these considerations change, if local test positivity rates go up, or if my children report that masking is not the norm in the classroom.
And sadly, I expect that this discussion will soon be a moot point. We continue to fail as a nation at basic public health policies. It is therefore unlikely that schools anywhere in the U.S. will be open by October. Our country has not shown the willpower to control the virus, leaving us all with, literally, no choice to make.
[Editor's Note: Here's the other essay in the Back to School series: Masks and Distancing Won't Be Enough to Prevent School Outbreaks, Latest Science Suggests.]
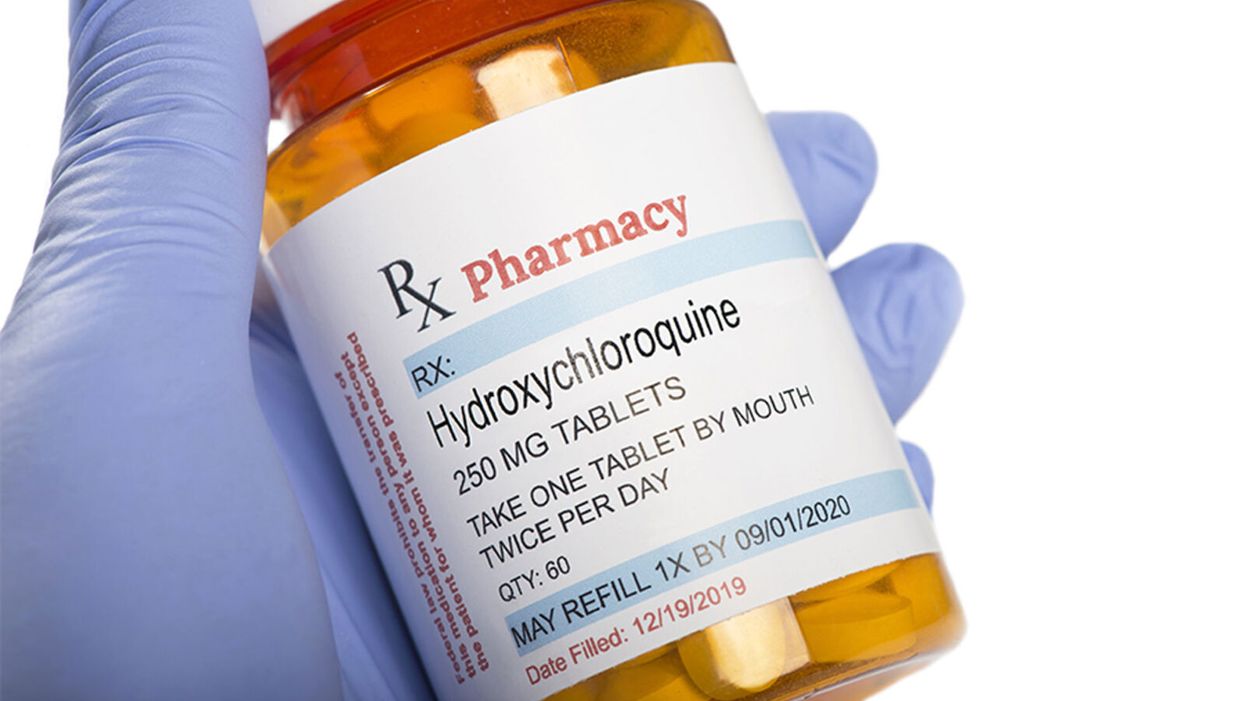
The Only Hydroxychloroquine Story You Need to Read
Hydroxychloroquine has been shown not to provide benefit for COVID-19 patients in multiple randomized controlled trials, despite continuous misinformation asserting its alleged effectiveness.
In the early days of a pandemic caused by a virus with no existing treatments, many different compounds are often considered and tried in an attempt to help patients.
It all relates back to a profound question: How do we know what we know?
Many of these treatments fall by the wayside as evidence accumulates regarding actual efficacy. At that point, other treatments become standard of care once their benefit is proven in rigorously designed trials.
However, about seven months into the pandemic, we're still seeing political resurrection of a treatment that has been systematically studied and demonstrated in well-designed randomized controlled trials to not have benefit.
The hydroxychloroquine (and by extension chloroquine) story is a complicated one that was difficult to follow even before it became infused with politics. It is a simple fact that these drugs, long approved by the Food and Drug Administration (FDA), work in Petri dishes against various viruses including coronaviruses. This set of facts provided biological plausibility to support formally studying their use in the clinical treatment and prevention of COVID-19. As evidence from these studies accumulates, it is a cognitive requirement to integrate that knowledge and not to evade it. This also means evaluating the rigor of the studies.
In recent days we have seen groups yet again promoting the use of hydroxychloroquine in, what is to me, a baffling disregard of the multiple recent studies that have shown no benefit. Indeed, though FDA-approved for other indications like autoimmune conditions and preventing malaria, the emergency use authorization for COVID-19 has been rescinded (which means the government cannot stockpile it). Still, however, many patients continue to ask for the drug, compelled by political commentary, viral videos, and anecdotal data. Yet most doctors (like myself) are refusing to write the prescriptions outside of a clinical trial – a position endorsed by professional medical organizations such as the American College of Physicians and the Infectious Diseases Society of America. Why this disconnect?
It all relates back to a profound question: How do we know what we know? In science, we use the scientific method – the process of observing reality, coming up with a hypothesis about what might be true, and testing that hypothesis as thoroughly as possible until we discover the objective truth.
The confusion we're seeing now stems from an inability to distinguish between anecdotes reported by physicians (observational data) and an actual evidence base. This is understandable among the general public but when done by a healthcare professional, it reveals a disdain for reason, logic, and the scientific method.
The Difference Between Observational Data and Randomized Controlled Trials
The power of informal observation is crucial. It is part of the scientific method but primarily as a basis for generating hypotheses that we can test. How do we conduct medical tests? The gold standard is the double-blind, randomized, placebo-controlled trial. This means that neither the researchers nor the volunteers know who is getting a drug and who is getting a sugar pill. Then both groups of the trial, called arms, can be compared to determine whether the people who got the drug fared better. This study design prevents biases and the placebo effect from confounding the data and undermining the veracity of the results.
For example, a seemingly beneficial effect might be seen in an observational study with no blinding and no control group. In such a case, all patients are openly given the drug and their doctors observe how they do. A prime example is the 36-patient single-arm study from France that generated a tremendous amount of interest after President Trump tweeted about it. But this kind of a study by its nature cannot answer the critical question: Was the positive effect because of hydroxychloroquine or just the natural course of the illness? In other words, would someone have recovered in a similar fashion regardless of the drug? What is the role of the placebo effect?
These are reasons why it is crucial to give a placebo to a control group that is as similar in every respect as possible to those receiving the intervention. Then we attempt to find out by comparing the two groups: What is the side effect profile of the drug? Are the groups large enough to detect a relatively rare safety concern? How long were the patients followed for? Was something else responsible for making the patients get better, such as the use of steroids (as likely was the case in the Henry Ford study)?
Looking at the two major hydroxychloroquine trials, it is apparent that, when studied using the best tools of clinical trials, no benefit is likely to occur.
All of these considerations amount to just a fraction of the questions that can be answered more definitively in a well-designed large randomized controlled trial than in observational studies. Indeed, an observational study from New York failed to show any benefit in hospitalized patients, showing how unclear and disparate the results can be with these types of studies. A New York retrospective study (which examined patient outcomes after they were already treated) had similar results and included the use of azithromycin.
When evaluating a study, it is also important to note whether conflicts of interest exist, as well as the quality of the peer review and the data itself. In the case of the French study, for example, the paper was published in a journal in which one of the authors was editor-in-chief, and it was accepted for publication after 24 hours. Patients who fared poorly on hydroxychloroquine were also left out of the study altogether, skewing the results.
What Randomized Controlled Trials Have Shown
Looking at the two major hydroxychloroquine trials, it is apparent that, when studied using the best tools of clinical trials, no benefit is likely to occur. The most important of these studies to announce results was part of the Recovery trial, which was designed to test multiple interventions in the treatment of COVID-19. This trial, which has yet to be formally published, was a randomized controlled trial that involved over 1500 hospitalized patients being administered hydroxychloroquine compared to over 3000 who did not receive the medication. Clinical testing requires large numbers of patients to have the power to demonstrate statistical significance -- the threshold at which any apparent benefit is more than you would expect by random chance alone.
In this study, hydroxychloroquine provided no mortality benefit or even a benefit in hospital length of stay. In fact, the opposite occurred. Hydroxychloroquine patients were more likely to stay in the hospital longer and were more likely to require mechanical ventilation. Additionally, smaller randomized trials conducted in China have not shown benefit either.
Another major study involved the use of hydroxychloroquine to prevent illness in people who were exposed to COVID-19. These results, published in The New England Journal of Medicine, included over 800 patients who were studied in a randomized double-blind controlled trial and also failed to show any benefit.
But what about adding the antibiotic azithromycin in conjunction with hydroxychloroquine? A three-arm randomized controlled study involving over 500 patients hospitalized with mild to moderate COVID-19 was conducted. Its results, also published in The New England Journal of Medicine, failed to show any benefit – with or without azithromycin – and demonstrated evidence of harm. Those who received these treatments had elevations of their liver function tests and heart rhythm abnormalities. These findings hold despite the retraction of an observational study showing similar results.
Additionally, when used in combination with remdesivir – an experimental antiviral – hydroxychloroquine has been shown to be associated with worse outcomes and more side effects.
But what about in mildly ill patients not requiring hospitalization? There was no benefit found in a randomized double-blind placebo-controlled trial of 400 patients, the majority of whom were given the drug within one day of symptoms.
Some randomized controlled studies have yet to report their findings on hydroxychloroquine in non-hospitalized patients, with the use of zinc (which has some evidence in the treatment of the common cold, another ailment that can be caused by coronaviruses). And studies have yet to come out regarding whether hydroxychloroquine can prevent people from getting sick before they are even exposed. But the preponderance of the evidence from studies designed specifically to find benefit for treating COVID-19 does not support its use outside of a research setting.
Today – even with some studies (including those with zinc) still ongoing – if a patient asked me to prescribe them hydroxychloroquine for any severity or stage of illness, with or without zinc, with or without azithromycin, I would refrain. I would explain that, based on the evidence from clinical trials that has been amassed, there is no reason to believe that it will alter the course of illness for the better.
Failing to recognize the reality of the situation runs the risk of crowding out other more promising treatments and creating animosity where none should exist.
What has been occurring is a continual shifting of goalposts with each negative hydroxychloroquine study. Those in favor of the drug protest that a trial did not include azithromycin or zinc or wasn't given at the right time to the right patients. While there may be biological plausibility to treating illness early or combining treatments with zinc, it can only be definitively shown in a randomized, controlled prospective study.
The bottom line: A study that only looks at past outcomes in one group of patients – even when well conducted – is at most hypothesis generating and cannot be used as the sole basis for a new treatment paradigm.
Some may argue that there is no time to wait for definitive studies, but no treatment is benign. The risk/benefit ratio is not the same for every possible use of the drug. For example, hydroxychloroquine has a long record of use in rheumatoid arthritis and systemic lupus (whose patients are facing shortages because of COVID-19 related demand). But the risk of side effects for many of these patients is worth taking because of the substantial benefit the drug provides in treating those conditions.
In COVID-19, however, the disease apparently causes cardiac abnormalities in a great deal of many mild cases, a situation that should prompt caution when using any drugs that have known effects on the cardiac system -- drugs like hydroxychloroquine and azithromycin.
My Own Experience
It is not the case that every physician was biased against this drug from the start. Indeed, most of us wanted it to be shown to be beneficial, as it was a generic drug that was widely available and very familiar. In fact, early in the pandemic I prescribed it to hospitalized patients on two occasions per a hospital protocol. However, it is impossible for me as a sole clinician to know whether it worked, was neutral, or was harmful. In recent days, however, I have found the hydroxychloroquine talk to have polluted the atmosphere. One recent patient was initially refusing remdesivir, a drug proven in large randomized trials to have effectiveness, because he had confused it with hydroxychloroquine.
Moving On to Other COVID Treatments: What a Treatment Should Do
The story of hydroxychloroquine illustrates a fruitless search for what we are actually looking for in a COVID-19 treatment. In short, we are looking for a medication that can decrease symptoms, decrease complications, hasten recovery, decrease hospitalizations, decrease contagiousness, decrease deaths, and prevent infection. While it is unlikely to find a single antiviral that can accomplish all of these, fulfilling even just one is important.
For example, remdesivir hastens recovery and dexamethasone decreases mortality. Definitive results of the use of convalescent plasma and immunomodulating drugs such as siltuxamab, baricitinib, and anakinra (for use in the cytokine storms characteristic of severe disease) are still pending, as are the trials with monoclonal antibodies.
While it was crucial that the medical and scientific community definitively answer the questions surrounding the use of chloroquine and hydroxychloroquine in the treatment of COVID-19, it is time to face the facts and accept that its use for the treatment of this disease is not likely to be beneficial. Failing to recognize the reality of the situation runs the risk of crowding out other more promising treatments and creating animosity where none should exist.
Dr. Adalja is focused on emerging infectious disease, pandemic preparedness, and biosecurity. He has served on US government panels tasked with developing guidelines for the treatment of plague, botulism, and anthrax in mass casualty settings and the system of care for infectious disease emergencies, and as an external advisor to the New York City Health and Hospital Emergency Management Highly Infectious Disease training program, as well as on a FEMA working group on nuclear disaster recovery. Dr. Adalja is an Associate Editor of the journal Health Security. He was a coeditor of the volume Global Catastrophic Biological Risks, a contributing author for the Handbook of Bioterrorism and Disaster Medicine, the Emergency Medicine CorePendium, Clinical Microbiology Made Ridiculously Simple, UpToDate's section on biological terrorism, and a NATO volume on bioterrorism. He has also published in such journals as the New England Journal of Medicine, the Journal of Infectious Diseases, Clinical Infectious Diseases, Emerging Infectious Diseases, and the Annals of Emergency Medicine. He is a board-certified physician in internal medicine, emergency medicine, infectious diseases, and critical care medicine. Follow him on Twitter: @AmeshAA