How 30 Years of Heart Surgeries Taught My Dad How to Live
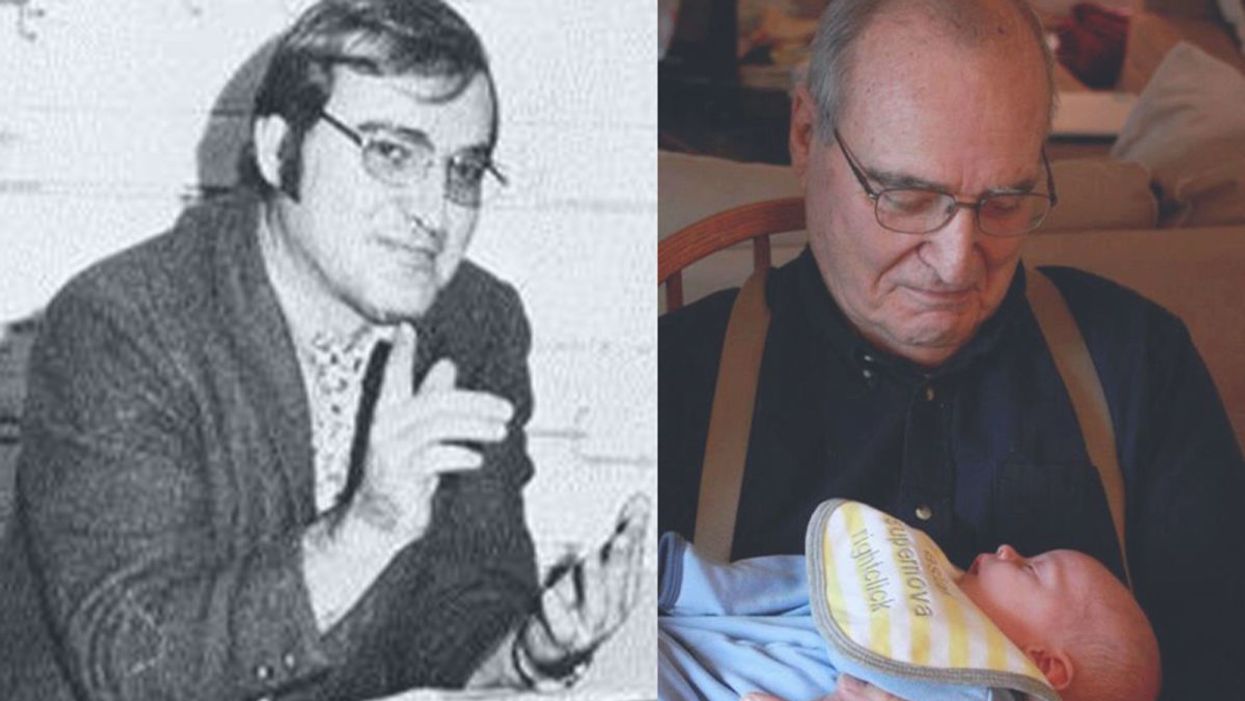
A mid-1970s photo of the author's father, and him holding a grandchild in 2012.
[Editor's Note: This piece is the winner of our 2019 essay contest, which prompted readers to reflect on the question: "How has an advance in science or medicine changed your life?"]
My father did not expect to live past the age of 50. Neither of his parents had done so. And he also knew how he would die: by heart attack, just as his father did.
In July of 1976, he had his first heart attack, days before his 40th birthday.
My dad lived the first 40 years of his life with this knowledge buried in his bones. He started smoking at the age of 12, and was drinking before he was old enough to enlist in the Navy. He had a sarcastic, often cruel, sense of humor that could drive my mother, my sister and me into tears. He was not an easy man to live with, but that was okay by him - he didn't expect to live long.
In July of 1976, he had his first heart attack, days before his 40th birthday. I was 13, and my sister was 11. He needed quadruple bypass surgery. Our small town hospital was not equipped to do this type of surgery; he would have to be transported 40 miles away to a heart center. I understood this journey to mean that my father was seriously ill, and might die in the hospital, away from anyone he knew. And my father knew a lot of people - he was a popular high school English teacher, in a town with only three high schools. He knew generations of students and their parents. Our high school football team did a blood drive in his honor.

During a trip to Disney World in 1974, Dad was suffering from angina the entire time but refused to tell me (left) and my sister, Kris.
Quadruple bypass surgery in 1976 meant that my father's breastbone was cut open by a sternal saw. His ribcage was spread wide. After the bypass surgery, his bones would be pulled back together, and tied in place with wire. The wire would later be pulled out of his body when the bones knitted back together. It would take months before he was fully healed.
Dad was in the hospital for the rest of the summer and into the start of the new school year. Going to visit him was farther than I could ride my bicycle; it meant planning a trip in the car and going onto the interstate. The first time I was allowed to visit him in the ICU, he was lying in bed, and then pushed himself to sit up. The heart monitor he was attached to spiked up and down, and I fainted. I didn't know that heartbeats change when you move; television medical dramas never showed that - I honestly thought that I had driven my father into another heart attack.
Only a few short years after that, my father returned to the big hospital to have his heart checked with a new advance in heart treatment: a CT scan. This would allow doctors to check for clogged arteries and treat them before a fatal heart attack. The procedure identified a dangerous blockage, and my father was admitted immediately. This time, however, there was no need to break bones to get to the problem; my father was home within a month.
During the late 1970's, my father changed none of his habits. He was still smoking, and he continued to drink. But now, he was also taking pills - pills to manage the pain. He would pop a nitroglycerin tablet under his tongue whenever he was experiencing angina (I have a vivid memory of him doing this during my driving lessons), but he never mentioned that he was in pain. Instead, he would snap at one of us, or joke that we were killing him.
I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count.
Being the kind of guy he was, my father never wanted to talk about his health. Any admission of pain implied that he couldn't handle pain. He would try to "muscle through" his angina, as if his willpower would be stronger than his heart muscle. His efforts would inevitably fail, leaving him angry and ready to lash out at anyone or anything. He would blame one of us as a reason he "had" to take valium or pop a nitro tablet. Dinners often ended in shouts and tears, and my father stalking to the television room with a bottle of red wine.
In the 1980's while I was in college, my father had another heart attack. But now, less than 10 years after his first, medicine had changed: our hometown hospital had the technology to run dye through my father's blood stream, identify the blockages, and do preventative care that involved statins and blood thinners. In one case, the doctors would take blood vessels from my father's legs, and suture them to replace damaged arteries around his heart. New advances in cholesterol medication and treatments for angina could extend my father's life by many years.
My father decided it was time to quit smoking. It was the first significant health step I had ever seen him take. Until then, he treated his heart issues as if they were inevitable, and there was nothing that he could do to change what was happening to him. Quitting smoking was the first sign that my father was beginning to move out of his fatalistic mindset - and the accompanying fatal behaviors that all pointed to an early death.
In 1986, my father turned 50. He had now lived longer than either of his parents. The habits he had learned from them could be changed. He had stopped smoking - what else could he do?
It was a painful decade for all of us. My parents divorced. My sister quit college. I moved to the other side of the country and stopped speaking to my father for almost 10 years. My father remarried, and divorced a second time. I stopped counting the number of times he was in and out of the hospital with heart-related issues.
In the early 1990's, my father reached out to me. I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count. He traveled across the country to spend a week with me, to meet my friends, and to rebuild his relationship with me. He did the same with my sister. He stopped drinking. He was more forthcoming about his health, and admitted that he was taking an antidepressant. His humor became less cruel and sadistic. He took an active interest in the world. He became part of my life again.
The 1990's was also the decade of angioplasty. My father explained it to me like this: during his next surgery, the doctors would place balloons in his arteries, and inflate them. The balloons would then be removed (or dissolve), leaving the artery open again for blood. He had several of these surgeries over the next decade.
When my father was in his 60's, he danced at with me at my wedding. It was now 10 years past the time he had expected to live, and his life was transformed. He was living with a woman I had known since I was a child, and my wife and I would make regular visits to their home. My father retired from teaching, became an avid gardener, and always had a home project underway. He was a happy man.

Dancing with my father at my wedding in 1998.
Then, in the mid 2000's, my father faced another serious surgery. Years of arterial surgery, angioplasty, and damaged heart muscle were taking their toll. He opted to undergo a life-saving surgery at Cleveland Clinic. By this time, I was living in New York and my sister was living in Arizona. We both traveled to the Midwest to be with him. Dad was unconscious most of the time. We took turns holding his hand in the ICU, encouraging him to regain his will to live, and making outrageous threats if he didn't listen to us.
The nursing staff were wonderful. I remember telling them that my father had never expected to live this long. One of the nurses pointed out that most of the patients in their ward were in their 70's and 80's, and a few were in their 90's. She reminded me that just a decade earlier, most hospitals were unwilling to do the kind of surgery my father had received on patients his age. In the first decade of the 21st century, however, things were different: 90-year-olds could now undergo heart surgery and live another decade. My father was on the "young" side of their patients.
The Cleveland Clinic visit would be the last major heart surgery my father would have. Not that he didn't return to his local hospital a few times after that: he broke his neck -- not once, but twice! -- slipping on ice. And in the 2010's, he began to show signs of dementia, and needed more home care. His partner, who had her own health issues, was not able to provide the level of care my father needed. My sister invited him to move in with her, and in 2015, I traveled with him to Arizona to get him settled in.
After a few months, he accepted home hospice. We turned off his pacemaker when the hospice nurse explained to us that the job of a pacemaker is to literally jolt a patient's heart back into beating. The jolts were happening more and more frequently, causing my Dad additional, unwanted pain.

My father in 2015, a few months before his death.
My father died in February 2016. His body carried the scars and implants of 30 years of cardiac surgeries, from the ugly breastbone scar from the 1970's to scars on his arms and legs from borrowed blood vessels, to the tiny red circles of robotic incisions from the 21st century. The arteries and veins feeding his heart were a patchwork of transplanted leg veins and fragile arterial walls pressed thinner by balloons.
And my father died with no regrets or unfinished business. He died in my sister's home, with his long-time partner by his side. Medical advancements had given him the opportunity to live 30 years longer than he expected. But he was the one who decided how to live those extra years. He was the one who made the years matter.
Coronavirus Misinformation: How You Can Fight Back
Turn yourself into a source of coronavirus facts and a bulwark against the fake, misleading and fraudulent.
When it comes to fighting the new coronavirus threat, the truth is one of the few things more crucial than a gallon of hand sanitizer. But these days, both can be hard to find if you don't know where to look.
"Humans are wired to respond to emotional triggers and share misinformation if it reinforces existing beliefs and prejudices."
While it's only been around for a few months, COVID-19 has already produced an ever-expanding universe of conspiracy theories about its origins, its spread, and the danger it poses. Meanwhile, fraudulent cures and myths about treatments threaten to upend public health efforts to contain the epidemic.
But ordinary citizens aren't helpless. Research offers insight into why we're susceptible to misinformation, and armies of fact-checkers can tell us what's real and what isn't. Meanwhile, experts are offering tips about how we can effectively promote facts whether we're chatting with a stranger at the post office or challenging a cousin on Facebook.
Here a four-part strategy to help you fight back against the Coronavirus Misinformation Industrial Complex:
Understand How Bogus Beliefs Work
That crank on the Internet may be your neighbor. Or maybe even you.
According to a 2014 study published in JAMA Internal Medicine, nearly half of American surveyed said they believed in at least one grand medical conspiracy theory. Twenty percent agreed, for example, that cell phones cause cancer but officials won't do anything because of corporate pressure, and 37 percent believed an elaborate conspiracy theory about the suppression of natural cancer cures. "Although it is common to disparage adherents of conspiracy theories as a delusional fringe of paranoid cranks, our data suggest that medical conspiracy theories are widely known, broadly endorsed, and highly predictive of many common health behaviors," the study authors write.
In an interview with leapsmag, study lead author Eric Oliver said we're drawn to "conspiracy theories that correspond with our intuitions."
"In the case of medicine, I think there are three big factors: Fears of Big Pharma -- a large percentage of Americans have a distorted sense of what pharmaceutical companies are capable of -- fears of government, and fears of contagion," said Oliver, a political scientist at the University of Chicago.
Why does it matter if people believe in conspiracy theories about coronavirus? As Oliver's study notes, conspiracy theorists are less likely to rely on traditional medicine, get flu shots, or go to annual check-ups. They could be especially susceptible to disease and inappropriate treatment.
Joseph Uscinski, a professor of political science at the University of Miami who studies conspiracies, elaborated on how this works. "You could have people who think coronavirus is fake and say, 'I'm not going to wash my hand or take preventive action. This is the media making something up, or this is just a plot for the pharmaceutical companies to sell a vaccine.' If you have a lot of people acting that way, that increases the ability of the virus to spread."
Get the Facts from the Experts
How can you avoid being a misinformation source? Educate yourself to make sure you're not spouting fake facts yourself with the instant ease that the Internet allows. "Humans are wired to respond to emotional triggers and share misinformation if it reinforces existing beliefs and prejudices," writes misinformation scholar Claire Wardle in a 2019 Scientific American commentary. That means you too.
For coronavirus facts, experts recommend looking to the websites of government agencies (such as the CDC, World Health Organization and National Institutes of Health) and top-tier medical organizations (Mayo Clinic, Infectious Disease Society of America).
Respected mainstream news outlets such as The New York Times and National Public Radio offer extensive original reporting on the coronavirus threat. While some news outlets still require users to pay to get full access to stories, others have dropped their paywalls and made coronavirus content free to all. These include the Seattle Times, Bloomberg News and the medical news site Stat.
Locally, look to your region's public health department, news outlets, and medical organizations such as hospitals and health plans.
The Poynter Institute, a journalism watchdog outfit, offers a helpful guide to evaluating what you read about coronavirus. And a paid service called NewsGuard offers a browser plug-in that provides a "trust rating" for popular news sites. "Our goal is to teach news literacy–and we hope all websites will earn green ratings and be generally reliable to consumers," the NewsGuard site says.
"As we combat misinformation, we also need to be mindful of the fact that we're dealing with a lot of uncertainty."
Remember, however, that scientists and physicians are learning more about the coronavirus each day. Assumptions about the virus will change as more information comes in, and there are still many questions about crucial topics like its fatality rate and the ways the virus spreads. You should expect that reliable sources – and experts – may provide conflicting information.
"As we combat misinformation, we also need to be mindful of the fact that we're dealing with a lot of uncertainty," says Boston cardiologist and author Dr. Haider Warraich of Brigham and Women's Hospital.
Double-Check Suspicious Information
No, the coronavirus wasn't created in a Winnipeg laboratory. You can't kill it by drinking bleach or frolicking in snow. And, as the French Health Ministry helpfully advised on Twitter, "Non, La cocaïne NE protège PAS contre le #COVID19" – "No, cocaine does NOT prevent Covid-19."
Facebook, YouTube and Twitter are all trying to remove fake or misleading coronavirus content, The New York Times reported, and "all said they were making efforts to point people back to reliable sources of medical information." Still, as the Times reports, bogus cures and conspiracy theories are rampant across social media and beyond.
Fortunately, there are many fact-checking resources. Turn to them for ammunition before you amplify – or challenge -- a coronavirus claim that seems suspicious.
Helpful myth-busting resources include:
** The venerable fact-checking site Snopes.com, which has checked multiple coronavirus claims. (Example: No, garlic water won't cure coronavirus.)
** The World Health Organization. (Example: No, mosquito bites can't transmit coronavirus)
** FactCheck.org. (Example: No, a disgraced Harvard scientist wasn't arrested for creating the coronavirus.)
** PolitiFact.org. (Example: No, the coronavirus is not just "the common cold.")
** The International Fact-Checking Network, accessible via the social-media hashtags #CoronaVirusFacts and #DatosCoronaVirus.
Correct Others With Caution
On social media, anger and sarcasm make up a kind of common tongue. But sick burns won't force misinformed people see the light. Instead, try a gentler approach.
"The most important thing would be to first acknowledge their anxieties rather than first trying to rationalize away their misbeliefs," said the University of Chicago's Oliver. "People embrace misinformation and conspiracy theories because they are afraid and trying to make sense of the world. Their beliefs serve a strong emotional function and will be defended as such. Trying to rationalize with them or argue with them may be counterproductive if one can't first put them at some ease."
Turn yourself into a source of coronavirus facts and a bulwark against the fake, misleading, and fraudulent.
So what can you do? "There will never be a magic bullet," the University of Miami's Uscinski said, but one approach is to highlight reliable information from sources that the person trusts, such as news outlets (think MSNBC or Fox News) or politicians.
However, don't waste your time. "If you have people who are believing in the craziest thing, they're probably not going to offer a rational conversation," he said. And, he added, there's an alternative to correcting others: Turn yourself into a source of coronavirus facts and a bulwark against the fake, misleading, and fraudulent. "We can be preventive and inoculate people against these beliefs," he said, "by flooding the information environment with proper information as much as possible."
Frequent, thorough handwashing is essential to protecting yourself from infection.
What's the case-fatality rate?
Currently, the official rate is 3.4%. But this is likely way too high. China was hit particularly hard, and their healthcare system was overwhelmed. The best data we have is from South Korea. The Koreans tested 210,000 people and detected the virus in 7,478 patients. So far, the death toll is 53, which is a case-fatality rate of 0.7%. This is seven times worse than the seasonal flu (which has a case-fatality rate of 0.1%).
What's the best way to clean your hands? Soap and water? Hand sanitizer?
Soap and water is always best. Be sure to wash your hands thoroughly. (The CDC recommends 20 seconds.) If soap and water are not available, the CDC says to use hand sanitizer that is at least 60% alcohol. The problem with hand sanitizer, however, is that people neither use enough nor spread it over their hands properly. Also, the sanitizer should be covering your hands for 10-15 seconds, not evaporating before that.
How often should I wash my hands?
You should wash your hands after being in a public place, before you eat, and before you touch your face. It's a good idea to wash your hands after handling money and your cell phone, too.
How long can coronavirus live on surfaces?
It depends on the surface. According to the New York Times, "[C]old and flu viruses survive longer on inanimate surfaces that are nonporous, like metal, plastic and wood, and less on porous surfaces, like clothing, paper and tissue." According to the Journal of Hospital Infection, human coronaviruses "can persist on inanimate surfaces like metal, glass or plastic for up to 9 days, but can be efficiently inactivated by surface disinfection procedures with 62–71% ethanol, 0.5% hydrogen peroxide or 0.1% sodium hypochlorite within 1 minute." (Note: Sodium hypochlorite is bleach.)
Can Lysol wipes kill it?
Maybe not. It depends on the active ingredient. Many Lysol products use benzalkonium chloride, which the aforementioned Journal of Hospital Infection paper said was "less effective." The EPA has released a list of disinfectants recommended for use against coronavirus.
Should you wear a mask in public?
The CDC does not recommend that healthy people wear a mask in public. The benefit is likely small. However, if you are sick, then you should wear a mask to help catch respiratory droplets as you exhale.
Will pets give it to you?
That can't be ruled out. There is a documented case of human-to-canine transmission. However, an article in LiveScience explains that canine-to-human is unlikely.
Are there any "normal" things we are doing that make things worse?
Yes! Not washing your hands!!
What does it mean that previously cleared people are getting sick again? Is it the virus within or have they caught it via contamination?
It's not entirely clear. It could be that the virus was never cleared to begin with. Or it could be that the person was simply infected again. That could happen if the antibodies generated don't last long.
Will the virus go away with the weather/summer?
Quite likely, yes. Cold and flu viruses don't do well outside in summer weather. (For influenza, the warm weather causes the viral envelope to become a liquid, and it can no longer protect the virus.) That's why cold and flu season is always during the late fall and winter. However, some experts think that it is a "false hope" that the coronavirus will disappear during the summer. We'll have to wait and see.
And will it come back in the fall/winter?
That's a likely outcome. Again, we'll have to wait and see. Some epidemiologists think that COVID-19 will become seasonal like influenza.
Does dry or humid air make a difference?
Flu viruses prefer cold, dry weather. That could be true of coronaviruses, too.
What is the incubation period?
According to the World Health Organization, it's about 5 days. But it could be anywhere from 1 to 14 days.
Should you worry about sitting next to asymptomatic people on a plane or train?
It's not possible to tell if an asymptomatic person is infected or not. That's what makes asymptomatic people tricky. Just be cautious. If you're worried, treat everyone like they might be infected. Don't let them get too close or cough in your face. Be sure to wash your hands.
Should you cancel air travel planned in the next 1-2 months in the U.S.?
There are no hard and fast rules. Use common sense. Avoid hotspots of infection. If you have a trip planned to Wuhan, you might want to wait on that one. If you have a trip planned to Seattle and you're over the age of 60 and/or have an underlying health condition, you may want to hold off on that, too. If you do fly on a plane, former FDA commissioner Dr. Scott Gottlieb recommends cleaning the back of your seat and other close contact areas with antiseptic wipes. He also refuses to take anything handed out by flight attendants, since he says the biggest route of transmission comes from touching contaminated surfaces (and then touching your face).
There have been reports of an escalation of hate crimes towards Asian Americans. Can the microbiologist help illuminate that this disease has impacted all racial groups?
People might be racist, but COVID-19 is not. It can infect anyone. Older people (i.e., 60 years and older) and those with underlying health conditions are most at risk. Interestingly, young people (aged 9 and under) are minimally impacted.
To what extent/if any should toddlers -- who put everything in mouth -- avoid group classes like Gymboree?
If they get infected, toddlers will probably experience only a mild illness. The problem is if the toddler then infects somebody at higher risk, like grandpa or grandma.
Should I avoid events like concerts or theater performances if I live in a place where there is known coronavirus?
It's not an unreasonable thing to do.
Any special advice or concerns for pregnant women?
There isn't good data on this. Previous evidence, reported by the CDC, suggests that pregnant women may be more susceptible to respiratory viruses.
Advice for residents of long-term care facilities/nursing homes?
Remind the nurse or aide to constantly wash their hands.
Can we eat at Chinese restaurants? Does eating onions kill viruses? Can I take an Uber and be safe from infection?
Yes. No. Does the Uber driver or previous passengers have coronavirus? It's not possible to tell. So, treat an Uber like a public space and behave accordingly.
What public spaces should we avoid?
That's hard to say. Some people avoid large gatherings, others avoid leaving the house. Ultimately, it's going to depend on who you are and what sort of risk you're willing to take. (For example, are you young and healthy or old and sick?) I would be willing to do things that I would advise older people avoid, like going to a sporting event.
What are the differences between the L strain and the S strain?
That's not entirely clear, and it's not even clear that they are separate strains. There are some genetic differences between them. However, just because RNA viruses mutate doesn't necessarily mean that the virus will mutate to something more dangerous or unrecognizable by our immune system. The measles virus mutates, but it more or less remains the same, which is why a single vaccine could eradicate it – if enough people actually were willing to get a measles shot.
Should I wear disposable gloves while traveling?
No. If you touch something that's contaminated, the virus will be on your glove instead of your hand. If you then touch your face, you still might get sick.

