How 30 Years of Heart Surgeries Taught My Dad How to Live
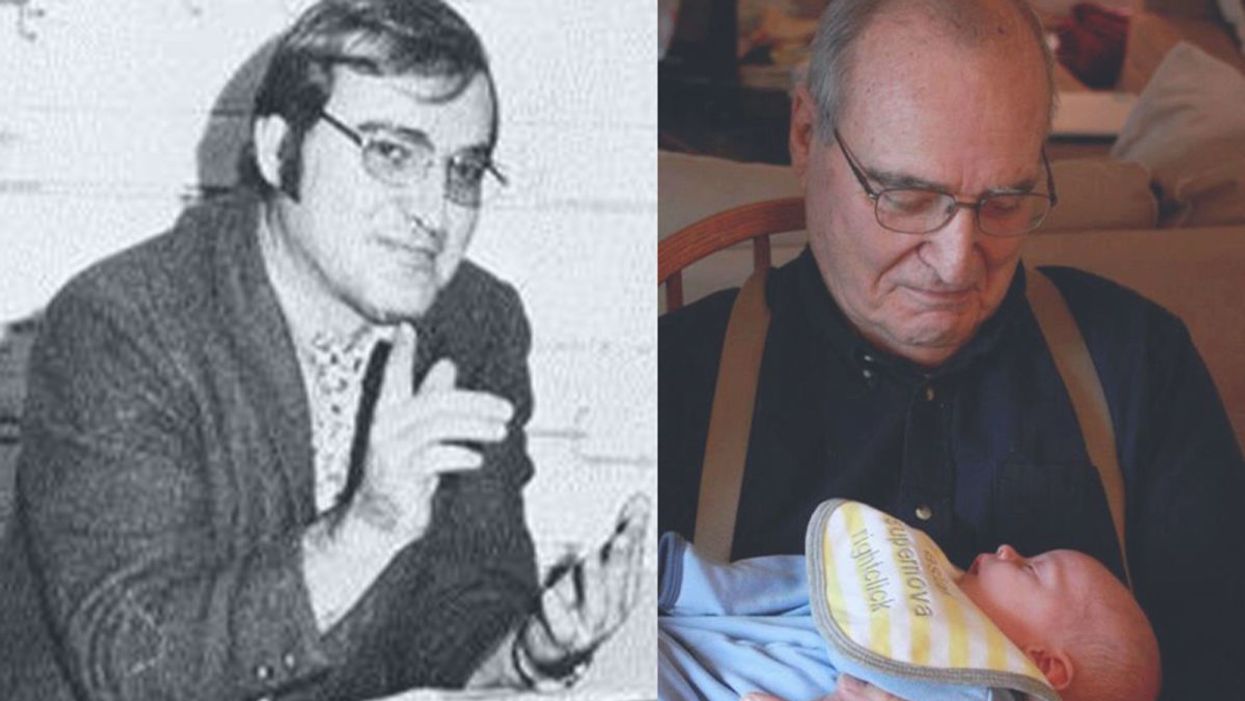
A mid-1970s photo of the author's father, and him holding a grandchild in 2012.
[Editor's Note: This piece is the winner of our 2019 essay contest, which prompted readers to reflect on the question: "How has an advance in science or medicine changed your life?"]
My father did not expect to live past the age of 50. Neither of his parents had done so. And he also knew how he would die: by heart attack, just as his father did.
In July of 1976, he had his first heart attack, days before his 40th birthday.
My dad lived the first 40 years of his life with this knowledge buried in his bones. He started smoking at the age of 12, and was drinking before he was old enough to enlist in the Navy. He had a sarcastic, often cruel, sense of humor that could drive my mother, my sister and me into tears. He was not an easy man to live with, but that was okay by him - he didn't expect to live long.
In July of 1976, he had his first heart attack, days before his 40th birthday. I was 13, and my sister was 11. He needed quadruple bypass surgery. Our small town hospital was not equipped to do this type of surgery; he would have to be transported 40 miles away to a heart center. I understood this journey to mean that my father was seriously ill, and might die in the hospital, away from anyone he knew. And my father knew a lot of people - he was a popular high school English teacher, in a town with only three high schools. He knew generations of students and their parents. Our high school football team did a blood drive in his honor.

During a trip to Disney World in 1974, Dad was suffering from angina the entire time but refused to tell me (left) and my sister, Kris.
Quadruple bypass surgery in 1976 meant that my father's breastbone was cut open by a sternal saw. His ribcage was spread wide. After the bypass surgery, his bones would be pulled back together, and tied in place with wire. The wire would later be pulled out of his body when the bones knitted back together. It would take months before he was fully healed.
Dad was in the hospital for the rest of the summer and into the start of the new school year. Going to visit him was farther than I could ride my bicycle; it meant planning a trip in the car and going onto the interstate. The first time I was allowed to visit him in the ICU, he was lying in bed, and then pushed himself to sit up. The heart monitor he was attached to spiked up and down, and I fainted. I didn't know that heartbeats change when you move; television medical dramas never showed that - I honestly thought that I had driven my father into another heart attack.
Only a few short years after that, my father returned to the big hospital to have his heart checked with a new advance in heart treatment: a CT scan. This would allow doctors to check for clogged arteries and treat them before a fatal heart attack. The procedure identified a dangerous blockage, and my father was admitted immediately. This time, however, there was no need to break bones to get to the problem; my father was home within a month.
During the late 1970's, my father changed none of his habits. He was still smoking, and he continued to drink. But now, he was also taking pills - pills to manage the pain. He would pop a nitroglycerin tablet under his tongue whenever he was experiencing angina (I have a vivid memory of him doing this during my driving lessons), but he never mentioned that he was in pain. Instead, he would snap at one of us, or joke that we were killing him.
I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count.
Being the kind of guy he was, my father never wanted to talk about his health. Any admission of pain implied that he couldn't handle pain. He would try to "muscle through" his angina, as if his willpower would be stronger than his heart muscle. His efforts would inevitably fail, leaving him angry and ready to lash out at anyone or anything. He would blame one of us as a reason he "had" to take valium or pop a nitro tablet. Dinners often ended in shouts and tears, and my father stalking to the television room with a bottle of red wine.
In the 1980's while I was in college, my father had another heart attack. But now, less than 10 years after his first, medicine had changed: our hometown hospital had the technology to run dye through my father's blood stream, identify the blockages, and do preventative care that involved statins and blood thinners. In one case, the doctors would take blood vessels from my father's legs, and suture them to replace damaged arteries around his heart. New advances in cholesterol medication and treatments for angina could extend my father's life by many years.
My father decided it was time to quit smoking. It was the first significant health step I had ever seen him take. Until then, he treated his heart issues as if they were inevitable, and there was nothing that he could do to change what was happening to him. Quitting smoking was the first sign that my father was beginning to move out of his fatalistic mindset - and the accompanying fatal behaviors that all pointed to an early death.
In 1986, my father turned 50. He had now lived longer than either of his parents. The habits he had learned from them could be changed. He had stopped smoking - what else could he do?
It was a painful decade for all of us. My parents divorced. My sister quit college. I moved to the other side of the country and stopped speaking to my father for almost 10 years. My father remarried, and divorced a second time. I stopped counting the number of times he was in and out of the hospital with heart-related issues.
In the early 1990's, my father reached out to me. I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count. He traveled across the country to spend a week with me, to meet my friends, and to rebuild his relationship with me. He did the same with my sister. He stopped drinking. He was more forthcoming about his health, and admitted that he was taking an antidepressant. His humor became less cruel and sadistic. He took an active interest in the world. He became part of my life again.
The 1990's was also the decade of angioplasty. My father explained it to me like this: during his next surgery, the doctors would place balloons in his arteries, and inflate them. The balloons would then be removed (or dissolve), leaving the artery open again for blood. He had several of these surgeries over the next decade.
When my father was in his 60's, he danced at with me at my wedding. It was now 10 years past the time he had expected to live, and his life was transformed. He was living with a woman I had known since I was a child, and my wife and I would make regular visits to their home. My father retired from teaching, became an avid gardener, and always had a home project underway. He was a happy man.

Dancing with my father at my wedding in 1998.
Then, in the mid 2000's, my father faced another serious surgery. Years of arterial surgery, angioplasty, and damaged heart muscle were taking their toll. He opted to undergo a life-saving surgery at Cleveland Clinic. By this time, I was living in New York and my sister was living in Arizona. We both traveled to the Midwest to be with him. Dad was unconscious most of the time. We took turns holding his hand in the ICU, encouraging him to regain his will to live, and making outrageous threats if he didn't listen to us.
The nursing staff were wonderful. I remember telling them that my father had never expected to live this long. One of the nurses pointed out that most of the patients in their ward were in their 70's and 80's, and a few were in their 90's. She reminded me that just a decade earlier, most hospitals were unwilling to do the kind of surgery my father had received on patients his age. In the first decade of the 21st century, however, things were different: 90-year-olds could now undergo heart surgery and live another decade. My father was on the "young" side of their patients.
The Cleveland Clinic visit would be the last major heart surgery my father would have. Not that he didn't return to his local hospital a few times after that: he broke his neck -- not once, but twice! -- slipping on ice. And in the 2010's, he began to show signs of dementia, and needed more home care. His partner, who had her own health issues, was not able to provide the level of care my father needed. My sister invited him to move in with her, and in 2015, I traveled with him to Arizona to get him settled in.
After a few months, he accepted home hospice. We turned off his pacemaker when the hospice nurse explained to us that the job of a pacemaker is to literally jolt a patient's heart back into beating. The jolts were happening more and more frequently, causing my Dad additional, unwanted pain.

My father in 2015, a few months before his death.
My father died in February 2016. His body carried the scars and implants of 30 years of cardiac surgeries, from the ugly breastbone scar from the 1970's to scars on his arms and legs from borrowed blood vessels, to the tiny red circles of robotic incisions from the 21st century. The arteries and veins feeding his heart were a patchwork of transplanted leg veins and fragile arterial walls pressed thinner by balloons.
And my father died with no regrets or unfinished business. He died in my sister's home, with his long-time partner by his side. Medical advancements had given him the opportunity to live 30 years longer than he expected. But he was the one who decided how to live those extra years. He was the one who made the years matter.
Today’s Focus on STEM Education Is Missing A Crucial Point
A student in a contemplative pose.
I once saw a fascinating TED talk on 3D printing. As I watched the presenter discuss the custom fabrication, not of plastic gears or figurines, but of living, implantable kidneys, I thought I was finally living in the world of Star Trek, and I experienced a flush of that eager, expectant enthusiasm I felt as a child looking toward the future. I looked at my current career and felt a rejuvenation of my commitment to teach young people the power of science.
The well-rounded education of human beings needs to include lessons learned both from a study of the physical world, and from a study of humanity.
Whether we are teachers or not, those of us who admire technology and innovation, and who wish to support progress, usually embrace the importance of educating the next generation of scientists and inventors. Growing a healthy technological civilization takes a lot of work, skill, and wisdom, and its continued health depends on future generations of competent thinkers. Thus, we may find it encouraging that there is currently an abundance of interest in STEM– the common acronym for the study of science, technology, engineering, and math.
But education is as challenging an endeavor as science itself. Educating youth--if we want to do it right--requires as much thought, work, and expertise as discovering a cure or pioneering regenerative medicine. Before we give our money, time, or support to any particular school or policy, let's give some thought to the details of the educational process.
A Well-Balanced Diet
For one thing, STEM education cannot stand in isolation. The well-rounded education of human beings needs to include lessons learned both from a study of the physical world, and from a study of humanity. This is especially true for the basic education of children, but it is true even for college students. And even for those in science and engineering, there are important lessons to be learned from the study of history, literature, and art.
Scientists have their own emotions and values, and also need financial support. The fruits of their labor ultimately benefit other people. How are we all to function together in our division-of-labor society, without some knowledge of the way societies work? How are we to fully thrive and enjoy life, without some understanding of ourselves, our motives, our moral values, and our relationships to others? STEM education needs the humanities as a partner. That flourishing civilization we dream of requires both technical competence and informed life-choices.
Think for Yourself (Even in Science)
Perhaps even more important than what is taught, is the subject of how things are taught. We want our children to learn the skill of thinking independently, but even in the sciences, we often fail completely to demonstrate how. Instead of teaching science as a thinking process, we indoctrinate, using the grand discoveries of the great scientists as our sacred texts. But consider the words of Isaac Newton himself, regarding rote learning:
A Vulgar Mechanick can practice what he has been taught or seen done, but if he is in an error he knows not how to find it out and correct it, and if you put him out of his road he is at a stand. Whereas he that is able to reason nimbly and judiciously about figure, force, and motion, is never at rest till he gets over every rub.
What's the point of all this formal schooling in the first place? Is it, as many of the proponents of STEM education might argue, to train students for a "good" career?
If our goal is to help students "reason nimbly" about the world around them, as the great scientists themselves did, are we succeeding? When we "teach" middle school students about DNA or cellular respiration by presenting as our only supporting evidence cartoon pictures, are we showing students a process of discovery based on evidence and hard work? Or are we just training them to memorize and repeat what the authorities say?
A useful education needs to give students the skill of following a line of reasoning, of asking rational questions, and of chewing things through in their minds--even if we regard the material as beyond question. Besides feeding students a well-balanced diet of knowledge, healthy schooling needs to teach them to digest this information thoroughly.
Thinking Training
Now step back for a moment and think about the purpose of education. What's the point of all this formal schooling in the first place? Is it, as many of the proponents of STEM education might argue, to train students for a "good" career? That view may have some validity for young adults, who are beginning to choose electives in favored subjects, and have started to choose a direction for their career.
But for the basic education of children, this way of thinking is presumptuous and disastrous. I would argue that the central purpose of a basic education is not to teach children how to perform this or that particular skill, but simply to teach them to think clearly. We should not be aiming to provide job training, but thinking training. We should be helping children learn how to "reason nimbly" about the world around them, and breathing life into their thinking processes, by which they will grapple with the events and circumstances of their lives.
So as we admire innovation, dream of a wonderful future, and attempt to nurture the next generation of scientists and engineers, instead of obsessing over STEM education, let us focus on rational education. Let's worry about showing children how to think--about all the important things in life. Let's give them the basic facts of human existence -- physical and humanitarian -- and show them how to fluently and logically understand them.
Some students will become the next generation of creators, and some will follow other careers, but together -- if they are educated properly -- they will continue to grow their inheritance, and to keep our civilization healthy and flourishing, in body and in mind.
Do New Tools Need New Ethics?
Symbols of countries on a chessboard.
Scarcely a week goes by without the announcement of another breakthrough owing to advancing biotechnology. Recent examples include the use of gene editing tools to successfully alter human embryos or clone monkeys; new immunotherapy-based treatments offering longer lives or even potential cures for previously deadly cancers; and the creation of genetically altered mosquitos using "gene drives" to quickly introduce changes into the population in an ecosystem and alter the capacity to carry disease.
The environment for conducting science is dramatically different today than it was in the 1970s, 80s, or even the early 2000s.
Each of these examples puts pressure on current policy guidelines and approaches, some existing since the late 1970s, which were created to help guide the introduction of controversial new life sciences technologies. But do the policies that made sense decades ago continue to make sense today, or do the tools created during different eras in science demand new ethics guidelines and policies?
Advances in biotechnology aren't new of course, and in fact have been the hallmark of science since the creation of the modern U.S. National Institutes of Health in the 1940s and similar government agencies elsewhere. Funding agencies focused on health sciences research with the hope of creating breakthroughs in human health, and along the way, basic science discoveries led to the creation of new scientific tools that offered the ability to approach life, death, and disease in fundamentally new ways.
For example, take the discovery in the 1970s of the "chemical scissors" in living cells called restriction enzymes, which could be controlled and used to introduce cuts at predictable locations in a strand of DNA. This led to the creation of tools that for the first time allowed for genetic modification of any organism with DNA, which meant bacteria, plants, animals, and even humans could in theory have harmful mutations repaired, but also that changes could be made to alter or even add genetic traits, with potentially ominous implications.
The scientists involved in that early research convened a small conference to discuss not only the science, but how to responsibly control its potential uses and their implications. The meeting became known as the Asilomar Conference for the meeting center where it was held, and is often noted as the prime example of the scientific community policing itself. While the Asilomar recommendations were not sufficient from a policy standpoint, they offered a blueprint on which policies could be based and presented a model of the scientific community setting responsible controls for itself.
But the environment for conducting science changed over the succeeding decades and it is dramatically different today than it was in the 1970s, 80s, or even the early 2000s. The regime for oversight and regulation that has provided controls for the introduction of so-called "gene therapy" in humans starting in the mid-1970s is beginning to show signs of fraying. The vast majority of such research was performed in the U.S., U.K., and Europe, where policies were largely harmonized. But as the tools for manipulating humans at the molecular level advanced, they also became more reliable and more precise, as well as cheaper and easier to use—think CRISPR—and therefore more accessible to more people in many more countries, many without clear oversight or policies laying out responsible controls.
There is no precedent for global-scale science policy, though that is exactly what this moment seems to demand.
As if to make the point through news headlines, scientists in China announced in 2017 that they had attempted to perform gene editing on in vitro human embryos to repair an inherited mutation for beta thalassemia--research that would not be permitted in the U.S. and most European countries and at the time was also banned in the U.K. Similarly, specialists from a reproductive medicine clinic in the U.S. announced in 2016 that they had performed a highly controversial reproductive technology by which DNA from two women is combined (so-called "three parent babies"), in a satellite clinic they had opened in Mexico to avoid existing prohibitions on the technique passed by the U.S. Congress in 2015.
In both cases, genetic changes were introduced into human embryos that if successful would lead to the birth of a child with genetically modified germline cells—the sperm in boys or eggs in girls—with those genetic changes passed on to all future generations of related offspring. Those are just two very recent examples, and it doesn't require much imagination to predict the list of controversial possible applications of advancing biotechnologies: attempts at genetic augmentation or even cloning in humans, and alterations of the natural environment with genetically engineered mosquitoes or other insects in areas with endemic disease. In fact, as soon as this month, scientists in Africa may release genetically modified mosquitoes for the first time.
The technical barriers are falling at a dramatic pace, but policy hasn't kept up, both in terms of what controls make sense and how to address what is an increasingly global challenge. There is no precedent for global-scale science policy, though that is exactly what this moment seems to demand. Mechanisms for policy at global scale are limited–-think UN declarations, signatory countries, and sometimes international treaties, but all are slow, cumbersome and have limited track records of success.
But not all the news is bad. There are ongoing efforts at international discussion, such as an international summit on human genome editing convened in 2015 by the National Academies of Sciences and Medicine (U.S.), Royal Academy (U.K.), and Chinese Academy of Sciences (China), a follow-on international consensus committee whose report was issued in 2017, and an upcoming 2nd international summit in Hong Kong in November this year.
These efforts need to continue to focus less on common regulatory policies, which will be elusive if not impossible to create and implement, but on common ground for the principles that ought to guide country-level rules. Such principles might include those from the list proposed by the international consensus committee, including transparency, due care, responsible science adhering to professional norms, promoting wellbeing of those affected, and transnational cooperation. Work to create a set of shared norms is ongoing and worth continued effort as the relevant stakeholders attempt to navigate what can only be called a brave new world.

