How 30 Years of Heart Surgeries Taught My Dad How to Live
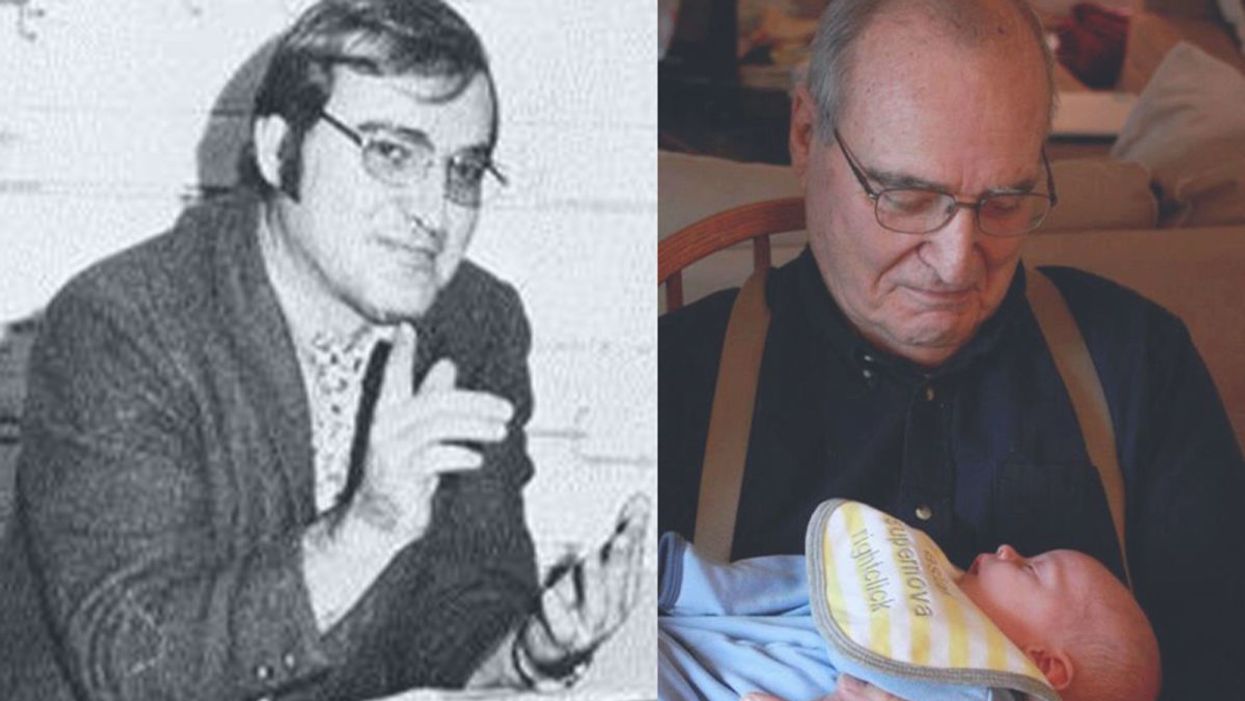
A mid-1970s photo of the author's father, and him holding a grandchild in 2012.
[Editor's Note: This piece is the winner of our 2019 essay contest, which prompted readers to reflect on the question: "How has an advance in science or medicine changed your life?"]
My father did not expect to live past the age of 50. Neither of his parents had done so. And he also knew how he would die: by heart attack, just as his father did.
In July of 1976, he had his first heart attack, days before his 40th birthday.
My dad lived the first 40 years of his life with this knowledge buried in his bones. He started smoking at the age of 12, and was drinking before he was old enough to enlist in the Navy. He had a sarcastic, often cruel, sense of humor that could drive my mother, my sister and me into tears. He was not an easy man to live with, but that was okay by him - he didn't expect to live long.
In July of 1976, he had his first heart attack, days before his 40th birthday. I was 13, and my sister was 11. He needed quadruple bypass surgery. Our small town hospital was not equipped to do this type of surgery; he would have to be transported 40 miles away to a heart center. I understood this journey to mean that my father was seriously ill, and might die in the hospital, away from anyone he knew. And my father knew a lot of people - he was a popular high school English teacher, in a town with only three high schools. He knew generations of students and their parents. Our high school football team did a blood drive in his honor.

During a trip to Disney World in 1974, Dad was suffering from angina the entire time but refused to tell me (left) and my sister, Kris.
Quadruple bypass surgery in 1976 meant that my father's breastbone was cut open by a sternal saw. His ribcage was spread wide. After the bypass surgery, his bones would be pulled back together, and tied in place with wire. The wire would later be pulled out of his body when the bones knitted back together. It would take months before he was fully healed.
Dad was in the hospital for the rest of the summer and into the start of the new school year. Going to visit him was farther than I could ride my bicycle; it meant planning a trip in the car and going onto the interstate. The first time I was allowed to visit him in the ICU, he was lying in bed, and then pushed himself to sit up. The heart monitor he was attached to spiked up and down, and I fainted. I didn't know that heartbeats change when you move; television medical dramas never showed that - I honestly thought that I had driven my father into another heart attack.
Only a few short years after that, my father returned to the big hospital to have his heart checked with a new advance in heart treatment: a CT scan. This would allow doctors to check for clogged arteries and treat them before a fatal heart attack. The procedure identified a dangerous blockage, and my father was admitted immediately. This time, however, there was no need to break bones to get to the problem; my father was home within a month.
During the late 1970's, my father changed none of his habits. He was still smoking, and he continued to drink. But now, he was also taking pills - pills to manage the pain. He would pop a nitroglycerin tablet under his tongue whenever he was experiencing angina (I have a vivid memory of him doing this during my driving lessons), but he never mentioned that he was in pain. Instead, he would snap at one of us, or joke that we were killing him.
I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count.
Being the kind of guy he was, my father never wanted to talk about his health. Any admission of pain implied that he couldn't handle pain. He would try to "muscle through" his angina, as if his willpower would be stronger than his heart muscle. His efforts would inevitably fail, leaving him angry and ready to lash out at anyone or anything. He would blame one of us as a reason he "had" to take valium or pop a nitro tablet. Dinners often ended in shouts and tears, and my father stalking to the television room with a bottle of red wine.
In the 1980's while I was in college, my father had another heart attack. But now, less than 10 years after his first, medicine had changed: our hometown hospital had the technology to run dye through my father's blood stream, identify the blockages, and do preventative care that involved statins and blood thinners. In one case, the doctors would take blood vessels from my father's legs, and suture them to replace damaged arteries around his heart. New advances in cholesterol medication and treatments for angina could extend my father's life by many years.
My father decided it was time to quit smoking. It was the first significant health step I had ever seen him take. Until then, he treated his heart issues as if they were inevitable, and there was nothing that he could do to change what was happening to him. Quitting smoking was the first sign that my father was beginning to move out of his fatalistic mindset - and the accompanying fatal behaviors that all pointed to an early death.
In 1986, my father turned 50. He had now lived longer than either of his parents. The habits he had learned from them could be changed. He had stopped smoking - what else could he do?
It was a painful decade for all of us. My parents divorced. My sister quit college. I moved to the other side of the country and stopped speaking to my father for almost 10 years. My father remarried, and divorced a second time. I stopped counting the number of times he was in and out of the hospital with heart-related issues.
In the early 1990's, my father reached out to me. I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count. He traveled across the country to spend a week with me, to meet my friends, and to rebuild his relationship with me. He did the same with my sister. He stopped drinking. He was more forthcoming about his health, and admitted that he was taking an antidepressant. His humor became less cruel and sadistic. He took an active interest in the world. He became part of my life again.
The 1990's was also the decade of angioplasty. My father explained it to me like this: during his next surgery, the doctors would place balloons in his arteries, and inflate them. The balloons would then be removed (or dissolve), leaving the artery open again for blood. He had several of these surgeries over the next decade.
When my father was in his 60's, he danced at with me at my wedding. It was now 10 years past the time he had expected to live, and his life was transformed. He was living with a woman I had known since I was a child, and my wife and I would make regular visits to their home. My father retired from teaching, became an avid gardener, and always had a home project underway. He was a happy man.

Dancing with my father at my wedding in 1998.
Then, in the mid 2000's, my father faced another serious surgery. Years of arterial surgery, angioplasty, and damaged heart muscle were taking their toll. He opted to undergo a life-saving surgery at Cleveland Clinic. By this time, I was living in New York and my sister was living in Arizona. We both traveled to the Midwest to be with him. Dad was unconscious most of the time. We took turns holding his hand in the ICU, encouraging him to regain his will to live, and making outrageous threats if he didn't listen to us.
The nursing staff were wonderful. I remember telling them that my father had never expected to live this long. One of the nurses pointed out that most of the patients in their ward were in their 70's and 80's, and a few were in their 90's. She reminded me that just a decade earlier, most hospitals were unwilling to do the kind of surgery my father had received on patients his age. In the first decade of the 21st century, however, things were different: 90-year-olds could now undergo heart surgery and live another decade. My father was on the "young" side of their patients.
The Cleveland Clinic visit would be the last major heart surgery my father would have. Not that he didn't return to his local hospital a few times after that: he broke his neck -- not once, but twice! -- slipping on ice. And in the 2010's, he began to show signs of dementia, and needed more home care. His partner, who had her own health issues, was not able to provide the level of care my father needed. My sister invited him to move in with her, and in 2015, I traveled with him to Arizona to get him settled in.
After a few months, he accepted home hospice. We turned off his pacemaker when the hospice nurse explained to us that the job of a pacemaker is to literally jolt a patient's heart back into beating. The jolts were happening more and more frequently, causing my Dad additional, unwanted pain.

My father in 2015, a few months before his death.
My father died in February 2016. His body carried the scars and implants of 30 years of cardiac surgeries, from the ugly breastbone scar from the 1970's to scars on his arms and legs from borrowed blood vessels, to the tiny red circles of robotic incisions from the 21st century. The arteries and veins feeding his heart were a patchwork of transplanted leg veins and fragile arterial walls pressed thinner by balloons.
And my father died with no regrets or unfinished business. He died in my sister's home, with his long-time partner by his side. Medical advancements had given him the opportunity to live 30 years longer than he expected. But he was the one who decided how to live those extra years. He was the one who made the years matter.
Catching colds may help protect kids from Covid
A new study shows that the immune system's response to colds can help prepare it to defend against COVID-19 - but only in the very young.
A common cold virus causes the immune system to produce T cells that also provide protection against SARS-CoV-2, according to new research. The study, published last month in PNAS, shows that this effect is most pronounced in young children. The finding may help explain why most young people who have been exposed to the cold-causing coronavirus have not developed serious cases of COVID-19.
One curiosity stood out in the early days of the COVID-19 pandemic – why were so few kids getting sick. Generally young children and the elderly are the most vulnerable to disease outbreaks, particularly viral infections, either because their immune systems are not fully developed or they are starting to fail.
But solid information on the new infection was so scarce that many public health officials acted on the precautionary principle, assumed a worst-case scenario, and applied the broadest, most restrictive policies to all people to try to contain the coronavirus SARS-CoV-2.
One early thought was that lockdowns worked and kids (ages 6 months to 17 years) simply were not being exposed to the virus. So it was a shock when data started to come in showing that well over half of them carried antibodies to the virus, indicating exposure without getting sick. That trend grew over time and the latest tracking data from the CDC shows that 96.3 percent of kids in the U.S. now carry those antibodies.
Antibodies are relatively quick and easy to measure, but some scientists are exploring whether the reactions of T cells could serve as a more useful measure of immune protection.
But that couldn't be the whole story because antibody protection fades, sometimes as early as a month after exposure and usually within a year. Additionally, SARS-CoV-2 has been spewing out waves of different variants that were more resistant to antibodies generated by their predecessors. The resistance was so significant that over time the FDA withdrew its emergency use authorization for a handful of monoclonal antibodies with earlier approval to treat the infection because they no longer worked.
Antibodies got most of the attention early on because they are part of the first line response of the immune system. Antibodies can bind to viruses and neutralize them, preventing infection. They are relatively quick and easy to measure and even manufacture, but as SARS-CoV-2 showed us, often viruses can quickly evolve to become more resistant to them. Some scientists are exploring whether the reactions of T cells could serve as a more useful measure of immune protection.
Kids, colds and T cells
T cells are part of the immune system that deals with cells once they have become infected. But working with T cells is much more difficult, takes longer, and is more expensive than working with antibodies. So studies often lags behind on this part of the immune system.
A group of researchers led by Annika Karlsson at the Karolinska Institute in Sweden focuses on T cells targeting virus-infected cells and, unsurprisingly, saw that they can play a role in SARS-CoV-2 infection. Other labs have shown that vaccination and natural exposure to the virus generates different patterns of T cell responses.
The Swedes also looked at another member of the coronavirus family, OC43, which circulates widely and is one of several causes of the common cold. The molecular structure of OC43 is similar to its more deadly cousin SARS-CoV-2. Sometimes a T cell response to one virus can produce a cross-reactive response to a similar protein structure in another virus, meaning that T cells will identify and respond to the two viruses in much the same way. Karlsson looked to see if T cells for OC43 from a wide age range of patients were cross-reactive to SARS-CoV-2.
And that is what they found, as reported in the PNAS study last month; there was cross-reactive activity, but it depended on a person’s age. A subset of a certain type of T cells, called mCD4+,, that recognized various protein parts of the cold-causing virus, OC43, expressed on the surface of an infected cell – also recognized those same protein parts from SARS-CoV-2. The T cell response was lower than that generated by natural exposure to SARS-CoV-2, but it was functional and thus could help limit the severity of COVID-19.
“One of the most politicized aspects of our pandemic response was not accepting that children are so much less at risk for severe disease with COVID-19,” because usually young children are among the most vulnerable to pathogens, says Monica Gandhi, professor of medicine at the University of California San Francisco.
“The cross-reactivity peaked at age six when more than half the people tested have a cross-reactive immune response,” says Karlsson, though their sample is too small to say if this finding applies more broadly across the population. The vast majority of children as young as two years had OC43-specific mCD4+ T cell responses. In adulthood, the functionality of both the OC43-specific and the cross-reactive T cells wane significantly, especially with advanced age.
“Considering that the mortality rate in children is the lowest from ages five to nine, and higher in younger children, our results imply that cross-reactive mCD4+ T cells may have a role in the control of SARS-CoV-2 infection in children,” the authors wrote in their paper.
“One of the most politicized aspects of our pandemic response was not accepting that children are so much less at risk for severe disease with COVID-19,” because usually young children are among the most vulnerable to pathogens, says Monica Gandhi, professor of medicine at the University of California San Francisco and author of the book, Endemic: A Post-Pandemic Playbook, to be released by the Mayo Clinic Press this summer. The immune response of kids to SARS-CoV-2 stood our expectations on their head. “We just haven't seen this before, so knowing the mechanism of protection is really important.”
Why the T cell immune response can fade with age is largely unknown. With some viruses such as measles, a single vaccination or infection generates life-long protection. But respiratory tract infections, like SARS-CoV-2, cause a localized infection - specific to certain organs - and that response tends to be shorter lived than systemic infections that affect the entire body. Karlsson suspects the elderly might be exposed to these localized types of viruses less often. Also, frequent continued exposure to a virus that results in reactivation of the memory T cell pool might eventually result in “a kind of immunosenescence or immune exhaustion that is associated with aging,” Karlsson says. https://leaps.org/scientists-just-started-testing-a-new-class-of-drugs-to-slow-and-even-reverse-aging/particle-3 This fading protection is why older people need to be repeatedly vaccinated against SARS-CoV-2.
Policy implications
Following the numbers on COVID-19 infections and severity over the last three years have shown us that healthy young people without risk factors are not likely to develop serious disease. This latest study points to a mechanism that helps explain why. But the inertia of existing policies remains. How should we adjust policy recommendations based on what we know today?
The World Health Organization (WHO) updated their COVID-19 vaccination guidance on March 28. It calls for a focus on vaccinating and boosting those at risk for developing serious disease. The guidance basically shrugged its shoulders when it came to healthy children and young adults receiving vaccinations and boosters against COVID-19. It said the priority should be to administer the “traditional essential vaccines for children,” such as those that protect against measles, rubella, and mumps.
“As an immunologist and a mother, I think that catching a cold or two when you are a kid and otherwise healthy is not that bad for you. Children have a much lower risk of becoming severely ill with SARS-CoV-2,” says Karlsson. She has followed public health guidance in Sweden, which means that her young children have not been vaccinated, but being older, she has received the vaccine and boosters. Gandhi and her children have been vaccinated, but they do not plan on additional boosters.
The WHO got it right in “concentrating on what matters,” which is getting traditional childhood immunizations back on track after their dramatic decline over the last three years, says Gandhi. Nor is there a need for masking in schools, according to a study from the Catalonia region of Spain. It found “no difference in masking and spread in schools,” particularly since tracking data indicate that nearly all young people have been exposed to SARS-CoV-2.
Both researchers lament that public discussion has overemphasized the quickly fading antibody part of the immune response to SARS-CoV-2 compared with the more durable T cell component. They say developing an efficient measure of T cell response for doctors to use in the clinic would help to monitor immunity in people at risk for severe cases of COVID-19 compared with the current method of toting up potential risk factors.
In this week's Friday Five: The eyes are the windows to the soul - and biological aging?
Plus, what bean genes mean for health and the planet, a breathing practice that could lower levels of tau proteins in the brain, AI beats humans at assessing heart health, and the benefits of "nature prescriptions"
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on new scientific theories and progress to give you a therapeutic dose of inspiration headed into the weekend.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Here are the stories covered this week:
- The eyes are the windows to the soul - and biological aging?
- What bean genes mean for health and the planet
- This breathing practice could lower levels of tau proteins
- AI beats humans at assessing heart health
- Should you get a nature prescription?