How 30 Years of Heart Surgeries Taught My Dad How to Live
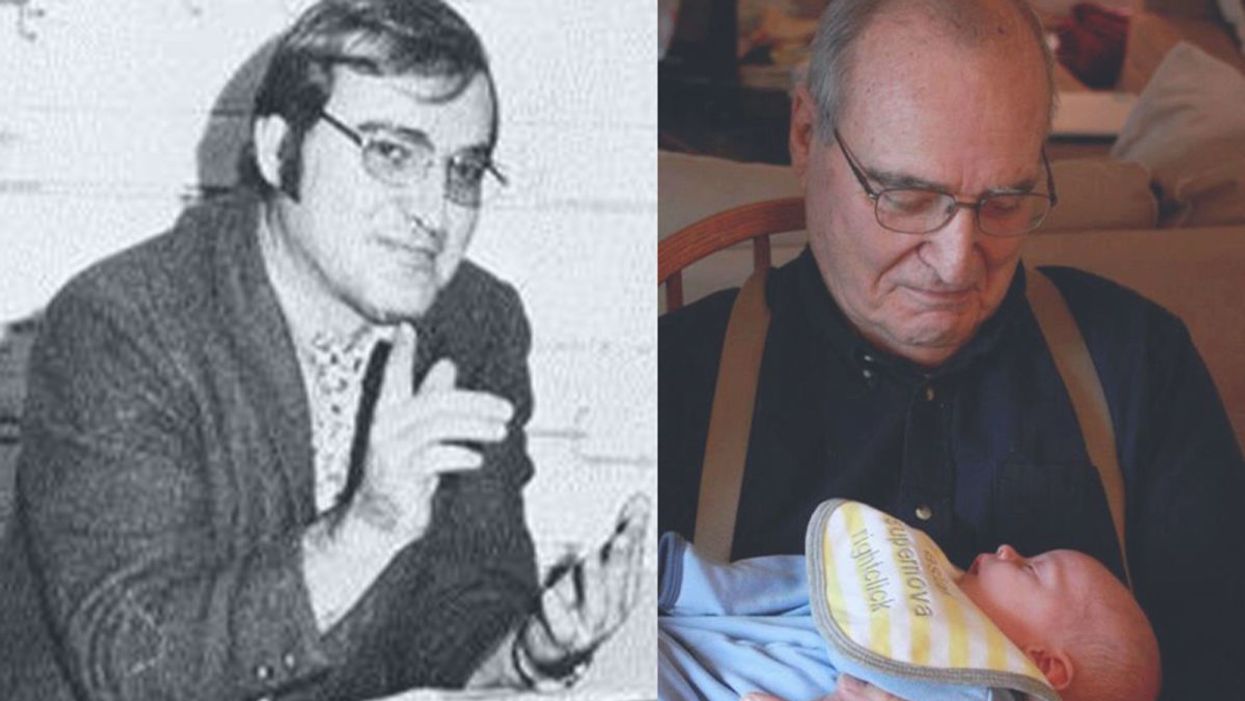
A mid-1970s photo of the author's father, and him holding a grandchild in 2012.
[Editor's Note: This piece is the winner of our 2019 essay contest, which prompted readers to reflect on the question: "How has an advance in science or medicine changed your life?"]
My father did not expect to live past the age of 50. Neither of his parents had done so. And he also knew how he would die: by heart attack, just as his father did.
In July of 1976, he had his first heart attack, days before his 40th birthday.
My dad lived the first 40 years of his life with this knowledge buried in his bones. He started smoking at the age of 12, and was drinking before he was old enough to enlist in the Navy. He had a sarcastic, often cruel, sense of humor that could drive my mother, my sister and me into tears. He was not an easy man to live with, but that was okay by him - he didn't expect to live long.
In July of 1976, he had his first heart attack, days before his 40th birthday. I was 13, and my sister was 11. He needed quadruple bypass surgery. Our small town hospital was not equipped to do this type of surgery; he would have to be transported 40 miles away to a heart center. I understood this journey to mean that my father was seriously ill, and might die in the hospital, away from anyone he knew. And my father knew a lot of people - he was a popular high school English teacher, in a town with only three high schools. He knew generations of students and their parents. Our high school football team did a blood drive in his honor.

During a trip to Disney World in 1974, Dad was suffering from angina the entire time but refused to tell me (left) and my sister, Kris.
Quadruple bypass surgery in 1976 meant that my father's breastbone was cut open by a sternal saw. His ribcage was spread wide. After the bypass surgery, his bones would be pulled back together, and tied in place with wire. The wire would later be pulled out of his body when the bones knitted back together. It would take months before he was fully healed.
Dad was in the hospital for the rest of the summer and into the start of the new school year. Going to visit him was farther than I could ride my bicycle; it meant planning a trip in the car and going onto the interstate. The first time I was allowed to visit him in the ICU, he was lying in bed, and then pushed himself to sit up. The heart monitor he was attached to spiked up and down, and I fainted. I didn't know that heartbeats change when you move; television medical dramas never showed that - I honestly thought that I had driven my father into another heart attack.
Only a few short years after that, my father returned to the big hospital to have his heart checked with a new advance in heart treatment: a CT scan. This would allow doctors to check for clogged arteries and treat them before a fatal heart attack. The procedure identified a dangerous blockage, and my father was admitted immediately. This time, however, there was no need to break bones to get to the problem; my father was home within a month.
During the late 1970's, my father changed none of his habits. He was still smoking, and he continued to drink. But now, he was also taking pills - pills to manage the pain. He would pop a nitroglycerin tablet under his tongue whenever he was experiencing angina (I have a vivid memory of him doing this during my driving lessons), but he never mentioned that he was in pain. Instead, he would snap at one of us, or joke that we were killing him.
I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count.
Being the kind of guy he was, my father never wanted to talk about his health. Any admission of pain implied that he couldn't handle pain. He would try to "muscle through" his angina, as if his willpower would be stronger than his heart muscle. His efforts would inevitably fail, leaving him angry and ready to lash out at anyone or anything. He would blame one of us as a reason he "had" to take valium or pop a nitro tablet. Dinners often ended in shouts and tears, and my father stalking to the television room with a bottle of red wine.
In the 1980's while I was in college, my father had another heart attack. But now, less than 10 years after his first, medicine had changed: our hometown hospital had the technology to run dye through my father's blood stream, identify the blockages, and do preventative care that involved statins and blood thinners. In one case, the doctors would take blood vessels from my father's legs, and suture them to replace damaged arteries around his heart. New advances in cholesterol medication and treatments for angina could extend my father's life by many years.
My father decided it was time to quit smoking. It was the first significant health step I had ever seen him take. Until then, he treated his heart issues as if they were inevitable, and there was nothing that he could do to change what was happening to him. Quitting smoking was the first sign that my father was beginning to move out of his fatalistic mindset - and the accompanying fatal behaviors that all pointed to an early death.
In 1986, my father turned 50. He had now lived longer than either of his parents. The habits he had learned from them could be changed. He had stopped smoking - what else could he do?
It was a painful decade for all of us. My parents divorced. My sister quit college. I moved to the other side of the country and stopped speaking to my father for almost 10 years. My father remarried, and divorced a second time. I stopped counting the number of times he was in and out of the hospital with heart-related issues.
In the early 1990's, my father reached out to me. I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count. He traveled across the country to spend a week with me, to meet my friends, and to rebuild his relationship with me. He did the same with my sister. He stopped drinking. He was more forthcoming about his health, and admitted that he was taking an antidepressant. His humor became less cruel and sadistic. He took an active interest in the world. He became part of my life again.
The 1990's was also the decade of angioplasty. My father explained it to me like this: during his next surgery, the doctors would place balloons in his arteries, and inflate them. The balloons would then be removed (or dissolve), leaving the artery open again for blood. He had several of these surgeries over the next decade.
When my father was in his 60's, he danced at with me at my wedding. It was now 10 years past the time he had expected to live, and his life was transformed. He was living with a woman I had known since I was a child, and my wife and I would make regular visits to their home. My father retired from teaching, became an avid gardener, and always had a home project underway. He was a happy man.

Dancing with my father at my wedding in 1998.
Then, in the mid 2000's, my father faced another serious surgery. Years of arterial surgery, angioplasty, and damaged heart muscle were taking their toll. He opted to undergo a life-saving surgery at Cleveland Clinic. By this time, I was living in New York and my sister was living in Arizona. We both traveled to the Midwest to be with him. Dad was unconscious most of the time. We took turns holding his hand in the ICU, encouraging him to regain his will to live, and making outrageous threats if he didn't listen to us.
The nursing staff were wonderful. I remember telling them that my father had never expected to live this long. One of the nurses pointed out that most of the patients in their ward were in their 70's and 80's, and a few were in their 90's. She reminded me that just a decade earlier, most hospitals were unwilling to do the kind of surgery my father had received on patients his age. In the first decade of the 21st century, however, things were different: 90-year-olds could now undergo heart surgery and live another decade. My father was on the "young" side of their patients.
The Cleveland Clinic visit would be the last major heart surgery my father would have. Not that he didn't return to his local hospital a few times after that: he broke his neck -- not once, but twice! -- slipping on ice. And in the 2010's, he began to show signs of dementia, and needed more home care. His partner, who had her own health issues, was not able to provide the level of care my father needed. My sister invited him to move in with her, and in 2015, I traveled with him to Arizona to get him settled in.
After a few months, he accepted home hospice. We turned off his pacemaker when the hospice nurse explained to us that the job of a pacemaker is to literally jolt a patient's heart back into beating. The jolts were happening more and more frequently, causing my Dad additional, unwanted pain.

My father in 2015, a few months before his death.
My father died in February 2016. His body carried the scars and implants of 30 years of cardiac surgeries, from the ugly breastbone scar from the 1970's to scars on his arms and legs from borrowed blood vessels, to the tiny red circles of robotic incisions from the 21st century. The arteries and veins feeding his heart were a patchwork of transplanted leg veins and fragile arterial walls pressed thinner by balloons.
And my father died with no regrets or unfinished business. He died in my sister's home, with his long-time partner by his side. Medical advancements had given him the opportunity to live 30 years longer than he expected. But he was the one who decided how to live those extra years. He was the one who made the years matter.
In this week's Friday Five, attending sports events is linked to greater life satisfaction, AI can identify specific brain tumors in under 90 seconds, LSD - minus hallucinations - raises hopes for mental health, new research on the benefits of cold showers, and inspiring awe in your kids leads to behavior change.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on new scientific theories and progress to give you a therapeutic dose of inspiration headed into the weekend.
This episode includes an interview with Dr. Helen Keyes, Head of the School of Psychology and Sports Science at Anglia Ruskin University.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
- Attending sports events is linked to greater life satisfaction
- Identifying specific brain tumors in under 90 seconds with AI
- LSD - minus hallucinations - raises hopes for mental health
- New research on the benefits of cold showers
- Inspire awe in your kids and reap the benefits
Residents of Fountain Hills, a small town near Phoenix, Arizona, fought against the night sky pollution to restore their Milky Way skies.
As a graduate student in observational astronomy at the University of Arizona during the 1970s, Diane Turnshek remembers the starry skies above the Kitt Peak National Observatory on the Tucson outskirts. Back then, she could observe faint objects like nebulae, galaxies, and star clusters on most nights.
When Turnshek moved to Pittsburgh in 1981, she found it almost impossible to see a clear night sky because the city’s countless lights created a bright dome of light called skyglow. Over the next two decades, Turnshek almost forgot what a dark sky looked like. She witnessed pristine dark skies in their full glory again during a visit to the Mars Desert Research Station in Utah in early 2000s.
“I was shocked at how beautiful the dark skies were in the West. That is when I realized that most parts of the world have lost access to starry skies because of light pollution,” says Turnshek, an astronomer and lecturer at Carnegie Mellon University. In 2015, she became a dark sky advocate.
Light pollution is defined as the excessive or wasteful use of artificial light.
Light-emitting diodes (LEDs) -- which became commercially available in 2002 and rapidly gained popularity in offices, schools, and hospitals when their price dropped six years later — inadvertently fueled the surge in light pollution. As traditional light sources like halogen, fluorescent, mercury, and sodium vapor lamps have been phased out or banned, LEDs became the main source of lighting globally in 2019. Switching to LEDs has been lauded as a win-win decision. Not only are they cheap but they also consume a fraction of electricity compared to their traditional counterparts.
But as cheap LED installations became omnipresent, they increased light pollution. “People have been installing LEDs thinking they are making a positive change for the environment. But LEDs are a lot brighter than traditional light sources,” explains Ashley Wilson, director of conservation at the International Dark-Sky Association (IDA). “Despite being energy-efficient, they are increasing our energy consumption. No one expected this kind of backlash from switching to LEDs.”
Light pollution impacts the circadian rhythms of all living beings — the natural internal process that regulates the sleep–wake cycle.
Currently, more than 80 percent of the world lives under light-polluted skies. In the U.S. and Europe, that figure is above 99 percent.
According to the IDA, $3 billion worth of electricity is lost to skyglow every year in the U.S. alone — thanks to unnecessary and poorly designed outdoor lighting installations. Worse, the resulting light pollution has insidious impacts on humans and wildlife — in more ways than one.
Disrupting the brain’s clock
Light pollution impacts the circadian rhythms of all living beings—the natural internal process that regulates the sleep–wake cycle. Humans and other mammals have neurons in their retina called intrinsically photosensitive retinal ganglion cells (ipRGCs). These cells collect information about the visual world and directly influence the brain’s biological clock in the hypothalamus.
The ipRGCs are particularly sensitive to the blue light that LEDs emit at high levels, resulting in suppression of melatonin, a hormone that helps us sleep. A 2020 JAMA Psychiatry study detailed how teenagers who lived in areas with bright outdoor lighting at night went to bed late and slept less, which made them more prone to mood disorders and anxiety.
“Many people are skeptical when they are told something as ubiquitous as lights could have such profound impacts on public health,” says Gena Glickman, director of the Chronobiology, Light and Sleep Lab at Uniformed Services University. “But when the clock in our brains gets exposed to blue light at nighttime, it could result in a lot of negative consequences like impaired cognitive function and neuro-endocrine disturbances.”
In the last 12 years, several studies indicated that light pollution exposure is associated with obesity and diabetes in humans and animals alike. While researchers are still trying to understand the exact underlying mechanisms, they found that even one night of too much light exposure could negatively affect the metabolic system. Studies have linked light pollution to a higher risk of hormone-sensitive cancers like breast and prostate cancer. A 2017 study found that female nurses exposed to light pollution have a 14 percent higher risk of breast cancer. The World Health Organization (WHO) identified long-term night shiftwork as a probable cause of cancer.
“We ignore our biological need for a natural light and dark cycle. Our patterns of light exposure have consequently become different from what nature intended,” explains Glickman.
Circadian lighting systems, designed to match individuals’ circadian rhythms, might help. The Lighting Research Center at Rensselaer Polytechnic Institute developed LED light systems that mimic natural lighting fluxes, required for better sleep. In the morning the lights shine brightly as does the sun. After sunset, the system dims, once again mimicking nature, which boosts melatonin production. It can even be programmed to increase blue light indoors when clouds block sunlight’s path through windows. Studies have shown that such systems might help reduce sleep fragmentation and cognitive decline. People who spend most of their day indoors can benefit from such circadian mimics.

When Diane Turnshek moved to Pittsburgh, she found it almost impossible to see a clear night sky because the city’s countless lights created a bright dome of light called skyglow.
Diane Turnshek
Leading to better LEDs
Light pollution disrupts the travels of millions of migratory birds that begin their long-distance journeys after sunset but end up entrapped within the sky glow of cities, becoming disoriented. A 2017 study in Nature found that nocturnal pollinators like bees, moths, fireflies and bats visit 62 percent fewer plants in areas with artificial lights compared to dark areas.
“On an evolutionary timescale, LEDs have triggered huge changes in the Earth’s environment within a relative blink of an eye,” says Wilson, the director of IDA. “Plants and animals cannot adapt so fast. They have to fight to survive with their existing traits and abilities.”
But not all types of LEDs are inherently bad -- it all comes down to how much blue light they emit. During the day, the sun emits blue light waves. By sunset, red and orange light waves become predominant, stimulating melatonin production. LED’s artificial blue light, when shining at night, disrupts that. For some unknown reason, there are more bluer color LEDs made and sold.
“Communities install blue color temperature LEDs rather than redder color temperature LEDs because more of the blue ones are made; they are the status quo on the market,” says Michelle Wooten, an assistant professor of astronomy at the University of Alabama at Birmingham.
Most artificial outdoor light produced is wasted as human eyes do not use them to navigate their surroundings.
While astronomers and the IDA have been educating LED manufacturers about these nuances, policymakers struggle to keep up with the growing industry. But there are things they can do—such as requiring LEDs to include dimmers. “Most LED installations can be dimmed down. We need to make the dimmable drivers a mandatory requirement while selling LED lighting,” says Nancy Clanton, a lighting engineer, designer, and dark sky advocate.
Some lighting companies have been developing more sophisticated LED lights that help support melatonin production. Lighting engineers at Crossroads LLC and Nichia Corporation have been working on creating LEDs that produce more light in the red range. “We live in a wonderful age of technology that has given us these new LED designs which cut out blue wavelengths entirely for dark-sky friendly lighting purposes,” says Wooten.
Dimming the lights to see better
The IDA and advocates like Turnshek propose that communities turn off unnecessary outdoor lights. According to the Department of Energy, 99 percent of artificial outdoor light produced is wasted as human eyes do not use them to navigate their surroundings.
In recent years, major cities like Chicago, Austin, and Philadelphia adopted the “Lights Out” initiative encouraging communities to turn off unnecessary lights during birds’ peak migration seasons for 10 days at a time. “This poses an important question: if people can live without some lights for 10 days, why can’t they keep them turned off all year round,” says Wilson.
Most communities globally believe that keeping bright outdoor lights on all night increases security and prevents crime. But in her studies of street lights’ brightness levels in different parts of the US — from Alaska to California to Washington — Clanton found that people felt safe and could see clearly even at low or dim lighting levels.
Clanton and colleagues installed LEDs in a Seattle suburb that provided only 25 percent of lighting levels compared to what they used previously. The residents reported far better visibility because the new LEDs did not produce glare. “Visual contrast matters a lot more than lighting levels,” Clanton says. Additionally, motion sensor LEDs for outdoor lighting can go a long way in reducing light pollution.
Flipping a switch to preserve starry nights
Clanton has helped draft laws to reduce light pollution in at least 17 U.S. states. However, poor awareness of light pollution led to inadequate enforcement of these laws. Also, getting thousands of counties and municipalities within any state to comply with these regulations is a Herculean task, Turnshek points out.
Fountain Hills, a small town near Phoenix, Arizona, has rid itself of light pollution since 2018, thanks to the community's efforts to preserve dark skies.
Until LEDs became mainstream, Fountain Hills enjoyed starry skies despite its proximity to Phoenix. A mountain surrounding the town blocks most of the skyglow from the city.
“Light pollution became an issue in Fountain Hills over the years because we were not taking new LED technologies into account. Our town’s lighting code was antiquated and out-of-date,” says Vicky Derksen, a resident who is also a part of the Fountain Hills Dark Sky Association founded in 2017. “To preserve dark skies, we had to work with the entire town to update the local lighting code and convince residents to follow responsible outdoor lighting practices.”
Derksen and her team first tackled light pollution in the town center which has a faux fountain in the middle of a lake. “The iconic centerpiece, from which Fountain Hills got its name, had the wrong types of lighting fixtures, which created a lot of glare,” adds Derksen. They then replaced several other municipal lighting fixtures with dark-sky-friendly LEDs.
The results were awe-inspiring. After a long time, residents could see the Milky Way with crystal clear clarity. Star-gazing activities made a strong comeback across the town. But keeping light pollution low requires constant work.
Derksen and other residents regularly measure artificial light levels in
Fountain Hills. Currently, the only major source of light pollution is from extremely bright, illuminated signs which local businesses had installed in different parts of the town. While Derksen says it is an uphill battle to educate local businesses about light pollution, Fountain Hills residents are determined to protect their dark skies.
“When a river gets polluted, it can take several years before clean-up efforts see any tangible results,” says Derksen. “But the effects are immediate when you work toward reducing light pollution. All it requires is flipping a switch.”