How Can We Decide If a Biomedical Advance Is Ethical?

A newborn in the maternity ward. (© rufous/Fotolia)
"All fixed, fast-frozen relations, with their train of ancient and venerable prejudices and opinions, are swept away, all new-formed ones become antiquated before they can ossify. All that is solid melts into air, all that is holy is profaned…"
On July 25, 1978, Louise Brown was born in Oldham, England, the first human born through in vitro fertilization, through the work of Patrick Steptoe, a gynecologist, and Robert Edwards, a physiologist. Her birth was greeted with strong (though not universal) expressions of ethical dismay. Yet in 2016, the latest year for which we have data, nearly two percent of the babies born in the United States – and around the same percentage throughout the developed world – were the result of IVF. Few, if any, think of these children as unnatural, monsters, or freaks or of their parents as anything other than fortunate.
How should we view Dr. He today, knowing that the world's eventual verdict on the ethics of biomedical technologies often changes?
On November 25, 2018, news broke that Chinese scientist, Dr. He Jiankui, claimed to have edited the genomes of embryos, two of whom had recently become the new babies, Lulu and Nana. The response was immediate and overwhelmingly negative.
Times change. So do views. How will Dr. He be viewed in 40 years? And, more importantly, how should we view him today, knowing that the world's eventual verdict on the ethics of biomedical technologies often changes? And when what biomedicine can do changes with vertiginous frequency?
How to determine what is and isn't ethical is above my pay grade. I'm a simple law professor – I can't claim any deeper insight into how to live a moral life than the millennia of religious leaders, philosophers, ethicists, and ordinary people trying to do the right thing. But I can point out some ways to think about these questions that may be helpful.
First, consider two different kinds of ethical commands. Some are quite specific – "thou shalt not kill," for example. Others are more general – two of them are "do unto others as you would have done to you" or "seek the greatest good for the greatest number."
Biomedicine in the last two centuries has often surprised us with new possibilities, situations that cultures, religions, and bodies of ethical thought had not previously had to consider, from vaccination to anesthesia for women in labor to genome editing. Sometimes these possibilities will violate important and deeply accepted precepts for a group or a person. The rise of blood transfusions around World War I created new problems for Jehovah's Witnesses, who believe that the Bible prohibits ingesting blood. The 20th century developments of artificial insemination and IVF both ran afoul of Catholic doctrine prohibiting methods other than "traditional" marital intercourse for conceiving children. If you subscribe to an ethical or moral code that contains prohibitions that modern biomedicine violates, the issue for you is stark – adhere to those beliefs or renounce them.
If the harms seem to outweigh the benefits, it's easy to conclude "this is worrisome."
But many biomedical changes violate no clear moral teachings. Is it ethical or not to edit the DNA of embryos? Not surprisingly, the sacred texts of various religions – few of which were created after, at the latest, the early 19th century, say nothing specific about this. There may be hints, precedents, leanings that could argue one way or another, but no "commandments." In that case, I recommend, at least as a starting point, asking "what are the likely consequences of these actions?"
Will people be, on balance, harmed or helped by them? "Consequentialist" approaches, of various types, are a vast branch of ethical theories. Personally I find a completely consequentialist approach unacceptable – I could not accept, for example, torturing an innocent child even in order to save many lives. But, in the absence of a clear rule, looking at the consequences is a great place to start. If the harms seem to outweigh the benefits, it's easy to conclude "this is worrisome."
Let's use that starting place to look at a few bioethical issues. IVF, for example, once proven (relatively) safe seems to harm no one and to help many, notably the more than 8 million children worldwide born through IVF since 1978 – and their 16 million parents. On the other hand, giving unknowing, and unconsenting, intellectually disabled children hepatitis A harmed them, for an uncertain gain for science. And freezing the heads of the dead seems unlikely to harm anyone alive (except financially) but it also seems almost certain not to benefit anyone. (Those frozen dead heads are not coming back to life.)
Now let's look at two different kinds of biomedical advances. Some are controversial just because they are new; others are controversial because they cut close to the bone – whether or not they violate pre-established ethical or moral norms, they clearly relate to them.
Consider anesthesia during childbirth. When first used, it was controversial. After all, said critics, in Genesis, the Bible says God told Eve, "I will greatly multiply Your pain in childbirth, In pain you will bring forth children." But it did not clearly prohibit pain relief and from the advent of ether on, anesthesia has been common, though not universal, in childbirth in western societies. The pre-existing ethical precepts were not clear and the consequences weighed heavily in favor of anesthesia. Similarly, vaccination seems to violate no deep moral principle. It was, and for some people, still is just strange, and unnatural. The same was true of IVF initially. Opposition to all of these has faded with time and familiarity. It has not disappeared – some people continue to find moral or philosophical problems with "unnatural" childbirth, vaccination, and IVF – but far fewer.
On the other hand, human embryonic stem cell research touches deeper issues. Human embryos are destroyed to make those stem cells. Reasonable people disagree on the moral status of the human embryo, and the moral weight of its destruction, but it does at least bring into play clear and broadly accepted moral precepts, such as "Thou shalt not kill." So, at the far side of an individual's time, does euthanasia. More exposure to, and familiarity with, these practices will not necessarily lead to broad acceptance as the objections involve more than novelty.
The first is "what would I do?" The second – what should my government, culture, religion allow or forbid?
Finally, all this ethical analysis must work at two levels. The first is "what would I do?" The second – what should my government, culture, religion allow or forbid? There are many things I would not do that I don't think should be banned – because I think other people may reasonably have different views from mine. I would not get cosmetic surgery, but I would not ban it – and will try not to think ill of those who choose it
So, how should we assess the ethics of new biomedical procedures when we know that society's views may change? More specifically, what should we think of He Jiankui's experiment with human babies?
First, look to see whether the procedure in question violates, at least fairly clearly, some rule in your ethical or moral code. If so, your choice may not be difficult. But if the procedure is unmentioned in your moral code, probably because it was inconceivable to the code's creators, examine the consequences of the act.
If the procedure is just novel, and not something that touches on important moral concerns, looking at the likely consequences may be enough for your ethical analysis –though it is always worth remembering that predicting consequences perfectly is impossible and predicting them well is never certain. If it does touch on morally significant issues, you need to think those issues through. The consequences may be important to your conclusions but they may not be determinative.
And, then, if you conclude that it is not ethical from your perspective, you need to take yet another step and consider whether it should be banned for people who do not share your perspective. Sometimes the answer will be yes – that psychopaths may not view murder as immoral does not mean we have to let them kill – but sometimes it will be no.
What does this say about He Jiankui's experiment? I have no qualms in condemning it, unequivocally. The potential risks to the babies grossly outweighed any benefits to them, and to science. And his secret work, against a near universal scientific consensus, privileged his own ethical conclusions without giving anyone else a vote, or even a voice.
But if, in ten or twenty years, genome editing of human embryos is shown to be safe (enough) and it is proposed to be used for good reasons – say, to relieve human suffering that could not be treated in other good ways – and with good consents from those directly involved as well as from the relevant society and government – my answer might well change. Yours may not. Bioethics is a process for approaching questions; it is not a set of universal answers.
This article opened with a quotation from the 1848 Communist Manifesto, referring to the dizzying pace of change from industrialization and modernity. You don't need to be a Marxist to appreciate that sentiment. Change – especially in the biosciences – keeps accelerating. How should we assess the ethics of new biotechnologies? The best we can, with what we know, at the time we inhabit. And, in the face of vast uncertainty, with humility.
Nobel Prize goes to technology for mRNA vaccines
Katalin Karikó, pictured, and Drew Weissman won the Nobel Prize for advances in mRNA research that led to the first Covid vaccines.
When Drew Weissman received a call from Katalin Karikó in the early morning hours this past Monday, he assumed his longtime research partner was calling to share a nascent, nagging idea. Weissman, a professor of medicine at the Perelman School of Medicine at the University of Pennsylvania, and Karikó, a professor at Szeged University and an adjunct professor at UPenn, both struggle with sleep disturbances. Thus, middle-of-the-night discourses between the two, often over email, has been a staple of their friendship. But this time, Karikó had something more pressing and exciting to share: They had won the 2023 Nobel Prize in Physiology or Medicine.
The work for which they garnered the illustrious award and its accompanying $1,000,000 cash windfall was completed about two decades ago, wrought through long hours in the lab over many arduous years. But humanity collectively benefited from its life-saving outcome three years ago, when both Moderna and Pfizer/BioNTech’s mRNA vaccines against COVID were found to be safe and highly effective at preventing severe disease. Billions of doses have since been given out to protect humans from the upstart viral scourge.
“I thought of going somewhere else, or doing something else,” said Katalin Karikó. “I also thought maybe I’m not good enough, not smart enough. I tried to imagine: Everything is here, and I just have to do better experiments.”
Unlocking the power of mRNA
Weissman and Karikó unlocked mRNA vaccines for the world back in the early 2000s when they made a key breakthrough. Messenger RNA molecules are essentially instructions for cells’ ribosomes to make specific proteins, so in the 1980s and 1990s, researchers started wondering if sneaking mRNA into the body could trigger cells to manufacture antibodies, enzymes, or growth agents for protecting against infection, treating disease, or repairing tissues. But there was a big problem: injecting this synthetic mRNA triggered a dangerous, inflammatory immune response resulting in the mRNA’s destruction.
While most other researchers chose not to tackle this perplexing problem to instead pursue more lucrative and publishable exploits, Karikó stuck with it. The choice sent her academic career into depressing doldrums. Nobody would fund her work, publications dried up, and after six years as an assistant professor at the University of Pennsylvania, Karikó got demoted. She was going backward.
“I thought of going somewhere else, or doing something else,” Karikó told Stat in 2020. “I also thought maybe I’m not good enough, not smart enough. I tried to imagine: Everything is here, and I just have to do better experiments.”
A tale of tenacity
Collaborating with Drew Weissman, a new professor at the University of Pennsylvania, in the late 1990s helped provide Karikó with the tenacity to continue. Weissman nurtured a goal of developing a vaccine against HIV-1, and saw mRNA as a potential way to do it.
“For the 20 years that we’ve worked together before anybody knew what RNA is, or cared, it was the two of us literally side by side at a bench working together,” Weissman said in an interview with Adam Smith of the Nobel Foundation.
In 2005, the duo made their 2023 Nobel Prize-winning breakthrough, detailing it in a relatively small journal, Immunity. (Their paper was rejected by larger journals, including Science and Nature.) They figured out that chemically modifying the nucleoside bases that make up mRNA allowed the molecule to slip past the body’s immune defenses. Karikó and Weissman followed up that finding by creating mRNA that’s more efficiently translated within cells, greatly boosting protein production. In 2020, scientists at Moderna and BioNTech (where Karikó worked from 2013 to 2022) rushed to craft vaccines against COVID, putting their methods to life-saving use.
The future of vaccines
Buoyed by the resounding success of mRNA vaccines, scientists are now hurriedly researching ways to use mRNA medicine against other infectious diseases, cancer, and genetic disorders. The now ubiquitous efforts stand in stark contrast to Karikó and Weissman’s previously unheralded struggles years ago as they doggedly worked to realize a shared dream that so many others shied away from. Katalin Karikó and Drew Weissman were brave enough to walk a scientific path that very well could have ended in a dead end, and for that, they absolutely deserve their 2023 Nobel Prize.
This article originally appeared on Big Think, home of the brightest minds and biggest ideas of all time.
Scientists turn pee into power in Uganda
With conventional fuel cells as their model, researchers learned to use similar chemical reactions to make a fuel from microbes in pee.
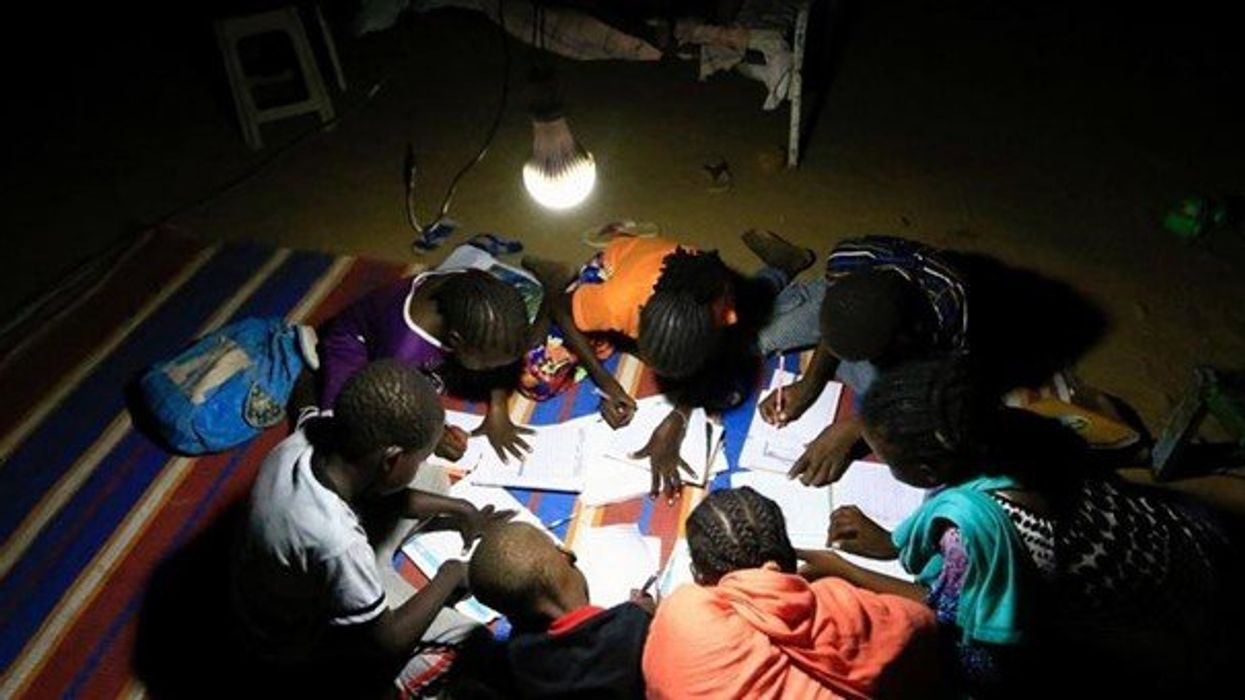
At the edge of a dirt road flanked by trees and green mountains outside the town of Kisoro, Uganda, sits the concrete building that houses Sesame Girls School, where girls aged 11 to 19 can live, learn and, at least for a while, safely use a toilet. In many developing regions, toileting at night is especially dangerous for children. Without electrical power for lighting, kids may fall into the deep pits of the latrines through broken or unsteady floorboards. Girls are sometimes assaulted by men who hide in the dark.
For the Sesame School girls, though, bright LED lights, connected to tiny gadgets, chased the fears away. They got to use new, clean toilets lit by the power of their own pee. Some girls even used the light provided by the latrines to study.
Urine, whether animal or human, is more than waste. It’s a cheap and abundant resource. Each day across the globe, 8.1 billion humans make 4 billion gallons of pee. Cows, pigs, deer, elephants and other animals add more. By spending money to get rid of it, we waste a renewable resource that can serve more than one purpose. Microorganisms that feed on nutrients in urine can be used in a microbial fuel cell that generates electricity – or "pee power," as the Sesame girls called it.
Plus, urine contains water, phosphorus, potassium and nitrogen, the key ingredients plants need to grow and survive. Human urine could replace about 25 percent of current nitrogen and phosphorous fertilizers worldwide and could save water for gardens and crops. The average U.S. resident flushes a toilet bowl containing only pee and paper about six to seven times a day, which adds up to about 3,500 gallons of water down per year. Plus cows in the U.S. produce 231 gallons of the stuff each year.
Pee power
A conventional fuel cell uses chemical reactions to produce energy, as electrons move from one electrode to another to power a lightbulb or phone. Ioannis Ieropoulos, a professor and chair of Environmental Engineering at the University of Southampton in England, realized the same type of reaction could be used to make a fuel from microbes in pee.
Bacterial species like Shewanella oneidensis and Pseudomonas aeruginosa can consume carbon and other nutrients in urine and pop out electrons as a result of their digestion. In a microbial fuel cell, one electrode is covered in microbes, immersed in urine and kept away from oxygen. Another electrode is in contact with oxygen. When the microbes feed on nutrients, they produce the electrons that flow through the circuit from one electrod to another to combine with oxygen on the other side. As long as the microbes have fresh pee to chomp on, electrons keep flowing. And after the microbes are done with the pee, it can be used as fertilizer.
These microbes are easily found in wastewater treatment plants, ponds, lakes, rivers or soil. Keeping them alive is the easy part, says Ieropoulos. Once the cells start producing stable power, his group sequences the microbes and keeps using them.
Like many promising technologies, scaling these devices for mass consumption won’t be easy, says Kevin Orner, a civil engineering professor at West Virginia University. But it’s moving in the right direction. Ieropoulos’s device has shrunk from the size of about three packs of cards to a large glue stick. It looks and works much like a AAA battery and produce about the same power. By itself, the device can barely power a light bulb, but when stacked together, they can do much more—just like photovoltaic cells in solar panels. His lab has produced 1760 fuel cells stacked together, and with manufacturing support, there’s no theoretical ceiling, he says.
Although pure urine produces the most power, Ieropoulos’s devices also work with the mixed liquids of the wastewater treatment plants, so they can be retrofit into urban wastewater utilities.
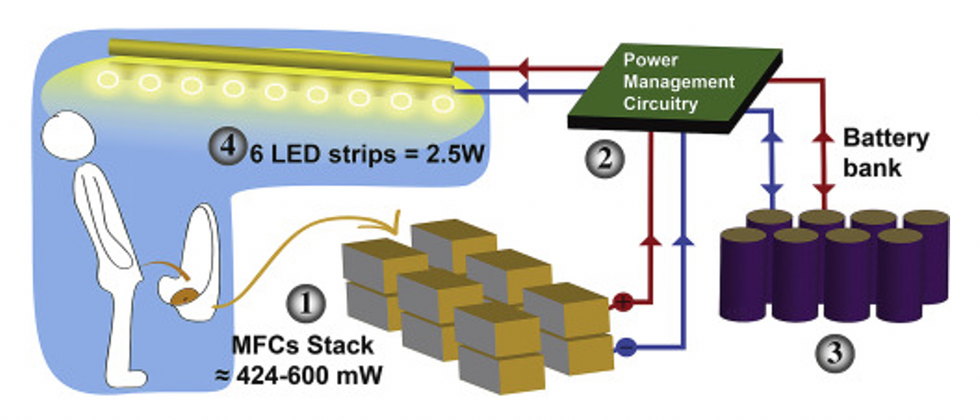
This image shows how the pee-powered system works. Pee feeds bacteria in the stack of fuel cells (1), which give off electrons (2) stored in parallel cylindrical cells (3). These cells are connected to a voltage regulator (4), which smooths out the electrical signal to ensure consistent power to the LED strips lighting the toilet.
Courtesy Ioannis Ieropoulos
Key to the long-term success of any urine reclamation effort, says Orner, is avoiding what he calls “parachute engineering”—when well-meaning scientists solve a problem with novel tech and then abandon it. “The way around that is to have either the need come from the community or to have an organization in a community that is committed to seeing a project operate and maintained,” he says.
Success with urine reclamation also depends on the economy. “If energy prices are low, it may not make sense to recover energy,” says Orner. “But right now, fertilizer prices worldwide are generally pretty high, so it may make sense to recover fertilizer and nutrients.” There are obstacles, too, such as few incentives for builders to incorporate urine recycling into new construction. And any hiccups like leaks or waste seepage will cost builders money and reputation. Right now, Orner says, the risks are just too high.
Despite the challenges, Ieropoulos envisions a future in which urine is passed through microbial fuel cells at wastewater treatment plants, retrofitted septic tanks, and building basements, and is then delivered to businesses to use as agricultural fertilizers. Although pure urine produces the most power, Ieropoulos’s devices also work with the mixed liquids of the wastewater treatment plants, so they can be retrofitted into urban wastewater utilities where they can make electricity from the effluent. And unlike solar cells, which are a common target of theft in some areas, nobody wants to steal a bunch of pee.
When Ieropoulos’s team returned to wrap up their pilot project 18 months later, the school’s director begged them to leave the fuel cells in place—because they made a major difference in students’ lives. “We replaced it with a substantial photovoltaic panel,” says Ieropoulos, They couldn’t leave the units forever, he explained, because of intellectual property reasons—their funders worried about theft of both the technology and the idea. But the photovoltaic replacement could be stolen, too, leaving the girls in the dark.
The story repeated itself at another school, in Nairobi, Kenya, as well as in an informal settlement in Durban, South Africa. Each time, Ieropoulos vowed to return. Though the pandemic has delayed his promise, he is resolute about continuing his work—it is a moral and legal obligation. “We've made a commitment to ourselves and to the pupils,” he says. “That's why we need to go back.”
Urine as fertilizer
Modern day industrial systems perpetuate the broken cycle of nutrients. When plants grow, they use up nutrients the soil. We eat the plans and excrete some of the nutrients we pass them into rivers and oceans. As a result, farmers must keep fertilizing the fields while our waste keeps fertilizing the waterways, where the algae, overfertilized with nitrogen, phosphorous and other nutrients grows out of control, sucking up oxygen that other marine species need to live. Few global communities remain untouched by the related challenges this broken chain create: insufficient clean water, food, and energy, and too much human and animal waste.
The Rich Earth Institute in Vermont runs a community-wide urine nutrient recovery program, which collects urine from homes and businesses, transports it for processing, and then supplies it as fertilizer to local farms.
One solution to this broken cycle is reclaiming urine and returning it back to the land. The Rich Earth Institute in Vermont is one of several organizations around the world working to divert and save urine for agricultural use. “The urine produced by an adult in one day contains enough fertilizer to grow all the wheat in one loaf of bread,” states their website.
Notably, while urine is not entirely sterile, it tends to harbor fewer pathogens than feces. That’s largely because urine has less organic matter and therefore less food for pathogens to feed on, but also because the urinary tract and the bladder have built-in antimicrobial defenses that kill many germs. In fact, the Rich Earth Institute says it’s safe to put your own urine onto crops grown for home consumption. Nonetheless, you’ll want to dilute it first because pee usually has too much nitrogen and can cause “fertilizer burn” if applied straight without dilution. Other projects to turn urine into fertilizer are in progress in Niger, South Africa, Kenya, Ethiopia, Sweden, Switzerland, The Netherlands, Australia, and France.
Eleven years ago, the Institute started a program that collects urine from homes and businesses, transports it for processing, and then supplies it as fertilizer to local farms. By 2021, the program included 180 donors producing over 12,000 gallons of urine each year. This urine is helping to fertilize hay fields at four partnering farms. Orner, the West Virginia professor, sees it as a success story. “They've shown how you can do this right--implementing it at a community level scale."