How One Doctor Single-Handedly Saved Countless Babies from Birth Defects

President John F. Kennedy gave Dr. Frances Oldham Kelsey the nation's highest federal civilian service award in 1962, saying she had "prevented a major tragedy of birth deformities."
In July 1956, a new drug hit the European market for the first time. The drug was called thalidomide – a sedative that was considered so safe it was available without a prescription.
Sedatives were in high demand in post-war Europe – but barbiturates, the most widely-used sedative at the time, caused overdoses and death when consumers took more than the recommended amount. Thalidomide, on the other hand, didn't appear to cause any side effects at all: Chemie Grünenthal, thalidomide's manufacturer, dosed laboratory rodents with over 600 times the normal dosage during clinical testing and had observed no evidence of toxicity.
The drug therefore was considered universally safe, and Grünenthal supplied thousands of doctors with samples to give to their patients. Doctors were encouraged to recommend thalidomide to their pregnant patients specifically because it was so safe, in order to relieve the nausea and insomnia associated with the first trimester of pregnancy.
By 1960, Thalidomide was being sold in countries throughout the world, and the United States was expected to soon follow suit. Dr. Frances Oldham Kelsey, a pharmacologist and physician, was hired by the Food and Drug Administration (FDA) in September of that year to review and approve drugs for the administration. Immediately, Kelsey was tasked with approving thalidomide for commercial use in the United States under the name Kevadon. Kelsey's approval was supposed to be a formality, since the drug was so widely used in other countries.
But Kelsey did something that few people expected – she paused. Rather than approving the drug offhand as she was expected to do, Kelsey asked the manufacturer – William S. Merrell Co., who was manufacturing thalidomide under license from Chemie Grünenthal – to supply her with more safety data, noting that Merrell's application for approval relied mostly on anecdotal testimony. Kelsey – along with her husband who worked as a pharmacologist at the National Institutes of Health (NIH) — was highly suspicious of a drug that had no lethal dose and no side effects. "It was just too positive," Kelsey said later. "This couldn't be the perfect drug with no risk."
At the same time, rumors were starting to swirl across Europe that thalidomide was not as safe as everyone had initially thought: Physicians were starting to notice an "unusual increase" in the birth of severely deformed babies, and they were beginning to suspect thalidomide as the cause. The babies, whose mothers had all taken thalidomide during pregnancy, were born with conditions like deafness, blindness, congenital heart problems, and even phocomelia, a malformation of the arms and legs. Doctors and midwives were also starting to notice a sharp rise in miscarriages and stillbirths among their patients as well.
Kelsey's skepticism was rewarded in November 1961 when thalidomide was yanked abruptly off the market, following a growing outcry that it was responsible for hundreds of stillbirths and deformities.
Kelsey had heard none of these rumors, but she did know from her post-doctoral research that adults could metabolize drugs differently than fetuses – in other words, a drug that was perfectly safe for adults could be detrimental to a patient's unborn child. Noting that thalidomide could cross the placental barrier, she asked for safety data, such as clinical trials, that showed specifically the drug was non-toxic for fetuses. Merrell supplied Kelsey with anecdotal data – in other words, accounts from patients who attested to the fact that they took thalidomide with no adverse effects – but she rejected it, needing stronger data: clinical studies with pregnant women included.
The drug company was annoyed at what they considered Kelsey's needless bureaucracy. After all, Germans were consuming around 1 million doses of thalidomide every day in 1960, with lots of anecdotal evidence that it was safe, even among pregnant women. As the holidays approached – the most lucrative time of year for sedative sales – Merrell executives started hounding Kelsey to approve thalidomide, even phoning her superior and paying her visits at work. But Kelsey was unmovable. Kelsey's skepticism was solidified in December 1960, when she read a letter published in the British Medical Journal from a physician. In the letter, the author warned that his long-term thalidomide patients were starting to report pain in their arms and legs.
"The burden of proof that the drug is safe … lies with the applicant," Kelsey wrote in a letter to Merrell executive Joseph F. Murray in May of 1961. Despite increasing pressure, Kelsey held fast to her insistence that more safety data – particularly for fetuses – was needed.
Kelsey's skepticism was rewarded in November 1961 when Chemie Grünenthal yanked thalidomide off the market overseas, following a growing outcry that it was responsible for hundreds of stillbirths and deformities. In early 1962, Merrell conceded that the drug's safety was unproven in fetuses and formally withdrew its application at the FDA.
Thanks to Kelsey, the United States was spared the effects of thalidomide – although countries like Europe and Canada were not so lucky. Thalidomide remained in people's homes under different names long after it was pulled from the market, and so women unfortunately continued to take thalidomide during their pregnancies, unaware of its effects. All told, thalidomide is thought to have caused around 10,000 birth defects and anywhere from 5,000 to 7,000 miscarriages. Many so-called "thalidomide babies" are now adults living with disabilities.

Niko von Glasow, born in 1960, is a German film director and producer who was born disabled due to the side effects of thalidomide.
Wikimedia Commons
Just two years after joining the FDA, Kelsey was presented with the President's Award for Distinguished Federal Civilian Service and was appointed as the head of the Investigational Drug Branch at the FDA. Not only did Kelsey save the U.S. public from the horrific effects of thalidomide, but she forever changed the way drugs were developed and approved for use in the United States: Drugs now need to not only be proven safe and effective, but adverse drug reactions need to be reported to the FDA and informed consent must be obtained by all participants before they volunteer for clinical trials. Today, the United States is safer because of Frances Kelsey's bravery.
Thanks to safety cautions from the COVID-19 pandemic, a strain of influenza has been completely eliminated.
If you were one of the millions who masked up, washed your hands thoroughly and socially distanced, pat yourself on the back—you may have helped change the course of human history.
Scientists say that thanks to these safety precautions, which were introduced in early 2020 as a way to stop transmission of the novel COVID-19 virus, a strain of influenza has been completely eliminated. This marks the first time in human history that a virus has been wiped out through non-pharmaceutical interventions, such as vaccines.
The flu shot, explained
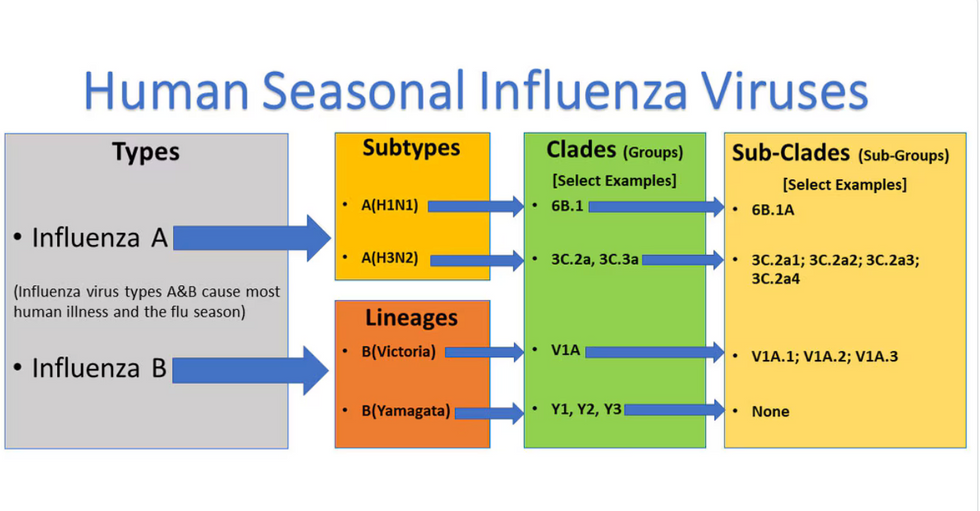
Influenza viruses type A and B are responsible for the majority of human illnesses and the flu season.
Centers for Disease Control
For more than a decade, flu shots have protected against two types of the influenza virus–type A and type B. While there are four different strains of influenza in existence (A, B, C, and D), only strains A, B, and C are capable of infecting humans, and only A and B cause pandemics. In other words, if you catch the flu during flu season, you’re most likely sick with flu type A or B.
Flu vaccines contain inactivated—or dead—influenza virus. These inactivated viruses can’t cause sickness in humans, but when administered as part of a vaccine, they teach a person’s immune system to recognize and kill those viruses when they’re encountered in the wild.
Each spring, a panel of experts gives a recommendation to the US Food and Drug Administration on which strains of each flu type to include in that year’s flu vaccine, depending on what surveillance data says is circulating and what they believe is likely to cause the most illness during the upcoming flu season. For the past decade, Americans have had access to vaccines that provide protection against two strains of influenza A and two lineages of influenza B, known as the Victoria lineage and the Yamagata lineage. But this year, the seasonal flu shot won’t include the Yamagata strain, because the Yamagata strain is no longer circulating among humans.
How Yamagata Disappeared

Flu surveillance data from the Global Initiative on Sharing All Influenza Data (GISAID) shows that the Yamagata lineage of flu type B has not been sequenced since April 2020.
Nature
Experts believe that the Yamagata lineage had already been in decline before the pandemic hit, likely because the strain was naturally less capable of infecting large numbers of people compared to the other strains. When the COVID-19 pandemic hit, the resulting safety precautions such as social distancing, isolating, hand-washing, and masking were enough to drive the virus into extinction completely.
Because the strain hasn’t been circulating since 2020, the FDA elected to remove the Yamagata strain from the seasonal flu vaccine. This will mark the first time since 2012 that the annual flu shot will be trivalent (three-component) rather than quadrivalent (four-component).
Should I still get the flu shot?
The flu shot will protect against fewer strains this year—but that doesn’t mean we should skip it. Influenza places a substantial health burden on the United States every year, responsible for hundreds of thousands of hospitalizations and tens of thousands of deaths. The flu shot has been shown to prevent millions of illnesses each year (more than six million during the 2022-2023 season). And while it’s still possible to catch the flu after getting the flu shot, studies show that people are far less likely to be hospitalized or die when they’re vaccinated.
Another unexpected benefit of dropping the Yamagata strain from the seasonal vaccine? This will possibly make production of the flu vaccine faster, and enable manufacturers to make more vaccines, helping countries who have a flu vaccine shortage and potentially saving millions more lives.
After his grandmother’s dementia diagnosis, one man invented a snack to keep her healthy and hydrated.
Founder Lewis Hornby and his grandmother Pat, sampling Jelly Drops—an edible gummy containing water and life-saving electrolytes.
On a visit to his grandmother’s nursing home in 2016, college student Lewis Hornby made a shocking discovery: Dehydration is a common (and dangerous) problem among seniors—especially those that are diagnosed with dementia.
Hornby’s grandmother, Pat, had always had difficulty keeping up her water intake as she got older, a common issue with seniors. As we age, our body composition changes, and we naturally hold less water than younger adults or children, so it’s easier to become dehydrated quickly if those fluids aren’t replenished. What’s more, our thirst signals diminish naturally as we age as well—meaning our body is not as good as it once was in letting us know that we need to rehydrate. This often creates a perfect storm that commonly leads to dehydration. In Pat’s case, her dehydration was so severe she nearly died.
When Lewis Hornby visited his grandmother at her nursing home afterward, he learned that dehydration especially affects people with dementia, as they often don’t feel thirst cues at all, or may not recognize how to use cups correctly. But while dementia patients often don’t remember to drink water, it seemed to Hornby that they had less problem remembering to eat, particularly candy.

Hornby wanted to create a solution for elderly people who struggled keeping their fluid intake up. He spent the next eighteen months researching and designing a solution and securing funding for his project. In 2019, Hornby won a sizable grant from the Alzheimer’s Society, a UK-based care and research charity for people with dementia and their caregivers. Together, through the charity’s Accelerator Program, they created a bite-sized, sugar-free, edible jelly drop that looked and tasted like candy. The candy, called Jelly Drops, contained 95% water and electrolytes—important minerals that are often lost during dehydration. The final product launched in 2020—and was an immediate success. The drops were able to provide extra hydration to the elderly, as well as help keep dementia patients safe, since dehydration commonly leads to confusion, hospitalization, and sometimes even death.
Not only did Jelly Drops quickly become a favorite snack among dementia patients in the UK, but they were able to provide an additional boost of hydration to hospital workers during the pandemic. In NHS coronavirus hospital wards, patients infected with the virus were regularly given Jelly Drops to keep their fluid levels normal—and staff members snacked on them as well, since long shifts and personal protective equipment (PPE) they were required to wear often left them feeling parched.
In April 2022, Jelly Drops launched in the United States. The company continues to donate 1% of its profits to help fund Alzheimer’s research.

