How sharing, hearing, and remembering positive stories can help shape our brains for the better

Across cultures and through millennia, human beings have always told stories. Whether it’s a group of boy scouts around a campfire sharing ghost stories or the paleolithic Cro-Magnons etching pictures of bison on cave walls, researchers believe that storytelling has been universal to human beings since the development of language.
But storytelling was more than just a way for our ancestors to pass the time. Researchers believe that storytelling served an important evolutionary purpose, helping humans learn empathy, share important information (such as where predators were or what berries were safe to eat), as well as strengthen social bonds. Quite literally, storytelling has made it possible for the human race to survive.
Today, neuroscientists are discovering that storytelling is just as important now as it was millions of years ago. Particularly in sharing positive stories, humans can more easily form relational bonds, develop a more flexible perspective, and actually grow new brain circuitry that helps us survive. Here’s how.
How sharing stories positively impacts the brain
When human beings share stories, it increases the levels of certain neurochemicals in the brain, neuroscientists have found. In a 2021 study published in Proceedings of the National Academy of Sciences (PNAS), Swedish researchers found that simply hearing a story could make hospitalized children feel better, compared to other hospitalized children who played a riddle game for the same amount of time. In their research, children in the intensive care unit who heard stories for just 30 minutes had higher levels of oxytocin, a hormone that promotes positive feelings and is linked to relaxation, trust, social connectedness, and overall psychological stability. Furthermore, the same children showed lower levels of cortisol, a hormone associated with stress. Afterward, the group of children who heard stories tended to describe their hospital experiences more positively, and even reported lower levels of pain.
Annie Brewster, MD, knows the positive effect of storytelling from personal experience. An assistant professor at Harvard Medical School and the author of The Healing Power of Storytelling: Using Personal Narrative to Navigate Illness, Trauma, and Loss, Brewster started sharing her personal experience with chronic illness after being diagnosed with multiple sclerosis in 2001. In doing so, Brewster says it has enabled her to accept her diagnosis and integrate it into her identity. Brewster believes so much in the power of hearing and sharing stories that in 2013 she founded Health Story Collaborative, a forum for others to share their mental and physical health challenges.“I wanted to hear stories of people who had found ways to move forward in positive ways, in spite of health challenges,” Brewster said. In doing so, Brewster believes people with chronic conditions can “move closer to self-acceptance and self-love.”
While hearing and sharing positive stories has been shown to increase oxytocin and other “feel good” chemicals, simply remembering a positive story has an effect on our brains as well. Mark Hoelterhoff, PhD, a lecturer in clinical psychology at the University of Edinburgh, recalling and “savoring” a positive story, thought, or feedback “begins to create new brain circuitry—a new neural network that’s geared toward looking for the positive,” he says. Over time, other research shows, savoring positive stories or thoughts can literally change the shape of your brain, hard-wiring someone to see things in a more positive light.How stories can change your behavior
In 2009, Paul Zak, PhD, a neuroscientist and professor at Claremont Graduate University, set out to measure how storytelling can actually change human behavior for the better. In his study, Zak wanted to measure the behavioral effects of oxytocin, and did this by showing test subjects two short video clips designed to elicit an emotional response.
In the first video they showed the study participants, a father spoke to the camera about his two-year-old son, Ben, who had been diagnosed with terminal brain cancer. The father told the audience that he struggled to connect with and enjoy Ben, as Ben had only a few months left to live. In the end, the father finds the strength to stay emotionally connected to his son until he dies.
The second video clip, however, was much less emotional. In that clip, the same father and son are shown spending the day at the zoo. Ben is only suggested to have cancer (he is bald from chemotherapy and referred to as a ‘miracle’, but the cancer isn’t mentioned directly). The second story lacked the dramatic narrative arc of the first video.
Zak’s team took blood before and after the participants watched one of the two videos and found that the first story increased the viewers’ cortisol and oxytocin, suggesting that they felt distress over the boy’s diagnosis and empathy toward the boy and his father. The second narrative, however, didn’t increase oxytocin or cortisol at all.
But Zak took the experiment a step further. After the movie clips, his team gave the study participants a chance to share money with a stranger in the lab. The participants who had an increase in cortisol and oxytocin were more likely to donate money generously. The participants who had increased cortisol and oxytocin were also more likely to donate money to a charity that works with children who are ill. Zak also found that the amount of oxytocin that was released was correlated with how much money people felt comfortable giving—in other words, the more oxytocin that was released, the more generous they felt, and the more money they donated.
How storytelling strengthens our bond with others
Sharing, hearing, and remembering stories can be a powerful tool for social change–not only in the way it changes our brain and our behavior, but also because it can positively affect our relationships with other people
Emotional stimulation from telling stories, writes Zak, is the foundation for empathy, and empathy strengthens our relationships with other people. “By knowing someone’s story—where they come from, what they do, and who you might know in common—relationships with strangers are formed.”
But why are these relationships important for humanity? Because human beings can use storytelling to build empathy and form relationships, it enables them to “engage in the kinds of large-scale cooperation that builds massive bridges and sends humans into space,” says Zak.
Storytelling, Zak found, and the oxytocin release that follows, also makes people more sensitive to social cues. This sensitivity not only motivates us to form relationships, but also to engage with other people and offer help, particularly if the other person seems to need help.
But as Zak found in his experiments, the type of storytelling matters when it comes to affecting relationships. Where Zak found that storytelling with a dramatic arc helps release oxytocin and cortisol, enabling people to feel more empathic and generous, other researchers have found that sharing happy stories allows for greater closeness between individuals and speakers. A group of Chinese researchers found that, compared to emotionally-neutral stories, happy stories were more “emotionally contagious.” Test subjects who heard happy stories had greater activation in certain areas of their brains, experienced more significant, positive changes in their mood, and felt a greater sense of closeness between themselves and the speaker.
“This finding suggests that when individuals are happy, they become less self-focused and then feel more intimate with others,” the authors of the study wrote. “Therefore, sharing happiness could strengthen interpersonal bonding.” The researchers went on to say that this could lead to developing better social networks, receiving more social support, and leading more successful social lives.
Since the start of the COVID pandemic, social isolation, loneliness, and resulting mental health issues have only gotten worse. In light of this, it’s safe to say that hearing, sharing, and remembering stories isn’t just something we can do for entertainment. Storytelling has always been central to the human experience, and now more than ever it’s become something crucial for our survival.
Want to know how you can reap the benefits of hearing happy stories? Keep an eye out for Upworthy’s first book, GOOD PEOPLE: Stories from the Best of Humanity, published by National Geographic/Disney, available on September 3, 2024. GOOD PEOPLE is a much-needed trove of life-affirming stories told straight from the heart. Handpicked from Upworthy’s community, these 101 stories speak to the breadth, depth, and beauty of the human experience, reminding us we have a lot more in common than we realize.
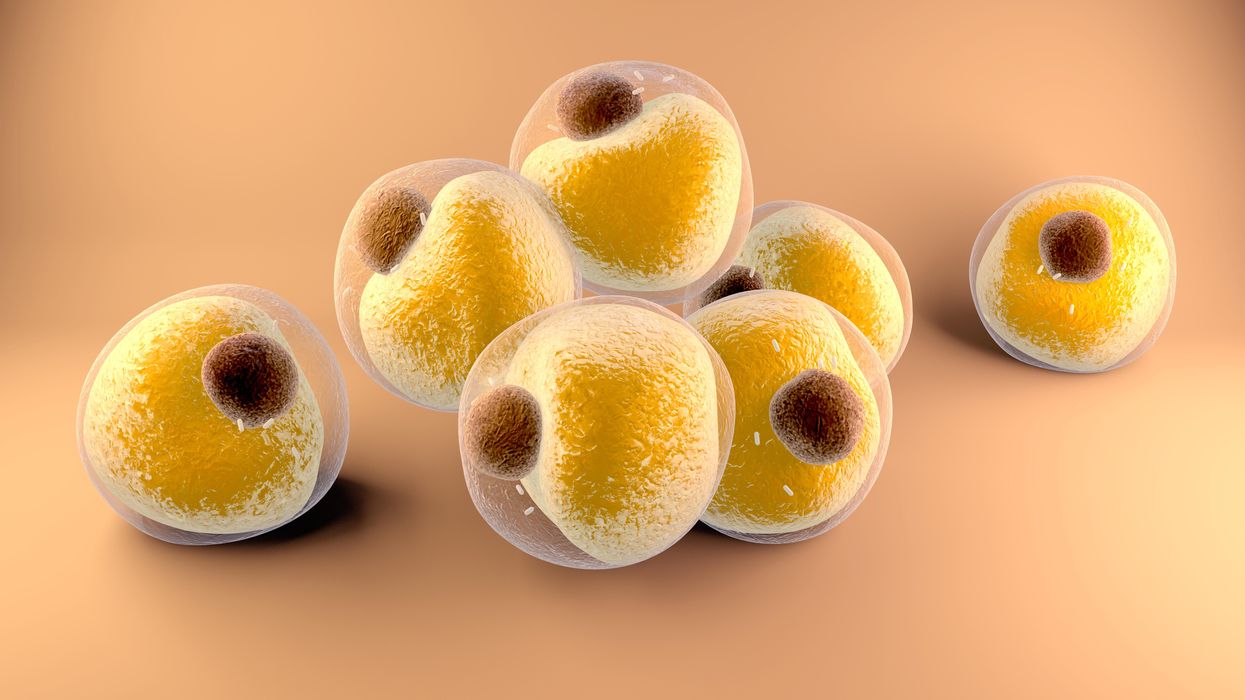
Researchers at Stanford have found that the virus that causes Covid-19 can infect fat cells, which could help explain why obesity is linked to worse outcomes for those who catch Covid-19.
Obesity is a risk factor for worse outcomes for a variety of medical conditions ranging from cancer to Covid-19. Most experts attribute it simply to underlying low-grade inflammation and added weight that make breathing more difficult.
Now researchers have found a more direct reason: SARS-CoV-2, the virus that causes Covid-19, can infect adipocytes, more commonly known as fat cells, and macrophages, immune cells that are part of the broader matrix of cells that support fat tissue. Stanford University researchers Catherine Blish and Tracey McLaughlin are senior authors of the study.
Most of us think of fat as the spare tire that can accumulate around the middle as we age, but fat also is present closer to most internal organs. McLaughlin's research has focused on epicardial fat, “which sits right on top of the heart with no physical barrier at all,” she says. So if that fat got infected and inflamed, it might directly affect the heart.” That could help explain cardiovascular problems associated with Covid-19 infections.
Looking at tissue taken from autopsy, there was evidence of SARS-CoV-2 virus inside the fat cells as well as surrounding inflammation. In fat cells and immune cells harvested from health humans, infection in the laboratory drove "an inflammatory response, particularly in the macrophages…They secreted proteins that are typically seen in a cytokine storm” where the immune response runs amok with potential life-threatening consequences. This suggests to McLaughlin “that there could be a regional and even a systemic inflammatory response following infection in fat.”
It is easy to see how the airborne SARS-CoV-2 virus infects the nose and lungs, but how does it get into fat tissue? That is a mystery and the source of ample speculation.
The macrophages studied by McLaughlin and Blish were spewing out inflammatory proteins, While the the virus within them was replicating, the new viral particles were not able to replicate within those cells. It was a different story in the fat cells. “When [the virus] gets into the fat cells, it not only replicates, it's a productive infection, which means the resulting viral particles can infect another cell,” including microphages, McLaughlin explains. It seems to be a symbiotic tango of the virus between the two cell types that keeps the cycle going.
It is easy to see how the airborne SARS-CoV-2 virus infects the nose and lungs, but how does it get into fat tissue? That is a mystery and the source of ample speculation.
Macrophages are mobile; they engulf and carry invading pathogens to lymphoid tissue in the lymph nodes, tonsils and elsewhere in the body to alert T cells of the immune system to the pathogen. Perhaps some of them also carry the virus through the bloodstream to more distant tissue.
ACE2 receptors are the means by which SARS-CoV-2 latches on to and enters most cells. They are not thought to be common on fat cells, so initially most researchers thought it unlikely they would become infected.
However, while some cell receptors always sit on the surface of the cell, other receptors are expressed on the surface only under certain conditions. Philipp Scherer, a professor of internal medicine and director of the Touchstone Diabetes Center at the University of Texas Southwestern Medical Center, suggests that, in people who have obesity, “There might be higher levels of dysfunctional [fat cells] that facilitate entry of the virus,” either through transiently expressed ACE2 or other receptors. Inflammatory proteins generated by macrophages might contribute to this process.
Another hypothesis is that viral RNA might be smuggled into fat cells as cargo in small bits of material called extracellular vesicles, or EVs, that can travel between cells. Other researchers have shown that when EVs express ACE2 receptors, they can act as decoys for SARS-CoV-2, where the virus binds to them rather than a cell. These scientists are working to create drugs that mimic this decoy effect as an approach to therapy.
Do fat cells play a role in Long Covid? “Fat cells are a great place to hide. You have all the energy you need and fat cells turn over very slowly; they have a half-life of ten years,” says Scherer. Observational studies suggest that acute Covid-19 can trigger the onset of diabetes especially in people who are overweight, and that patients taking medicines to regulate their diabetes “were actually quite protective” against acute Covid-19. Scherer has funding to study the risks and benefits of those drugs in animal models of Long Covid.
McLaughlin says there are two areas of potential concern with fat tissue and Long Covid. One is that this tissue might serve as a “big reservoir where the virus continues to replicate and is sent out” to other parts of the body. The second is that inflammation due to infected fat cells and macrophages can result in fibrosis or scar tissue forming around organs, inhibiting their function. Once scar tissue forms, the tissue damage becomes more difficult to repair.
Current Covid-19 treatments work by stopping the virus from entering cells through the ACE2 receptor, so they likely would have no effect on virus that uses a different mechanism. That means another approach will have to be developed to complement the treatments we already have. So the best advice McLaughlin can offer today is to keep current on vaccinations and boosters and lose weight to reduce the risk associated with obesity.
Air pollution can lead to lung cancer. The connection suggests new ways to stop cancer in its tracks.
Researchers at Francis Crick Institute found that air pollution can "wake up" existing mutations, triggering them to turn into lung cancer. The scientists used their new understanding about this connection to prevent cancer in mice.
Forget taking a deep breath. Around the world, 99 percent of people breathe air polluted to unsafe levels, according to data from the World Health Organization. Activities such as burning fossil fuels release greenhouse gases that contribute to air pollution, which could lead to heart disease, stroke, asthma, emphysema, and some types of cancer.
“The burden of disease attributable to air pollution is now estimated to be on a par with other major global health risks such as unhealthy diet and tobacco smoking, and air pollution is now recognized as the single biggest environmental threat to human health,” wrote the authors of a 2021 WHO report.
The majority of lung cancer is attributed to smoking. But as pollution levels have increased, and anti-smoking campaigns have discouraged smoking, the proportion of lung cancers diagnosed in non-smokers has grown. The CDC estimates that 10 to 20 percent of lung cancers in the U.S. currently occur in non-smokers.
The mechanism between air pollution and the development of lung cancer has been unclear, but researchers at London’s Francis Crick Institute recently made an important breakthrough in understanding the connection. Lead investigator Charles Swanton presented this research last month at a conference in Paris.
Pollution awakens mutations
The Crick Institute scientists were able to identify a new link between common air pollutants and non-small cell lung cancer (NSCLC). They focused on pollutants called particulate matter, or PM, that are 2.5 microns wide, narrower than human cells.
Most cancer diagnosed in non-smoking people is NSCLC, but this type of cancer hasn’t received the same research attention as more common lung cancers found in smokers, according to Clare Weeden, a cancer researcher at the Crick Institute and a co-author of the study.
“This is a really underserved and under-researched population that we really need to tackle, as well as lung cancers that occur in smokers,” she says. “Lung cancer is the number one cancer killer worldwide.”
In the past, some researchers believed air pollution caused mutations that led to cancer. Others believed these mutations could remain dormant without any detriment to health until pollutants or other stressors triggered them to become cancerous. Reviving the latter hypothesis that carcinogens may activate pre-existing mutations, instead of directly causing them, the Crick researchers analyzed samples from 463,679 people in the UK and parts of Asia, noting mutations and comparing changes in gene expression in mice and human cells.
“The mutation can exist in a nascent clone without causing cancer,” says Emilia Lim, a bioinformatics expert and a co-first author of the Crick study. “It is the carcinogen that promotes a conducive environment for this one little clone to grow and expand into cancer. Through our work, we were able to revive excitement for this hypothesis and bring it to light.”
The study explains a confusing pattern of lung cancer developing, particularly in women, despite a lack of environmental risk factors like smoking, secondhand smoke, or radon exposure. The culprit in these cases may have been too much PM 2.5 exposure.
Other researchers had previously identified a link between mutations in certain genes that control epidermal growth factor receptors, or EGFR mutations, and the development of NSCLC. In a 2019 study of 250 people with this type of cancer, about 32 percent had the mutation. Women are more likely to have EGFR mutations than men.
Not everyone who has the EGFR mutation will develop lung cancer. Respirologist Stephen Lam studies lung cancer at the BC Cancer Research Centre in Vancouver, Canada, but was not involved in the Crick Institute research. He says the study explains a confusing pattern of lung cancer developing, particularly in women, despite a lack of environmental risk factors like smoking, secondhand smoke, or radon exposure. The culprit in these cases may have been too much PM 2.5 exposure.
More exposure leads to inflammation and lesions
The Crick researchers found that an excess of PM 2.5 in the air sparked an inflammatory process in cells within the lung. This inflammation set the stage for NSCLC to develop in people and mice with existing EGFR mutations.
The researchers also exposed mice without EGFR mutations to PM 2.5 pollution—an experiment that couldn’t be ethically conducted in humans—to link pollution exposure to NSCLC. The mice experiments also showed that NSCLC is dose-dependent; higher levels of exposure were associated with higher number of cancerous lesions forming.
Ultimately, the study “fundamentally changed how we view lung cancer in people who have never smoked,” said Swanton in a Crick Institute press release. “Cells with cancer-causing mutations accumulate naturally as we age, but they are normally inactive. We’ve demonstrated that air pollution wakes these cells up in the lungs, encouraging them to grow and potentially form tumors.”
Preventing cancer before it begins
Targeted therapies already exist for people with EGFR mutations who’ve developed NSCLC, but they have many side effects, according to Weeden. Researchers hope that making more definitive links between pollutants and cancer could help prevent people with EGFR or other mutations from developing lung cancer in the first place.
Along those lines, as an additional component of their study presented last month, the Crick researchers were able to prevent cancer in mice that had the EGFR mutations by blocking inflammation. They used an antibody to inhibit a protein called interleukin 1 beta, which plays a key role in inflammation. Scientists could eventually use such antibodies or other therapies to make a drug treatment that people can take to stop cancer in its tracks, even if they live in highly polluted areas.
Such potential could reach beyond lung cancer; in the past, Crick and other researchers have also found associations between exposure to air pollution and mesothelioma, as well as cancers of the small intestine, lip, mouth, and throat. These links could be meaningful to a growing number of people as climate change intensifies, and with increases in air pollution from fossil fuel combustion and natural disasters like forest fires.
Plus, air pollution is just one external condition that can flip the switch of these inflammatory pathways. Identifying a link between pollution and cancer “has wide ramifications for many other environmental factors that may [play] similar roles,” Weedon says. She hopes that the Crick study and future research in this area will offer some hope for non-smokers frustrated by cancer diagnoses.