How Smallpox Was Wiped Off the Planet By a Vaccine and Global Cooperation
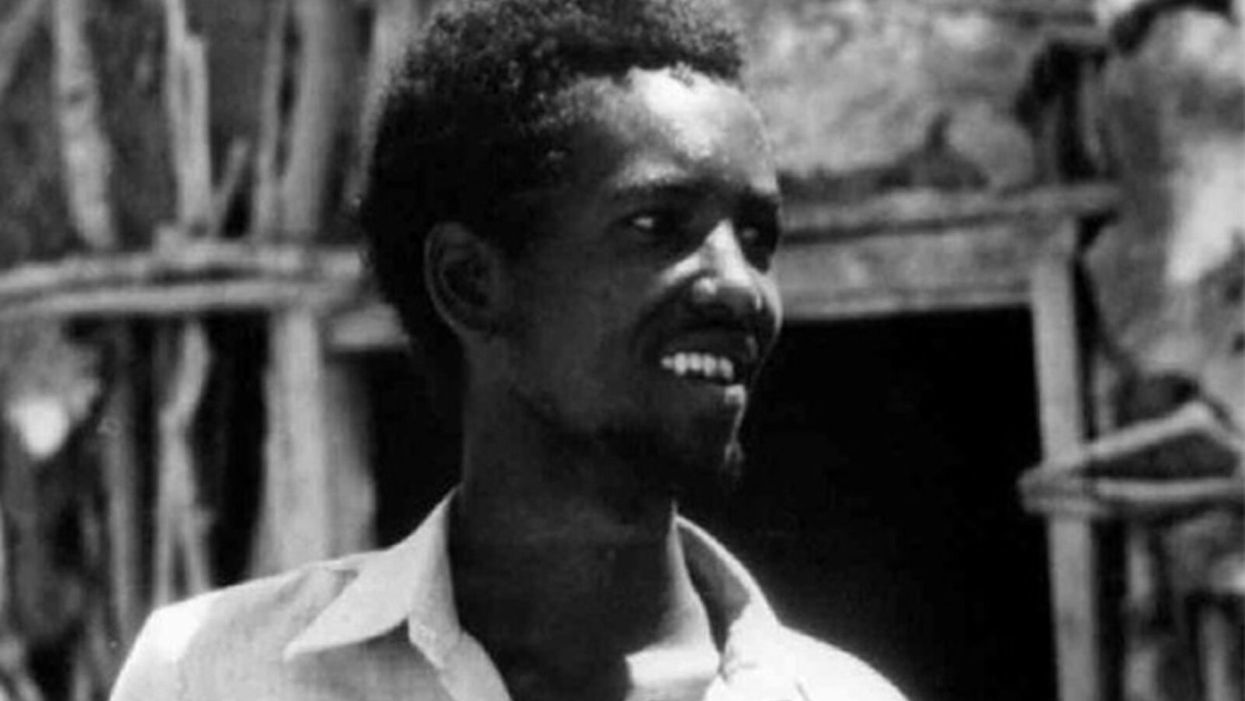
The world's last recorded case of endemic smallpox was in Ali Maow Maalin, of Merka, Somalia, in October 1977. He made a full recovery.
For 3000 years, civilizations all over the world were brutalized by smallpox, an infectious and deadly virus characterized by fever and a rash of painful, oozing sores.
Doctors had to contend with wars, floods, and language barriers to make their campaign a success.
Smallpox was merciless, killing one third of people it infected and leaving many survivors permanently pockmarked and blind. Although smallpox was more common during the 18th and 19th centuries, it was still a leading cause of death even up until the early 1950s, killing an estimated 50 million people annually.
A Primitive Cure
Sometime during the 10th century, Chinese physicians figured out that exposing people to a tiny bit of smallpox would sometimes result in a milder infection and immunity to the disease afterward (if the person survived). Desperate for a cure, people would huff powders made of smallpox scabs or insert smallpox pus into their skin, all in the hopes of getting immunity without having to get too sick. However, this method – called inoculation – didn't always work. People could still catch the full-blown disease, spread it to others, or even catch another infectious disease like syphilis in the process.
A Breakthrough Treatment
For centuries, inoculation – however imperfect – was the only protection the world had against smallpox. But in the late 18th century, an English physician named Edward Jenner created a more effective method. Jenner discovered that inoculating a person with cowpox – a much milder relative of the smallpox virus – would make that person immune to smallpox as well, but this time without the possibility of actually catching or transmitting smallpox. His breakthrough became the world's first vaccine against a contagious disease. Other researchers, like Louis Pasteur, would use these same principles to make vaccines for global killers like anthrax and rabies. Vaccination was considered a miracle, conferring all of the rewards of having gotten sick (immunity) without the risk of death or blindness.
Scaling the Cure
As vaccination became more widespread, the number of global smallpox deaths began to drop, particularly in Europe and the United States. But even as late as 1967, smallpox was still killing anywhere from 10 to 15 million people in poorer parts of the globe. The World Health Assembly (a decision-making body of the World Health Organization) decided that year to launch the first coordinated effort to eradicate smallpox from the planet completely, aiming for 80 percent vaccine coverage in every country in which the disease was endemic – a total of 33 countries.
But officials knew that eradicating smallpox would be easier said than done. Doctors had to contend with wars, floods, and language barriers to make their campaign a success. The vaccination initiative in Bangladesh proved the most challenging, due to its population density and the prevalence of the disease, writes journalist Laurie Garrett in her book, The Coming Plague.
In one instance, French physician Daniel Tarantola on assignment in Bangladesh confronted a murderous gang that was thought to be spreading smallpox throughout the countryside during their crime sprees. Without police protection, Tarantola confronted the gang and "faced down guns" in order to immunize them, protecting the villagers from repeated outbreaks.
Because not enough vaccines existed to vaccinate everyone in a given country, doctors utilized a strategy called "ring vaccination," which meant locating individual outbreaks and vaccinating all known and possible contacts to stop an outbreak at its source. Fewer than 50 percent of the population in Nigeria received a vaccine, for example, but thanks to ring vaccination, it was eradicated in that country nonetheless. Doctors worked tirelessly for the next eleven years to immunize as many people as possible.
The World Health Organization declared smallpox officially eradicated on May 8, 1980.
A Resounding Success
In November 1975, officials discovered a case of variola major — the more virulent strain of the smallpox virus — in a three-year-old Bangladeshi girl named Rahima Banu. Banu was forcibly quarantined in her family's home with armed guards until the risk of transmission had passed, while officials went door-to-door vaccinating everyone within a five-mile radius. Two years later, the last case of variola major in human history was reported in Somalia. When no new community-acquired cases appeared after that, the World Health Organization declared smallpox officially eradicated on May 8, 1980.
Because of smallpox, we now know it's possible to completely eliminate a disease. But is it likely to happen again with other diseases, like COVID-19? Some scientists aren't so sure. As dangerous as smallpox was, it had a few characteristics that made eradication possibly easier than for other diseases. Smallpox, for instance, has no animal reservoir, meaning that it could not circulate in animals and resurge in a human population at a later date. Additionally, a person who had smallpox once was guaranteed immunity from the disease thereafter — which is not the case for COVID-19.
In The Coming Plague, Japanese physician Isao Arita, who led the WHO's Smallpox Eradication Unit, admitted to routinely defying orders from the WHO, mobilizing to parts of the world without official approval and sometimes even vaccinating people against their will. "If we hadn't broken every single WHO rule many times over, we would have never defeated smallpox," Arita said. "Never."
Still, thanks to the life-saving technology of vaccines – and the tireless efforts of doctors and scientists across the globe – a once-lethal disease is now a thing of the past.
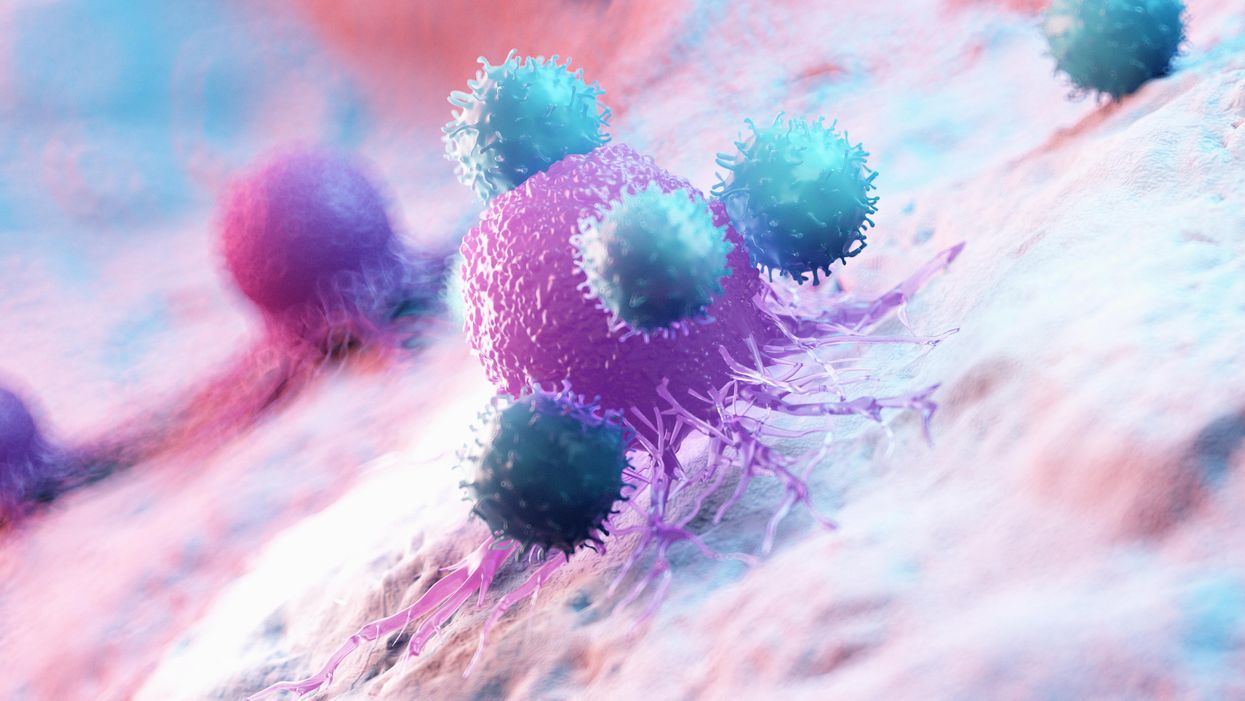
The Friday Five: Artificial DNA Could Give Cancer the Hook
In this week's Friday Five, artificial DNA could give cancer the hook. Plus, research suggests that this daily practice can improve relationships, social media could be good for finding factual information, injecting a gel may speed up recovery from injuries, and a blood pressure medicine is promising for a long healthy life.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Here are the promising studies covered in this week's Friday Five:
- Artificial DNA gives cancer the hook
- This daily practice could improve relationships
- Can social media handle the truth?
- Injecting a gel could speed up recovery
- A blood pressure medicine for a long healthy life
9 Tips for Online Mental Health Therapy
Research shows that, for most patients, online therapy offers the same benefits as in-person therapy, yet many people still resist it. A behavioral scientist explains how you can use it to improve mental health.
Telehealth offers a vast improvement in access and convenience to all sorts of medical services, and online therapy for mental health is one of the most promising case studies for telehealth. With many online therapy options available, you can choose whatever works best for you. Yet many people are hesitant about using online therapy. Even if they do give it a try, they often don’t know how to make the most effective use of this treatment modality.
Why do so many feel uncertain about online therapy? A major reason stems from its novelty. Humans are creatures of habit, prone to falling for what behavioral scientists like myself call the status quo bias, a predisposition to stick to traditional practices and behaviors. Many people reject innovative solutions even when they would be helpful. Thus, while teletherapy was available long before the pandemic, and might have fit the needs of many potential clients, relatively few took advantage of this option.
Even when we do try new methodologies, we often don’t do so effectively, because we cling to the same approaches that worked in previous situations. Scientists call this behavior functional fixedness. It’s kind of like the saying about the hammer-nail syndrome: “when you have a hammer, everything looks like a nail.”
These two mental blindspots, the status quo bias and functional fixedness, impact decision making in many areas of life. Fortunately, recent research has shown effective and pragmatic strategies to defeat these dangerous errors in judgment. The nine tips below will help you make the best decisions to get effective online therapy, based on the latest research.
Trust the science of online therapy
Extensive research shows that, for most patients, online therapy offers the same benefits as in-person therapy.
For instance, a 2014 study in the Journal of Affective Disorders reported that online treatment proved just as effective as face-to-face treatment for depression. A 2018 study, published in Journal of Psychological Disorders, found that online cognitive behavioral therapy, or CBT, was just as effective as face-to-face treatment for major depression, panic disorder, social anxiety disorder, and generalized anxiety disorder. And a 2014 study in Behaviour Research and Therapy discovered that online CBT proved effective in treating anxiety disorders, and helped lower costs of treatment.
During the forced teletherapy of COVID, therapists worried that those with serious mental health conditions would be less likely to convert to teletherapy. Yet research published in Counselling Psychology Quarterly has helped to alleviate that concern. It found that those with schizophrenia, bipolar disorder, severe depression, PTSD, and even suicidality converted to teletherapy at about the same rate as those with less severe mental health challenges.
Yet teletherapy may not be for everyone. For example, adolescents had the most varied response to teletherapy, according to a 2020 study in Family Process. Some adapted quickly and easily, while others found it awkward and anxiety-inducing. On the whole, children with trauma respond worse to online therapy, per a 2020 study in Child Abuse & Neglect. The treatment of mental health issues can sometimes require in-person interactions, such as the use of eye movement desensitization and reprocessing to treat post-traumatic stress disorder. And according to a 2020 study from the Journal of Humanistic Psychology, online therapy may not be as effective for those suffering from loneliness.
Leverage the strengths of online therapy
Online therapy is much more accessible than in-person therapy for those with a decent internet connection, webcam, mic, and digital skills. You don’t have to commute to your therapist’s office, wasting money and time. You can take much less medical leave from work, saving you money and hassle with your boss. If you live in a sparsely populated area, online therapy could allow you to access many specialized kinds of therapy that isn’t accessible locally.
Online options are much quicker compared to the long waiting lines for in-person therapy. You also have much more convenient scheduling options. And you won’t have to worry about running into someone you know in the waiting room. Online therapy is easier to conceal from others and reduces stigma. Many patients may feel more comfortable and open to sharing in the privacy and comfort of their own home.
You can use a variety of communication tools suited to your needs at any given time. Video can be used to start a relationship with a therapist and have more intense and nuanced discussions, but can be draining, especially for those with social anxiety. Voice-only may work well for less intense discussions. Email offers a useful option for long-form, well-thought-out messages. Texting is useful for quick, real-time questions, answers, and reinforcement.
Plus, online therapy is often cheaper than in-person therapy. In the midst of COVID, many insurance providers have decided to cover online therapy.
Address the weaknesses
One weakness is the requirement for appropriate technology and skills to engage in online therapy. Another is the difficulty of forming a close therapeutic relationship with your therapist. You won’t be able to communicate non-verbals as fully and the therapist will not be able to read you as well, requiring you to be more deliberate in how you express yourself.
Another important issue is that online therapy is subject to less government oversight compared to the in-person approach, which is regulated in each state, providing a baseline of quality control. As a result, you have to do more research on the providers that offer online therapy to make sure they’re reputable, use only licensed therapists, and have a clear and transparent pay structure.
Be intentional about advocating for yourself
Figure out what kind of goals you want to achieve. Consider how, within the context of your goals, you can leverage the benefits of online therapy while addressing the weaknesses. Write down and commit to achieving your goals. Remember, you need to be your own advocate, especially in the less regulated space of online therapy, so focus on being proactive in achieving your goals.
Develop your Hero’s Journey
Because online therapy can occur at various times of day through videos calls, emails and text, it might feel more open-ended and less organized, which can have advantages and disadvantages. One way you can give it more structure is to ground these interactions in the story of your self-improvement. Our minds perceive the world through narratives. Create a story of how you’ll get from where you are to where you want to go, meaning your goals.
A good template to use is the Hero’s Journey. Start the narrative with where you are, and what caused you to seek therapy. Write about the obstacles you will need to overcome, and the kind of help from a therapist that you’ll need in the process. Then, describe the final end state: how will you be better off after this journey, including what you will have learned.
Especially in online therapy, you need to be on top of things. Too many people let the therapist manage the treatment plan. As you pursue your hero’s journey, another way to organize for success is to take notes on your progress, and reevaluate how you’re doing every month with your therapist.
Identify your ideal mentor
Since it’s more difficult to be confident about the quality of service providers in an online setting, you should identify in advance the traits of your desired therapist. Every Hero’s Journey involves a mentor figure who guides the protagonist through this journey. So who’s your ideal mentor? Write out their top 10 characteristics, from most to least important.
For example, you might want someone who is:
- Empathetic
- Caring
- Good listener
- Logical
- Direct
- Questioning
- Non-judgmental
- Organized
- Curious
- Flexible
That’s my list. Depending on what challenge you’re facing and your personality and preferences, you should make your own. Then, when you are matched with a therapist, evaluate how well they fit your ideal list.
Fail fast
When you first match with a therapist, try to fail fast. That means, instead of focusing on getting treatment, focus on figuring out if the therapist is a good match based on the traits you identified above. That will enable you to move on quickly if they’re not, and it’s very much worth it to figure that out early.
Tell them your goals, your story, and your vision of your ideal mentor. Ask them whether they think they are a match, and what kind of a treatment plan they would suggest based on the information you provided. And observe them yourself in your initial interactions, focusing on whether they’re a good match. Often, you’ll find that your initial vision of your ideal mentor is incomplete, and you’ll learn through doing therapy what kind of a therapist is the best fit for you.
Choose a small but meaningful subgoal to work on first
This small subgoal should be sufficient to be meaningful and impactful for improving your mental health, but not a big stretch for you to achieve. This subgoal should be a tool for you to use to evaluate whether the therapist is indeed a good fit for you. It will also help you evaluate whether the treatment plan makes sense, or whether it needs to be revised.
Know when to wrap things up
As you approach the end of your planned work and you see you’re reaching your goals, talk to the therapist about how to wrap up rather than letting things drag on for too long. You don’t want to become dependent on therapy: it’s meant to be a temporary intervention. Some less scrupulous therapists will insist that therapy should never end and we should all stay in therapy forever, and you want to avoid falling for this line. When you reach your goals, end your therapy, unless you discover a serious new reason to continue it. Still, it may be wise to set up occasional check-ins once every three to six months to make sure you’re staying on the right track.