Scientists are making machines, wearable and implantable, to act as kidneys
Recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen soon.
Like all those whose kidneys have failed, Scott Burton’s life revolves around dialysis. For nearly two decades, Burton has been hooked up (or, since 2020, has hooked himself up at home) to a dialysis machine that performs the job his kidneys normally would. The process is arduous, time-consuming, and expensive. Except for a brief window before his body rejected a kidney transplant, Burton has depended on machines to take the place of his kidneys since he was 12-years-old. His whole life, the 39-year-old says, revolves around dialysis.
“Whenever I try to plan anything, I also have to plan my dialysis,” says Burton says, who works as a freelance videographer and editor. “It’s a full-time job in itself.”
Many of those on dialysis are in line for a kidney transplant that would allow them to trade thrice-weekly dialysis and strict dietary limits for a lifetime of immunosuppressants. Burton’s previous transplant means that his body will likely reject another donated kidney unless it matches perfectly—something he’s not counting on. It’s why he’s enthusiastic about the development of artificial kidneys, small wearable or implantable devices that would do the job of a healthy kidney while giving users like Burton more flexibility for traveling, working, and more.
Still, the devices aren’t ready for testing in humans—yet. But recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen soon, according to Jonathan Himmelfarb, a nephrologist at the University of Washington.
“It would liberate people with kidney failure,” Himmelfarb says.
An engineering marvel
Compared to the heart or the brain, the kidney doesn’t get as much respect from the medical profession, but its job is far more complex. “It does hundreds of different things,” says UCLA’s Ira Kurtz.
Kurtz would know. He’s worked as a nephrologist for 37 years, devoting his career to helping those with kidney disease. While his colleagues in cardiology and endocrinology have seen major advances in the development of artificial hearts and insulin pumps, little has changed for patients on hemodialysis. The machines remain bulky and require large volumes of a liquid called dialysate to remove toxins from a patient’s blood, along with gallons of purified water. A kidney transplant is the next best thing to someone’s own, functioning organ, but with over 600,000 Americans on dialysis and only about 100,000 kidney transplants each year, most of those in kidney failure are stuck on dialysis.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. Each of the 45 different cell types in the kidney do something different.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. To build an artificial heart, Kurtz says, you basically need to engineer a pump. An artificial pancreas needs to balance blood sugar levels with insulin secretion. While neither of these tasks is simple, they are fairly straightforward. The kidney, on the other hand, does more than get rid of waste products like urea and other toxins. Each of the 45 different cell types in the kidney do something different, helping to regulate electrolytes like sodium, potassium, and phosphorous; maintaining blood pressure and water balance; guiding the body’s hormonal and inflammatory responses; and aiding in the formation of red blood cells.
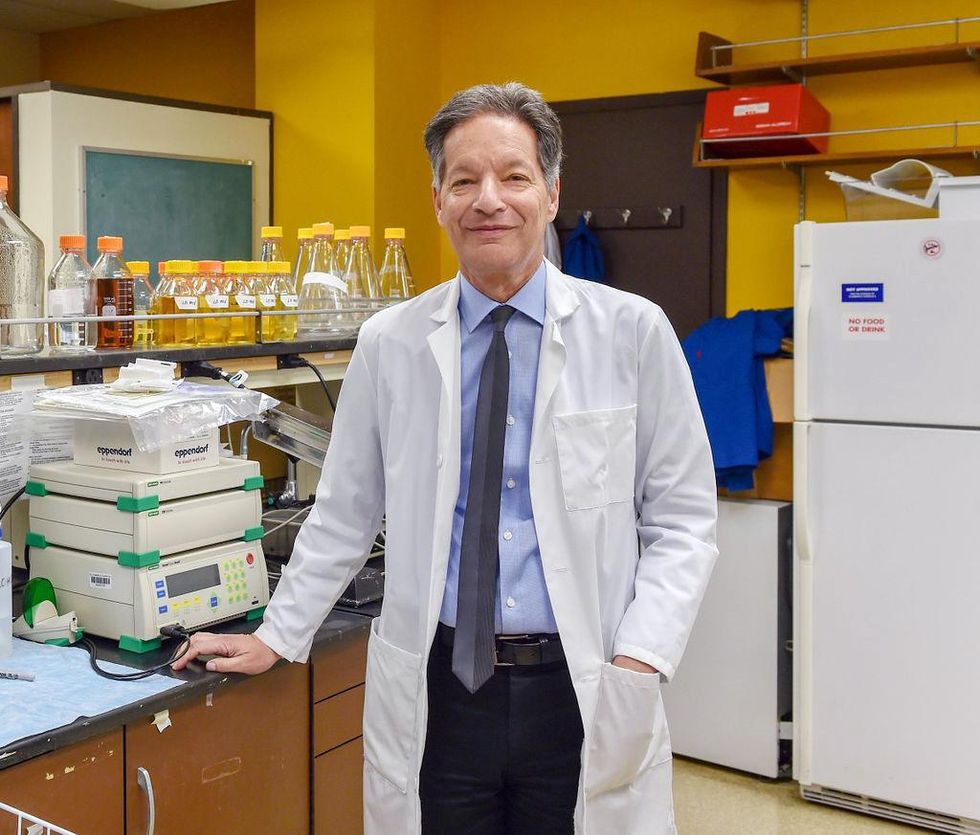
There's been little progress for patients during Ira Kurtz's 37 years as a nephrologist. Artificial kidneys would change that.
UCLA
Dialysis primarily filters waste, and does so well enough to keep someone alive, but it isn’t a true artificial kidney because it doesn’t perform the kidney’s other jobs, according to Kurtz, such as sensing levels of toxins, wastes, and electrolytes in the blood. Due to the size and water requirements of existing dialysis machines, the equipment isn’t portable. Physicians write a prescription for a certain duration of dialysis and assess how well it’s working with semi-regular blood tests. The process of dialysis itself, however, is conducted blind. Doctors can’t tell how much dialysis a patient needs based on kidney values at the time of treatment, says Meera Harhay, a nephrologist at Drexel University in Philadelphia.
But it’s the impact of dialysis on their day-to-day lives that creates the most problems for patients. Only one-quarter of those on dialysis are able to remain employed (compared to 85% of similar-aged adults), and many report a low quality of life. Having more flexibility in life would make a major different to her patients, Harhay says.
“Almost half their week is taken up by the burden of their treatment. It really eats away at their freedom and their ability to do things that add value to their life,” she says.
Art imitates life
The challenge for artificial kidney designers was how to compress the kidney’s natural functions into a portable, wearable, or implantable device that wouldn’t need constant access to gallons of purified and sterilized water. The other universal challenge they faced was ensuring that any part of the artificial kidney that would come in contact with blood was kept germ-free to prevent infection.
As part of the 2021 KidneyX Prize, a partnership between the U.S. Department of Health and Human Services and the American Society of Nephrology, inventors were challenged to create prototypes for artificial kidneys. Himmelfarb’s team at the University of Washington’s Center for Dialysis Innovation won the prize by focusing on miniaturizing existing technologies to create a portable dialysis machine. The backpack sized AKTIV device (Ambulatory Kidney to Increase Vitality) will recycle dialysate in a closed loop system that removes urea from blood and uses light-based chemical reactions to convert the urea to nitrogen and carbon dioxide, which allows the dialysate to be recirculated.
Himmelfarb says that the AKTIV can be used when at home, work, or traveling, which will give users more flexibility and freedom. “If you had a 30-pound device that you could put in the overhead bins when traveling, you could go visit your grandkids,” he says.
Kurtz’s team at UCLA partnered with the U.S. Kidney Research Corporation and Arkansas University to develop a dialysate-free desktop device (about the size of a small printer) as the first phase of a progression that will he hopes will lead to something small and implantable. Part of the reason for the artificial kidney’s size, Kurtz says, is the number of functions his team are cramming into it. Not only will it filter urea from blood, but it will also use electricity to help regulate electrolyte levels in a process called electrodeionization. Kurtz emphasizes that these additional functions are what makes his design a true artificial kidney instead of just a small dialysis machine.
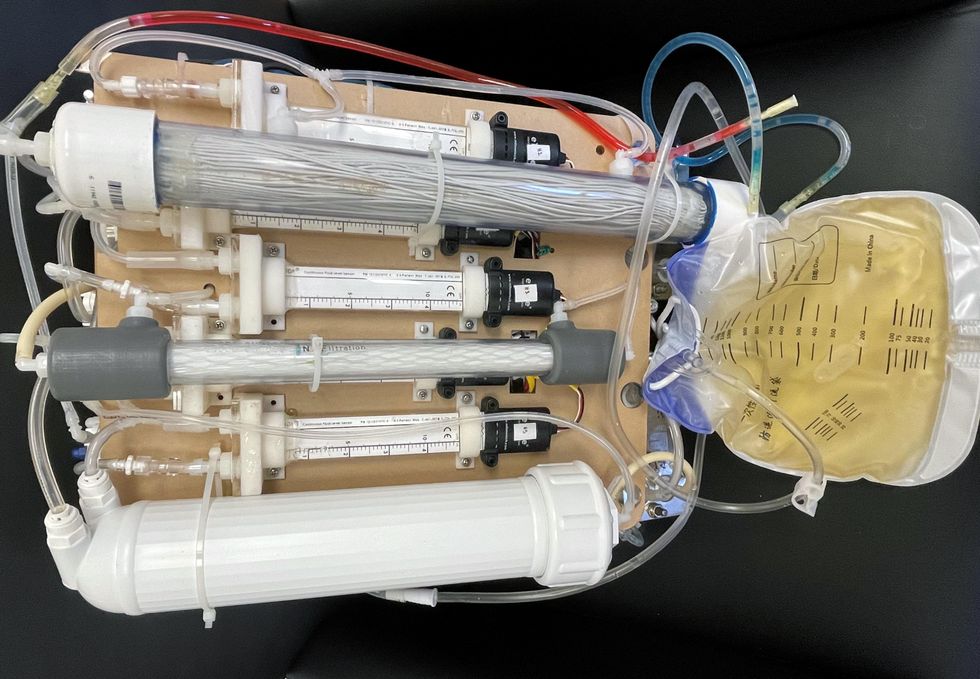
One version of an artificial kidney.
UCLA
“It doesn't have just a static function. It has a bank of sensors that measure chemicals in the blood and feeds that information back to the device,” Kurtz says.
Other startups are getting in on the game. Nephria Bio, a spinout from the South Korean-based EOFlow, is working to develop a wearable dialysis device, akin to an insulin pump, that uses miniature cartridges with nanomaterial filters to clean blood (Harhay is a scientific advisor to Nephria). Ian Welsford, Nephria’s co-founder and CTO, says that the device’s design means that it can also be used to treat acute kidney injuries in resource-limited settings. These potentials have garnered interest and investment in artificial kidneys from the U.S. Department of Defense.
For his part, Burton is most interested in an implantable device, as that would give him the most freedom. Even having a regular outpatient procedure to change batteries or filters would be a minor inconvenience to him.
“Being plugged into a machine, that’s not mimicking life,” he says.
This article was first published by Leaps.org on May 5, 2022.
Podcast: Should Scientific Controversies Be Silenced?
The recent Joe Rogan/Spotify controversy prompts the consideration of tough questions about expertise, trust, gatekeepers, and dissent.
The "Making Sense of Science" podcast features interviews with leading medical and scientific experts about the latest developments and the big ethical and societal questions they raise. This monthly podcast is hosted by journalist Kira Peikoff, founding editor of the award-winning science outlet Leaps.org.
The recent Joe Rogan/Spotify backlash over the misinformation presented in his recent episode on the Covid-19 vaccines raises some difficult and important bioethical questions for society: How can people know which experts to trust? What should big tech gatekeepers do about false claims promoted on their platforms? How should the scientific establishment respond to heterodox viewpoints from experts who disagree with the consensus? When is silencing of dissent merited, and when is it problematic? Journalist Kira Peikoff asks infectious disease physician and pandemic scholar Dr. Amesh Adalja to weigh in.

Dr. Amesh Adalja, Senior Scholar, Johns Hopkins Center for Health Security and an infectious disease physician
Listen to the Episode
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Scientists Are Studying How to Help Dogs Have Longer Lives, in a Bid to Further Our Own
Feeding dogs only once a day is showing health benefits in a large study, scientists report.
The sad eyes. The wagging tail. The frustrated whine. The excited bark. Dogs know how to get their owners to fork over the food more often.
The extra calories dogs get from feeding patterns now used by many Americans may not be good for them from a health and longevity viewpoint. In research from a large study called the Dog Aging Project, canines fed once a day had better scores on cognition tests and lower odds of developing diseases of organs throughout the body: intestinal tract, mouth and teeth, bones and joints, kidneys and bladder, and liver and pancreas.
Fewer than 1 in 10 dog owners fed their furry friends once daily, while nearly three fourths provided two daily meals.
“Most veterinarians have been led to believe that feeding dogs twice a day is optimal, but this is a relatively new idea that has developed over the past few decades with little supportive evidence from a health standpoint,” said Matt Kaeberlein, PhD, Co-Director of the Dog Aging Project, a professor of pathology and Director of the Healthy Aging and Longevity Research Institute at the University of Washington. Kaeberlein studies basic mechanisms of aging to find ways of extending the healthspan, the number of years of life lived free of disease. It’s not enough to extend the lifespan unless declines in biological function and risks of age-related diseases are also studied, he believes, hence the healthspan.
The Dog Aging Project is studying tens of thousands of dogs living with their owners in the real world, not a biology laboratory. The feeding study is the first of several reports now coming from the project based on owners’ annual reports of demographics, physical activity, environment, dog behavior, diet, medications and supplements, and health status. It has been posted on bioRxiv as it goes through peer review.
“All available evidence suggests that most biological mechanisms of aging in dogs will be conserved in humans. It just happens much faster in dogs.”
“The Dog Aging Project is one of the most exciting in the longevity space,” said David A. Sinclair, professor in the Department of Genetics and co-director of the Paul F. Glenn Center for Biology of Aging Research at Harvard Medical School. “Not only is it important to help our companions live longer and healthier, but because they are like people and share the same environment and many of the lifestyles as their owners, they are the perfect model for human longevity interventions.”
The epigenetic clock — and specifically changes in gene expression resulting from methylation of cytosine and guanine in the DNA — provides the critical connection between aging in dogs and people. “All available evidence suggests that most biological mechanisms of aging in dogs will be conserved in humans,” Kaeberlein said. “It just happens much faster in dogs.” These methylation changes, called the “methylomes,” have been associated with rates of aging in dogs, humans, and also mice.
In a 2020 study young dogs matched with young adults and aged dogs matched with older adults showed the greatest similarities in methylomes. In the Cell Systems report, Tina Wang of the University of California, San Diego, and colleagues wrote that the methylome “can be used to quantitatively translate the age-related physiology experienced by one organism (i.e., a model species like dog) to the age at which physiology in a second organism is most similar (i.e., a second model or humans).” This allows rates of aging in one species to be mapped onto aging in another species, providing “a compelling tool in the quest to understand aging and identify interventions for maximizing healthy lifespan.”
In the Dog Aging Project study, 8% of 24,238 owners fed their dogs once daily, the same as the percentage of owners serving three daily meals. Twice-daily feedings were most common (73%), and just over 1 in 10 owners (11%) “free fed” their dogs by just filling up the bowl whenever it was empty — most likely Rover’s favorite option.
“The notion of breakfast, lunch, and dinner for people in the United States is not based on large studies that compared three meals a day to two meals a day, or to four, “ said Kate E. Creevy, chief veterinary officer with the Dog Aging Project and associate professor at Texas A&M University. “It’s more about what we are accustomed to. Similarly, there are not large population studies comparing outcomes of dogs fed once, twice, or three times a day.”
“We do not recommend that people change their dogs’ diets based on this report,” Creevy emphasized. “It’s important to understand the difference between research that finds associations versus research that finds cause and effect.”
To establish cause and effect, the Dog Aging Project will follow their cohort over many years. Then, Creevy said, “We will be able to determine whether the associations we have found with feeding frequency are causes, or effects, or neither.”
While not yet actionable, the feeding findings fit with biology across a variety of animals, Kaeberlein said, including indicators that better health translates into longer healthspans. He said that caloric restriction and perhaps time-restricted eating or intermittent fasting — all ways that some human diets are structured — can have a positive impact on the biology of aging by allowing the gastrointestinal tract to have time each day to rest and repair itself, just as sleep benefits the brain through rest.
Timing of meals is also related to the concept of ketogenesis, Kaeberlein explained. Without access to glucose, animals switch over to a ketogenic state in which back-up systems produce energy through metabolic pathways that generate ketones. Mice go into this state very quickly, after a few hours or an overnight fast, while people shift to ketogenesis more slowly, from a few hours to up to 36 hours for people on typical Western diets, Kaeberlein said.
Dogs are different. They take at least two days to shift to ketogenesis, suggesting they have evolved to need fewer meals that are spaced out rather than the multiple daily meals plus snacks that people prefer.
As this relates to longevity, Kaeberlein said that a couple of studies show that mice who are fed a ketogenic diet have longer lifespans (years of life regardless of health). “For us, the next step is to analyze the composition of the dogs’ diets or the relationship of multiple daily feedings with obesity,” he said. “Maybe not being obese is related to better health.”
To learn more, the Dog Aging Project needs dogs — lots of dogs! Kaeberlein wants at least 100,000 dogs, including small dogs, large dogs, dogs of all ages. Puppies are needed for the researchers to follow across their lifespan. The project has an excellent website where owners can volunteer to participate.
Nutritional strategies are often not built around sound scientific principles, Kaeberlein said. In human nutrition, people have tried all kinds of diets over the years, including some that were completely wrong. Kaeberlein and his colleagues in the Dog Aging Project want to change that, at least for people’s canine companions, and hopefully, as a result, give dogs added years of healthy life and provide clues for human nutrition.
After that, maybe they can do something about those sad eyes and the frustrated whine.

