Scientists are making machines, wearable and implantable, to act as kidneys
Recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen soon.
Like all those whose kidneys have failed, Scott Burton’s life revolves around dialysis. For nearly two decades, Burton has been hooked up (or, since 2020, has hooked himself up at home) to a dialysis machine that performs the job his kidneys normally would. The process is arduous, time-consuming, and expensive. Except for a brief window before his body rejected a kidney transplant, Burton has depended on machines to take the place of his kidneys since he was 12-years-old. His whole life, the 39-year-old says, revolves around dialysis.
“Whenever I try to plan anything, I also have to plan my dialysis,” says Burton says, who works as a freelance videographer and editor. “It’s a full-time job in itself.”
Many of those on dialysis are in line for a kidney transplant that would allow them to trade thrice-weekly dialysis and strict dietary limits for a lifetime of immunosuppressants. Burton’s previous transplant means that his body will likely reject another donated kidney unless it matches perfectly—something he’s not counting on. It’s why he’s enthusiastic about the development of artificial kidneys, small wearable or implantable devices that would do the job of a healthy kidney while giving users like Burton more flexibility for traveling, working, and more.
Still, the devices aren’t ready for testing in humans—yet. But recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen soon, according to Jonathan Himmelfarb, a nephrologist at the University of Washington.
“It would liberate people with kidney failure,” Himmelfarb says.
An engineering marvel
Compared to the heart or the brain, the kidney doesn’t get as much respect from the medical profession, but its job is far more complex. “It does hundreds of different things,” says UCLA’s Ira Kurtz.
Kurtz would know. He’s worked as a nephrologist for 37 years, devoting his career to helping those with kidney disease. While his colleagues in cardiology and endocrinology have seen major advances in the development of artificial hearts and insulin pumps, little has changed for patients on hemodialysis. The machines remain bulky and require large volumes of a liquid called dialysate to remove toxins from a patient’s blood, along with gallons of purified water. A kidney transplant is the next best thing to someone’s own, functioning organ, but with over 600,000 Americans on dialysis and only about 100,000 kidney transplants each year, most of those in kidney failure are stuck on dialysis.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. Each of the 45 different cell types in the kidney do something different.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. To build an artificial heart, Kurtz says, you basically need to engineer a pump. An artificial pancreas needs to balance blood sugar levels with insulin secretion. While neither of these tasks is simple, they are fairly straightforward. The kidney, on the other hand, does more than get rid of waste products like urea and other toxins. Each of the 45 different cell types in the kidney do something different, helping to regulate electrolytes like sodium, potassium, and phosphorous; maintaining blood pressure and water balance; guiding the body’s hormonal and inflammatory responses; and aiding in the formation of red blood cells.
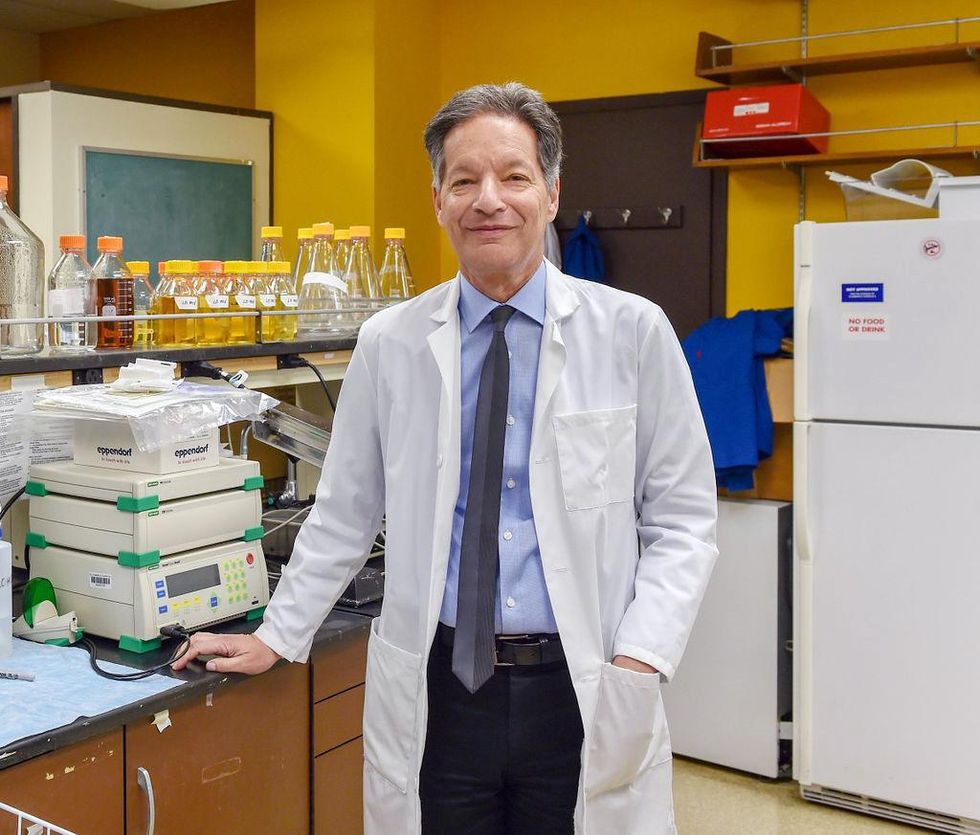
There's been little progress for patients during Ira Kurtz's 37 years as a nephrologist. Artificial kidneys would change that.
UCLA
Dialysis primarily filters waste, and does so well enough to keep someone alive, but it isn’t a true artificial kidney because it doesn’t perform the kidney’s other jobs, according to Kurtz, such as sensing levels of toxins, wastes, and electrolytes in the blood. Due to the size and water requirements of existing dialysis machines, the equipment isn’t portable. Physicians write a prescription for a certain duration of dialysis and assess how well it’s working with semi-regular blood tests. The process of dialysis itself, however, is conducted blind. Doctors can’t tell how much dialysis a patient needs based on kidney values at the time of treatment, says Meera Harhay, a nephrologist at Drexel University in Philadelphia.
But it’s the impact of dialysis on their day-to-day lives that creates the most problems for patients. Only one-quarter of those on dialysis are able to remain employed (compared to 85% of similar-aged adults), and many report a low quality of life. Having more flexibility in life would make a major different to her patients, Harhay says.
“Almost half their week is taken up by the burden of their treatment. It really eats away at their freedom and their ability to do things that add value to their life,” she says.
Art imitates life
The challenge for artificial kidney designers was how to compress the kidney’s natural functions into a portable, wearable, or implantable device that wouldn’t need constant access to gallons of purified and sterilized water. The other universal challenge they faced was ensuring that any part of the artificial kidney that would come in contact with blood was kept germ-free to prevent infection.
As part of the 2021 KidneyX Prize, a partnership between the U.S. Department of Health and Human Services and the American Society of Nephrology, inventors were challenged to create prototypes for artificial kidneys. Himmelfarb’s team at the University of Washington’s Center for Dialysis Innovation won the prize by focusing on miniaturizing existing technologies to create a portable dialysis machine. The backpack sized AKTIV device (Ambulatory Kidney to Increase Vitality) will recycle dialysate in a closed loop system that removes urea from blood and uses light-based chemical reactions to convert the urea to nitrogen and carbon dioxide, which allows the dialysate to be recirculated.
Himmelfarb says that the AKTIV can be used when at home, work, or traveling, which will give users more flexibility and freedom. “If you had a 30-pound device that you could put in the overhead bins when traveling, you could go visit your grandkids,” he says.
Kurtz’s team at UCLA partnered with the U.S. Kidney Research Corporation and Arkansas University to develop a dialysate-free desktop device (about the size of a small printer) as the first phase of a progression that will he hopes will lead to something small and implantable. Part of the reason for the artificial kidney’s size, Kurtz says, is the number of functions his team are cramming into it. Not only will it filter urea from blood, but it will also use electricity to help regulate electrolyte levels in a process called electrodeionization. Kurtz emphasizes that these additional functions are what makes his design a true artificial kidney instead of just a small dialysis machine.
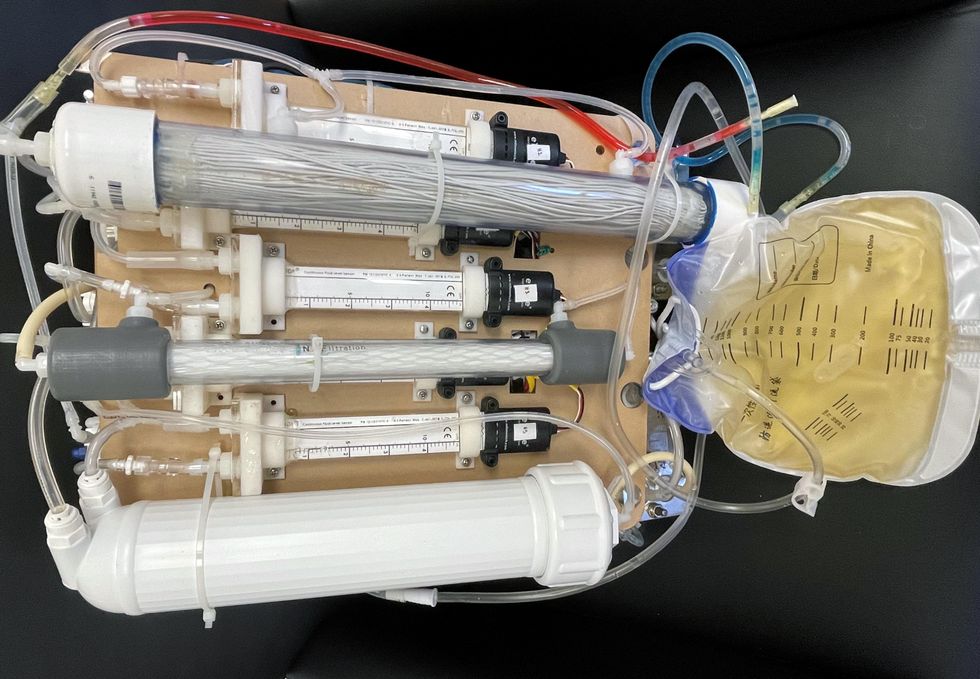
One version of an artificial kidney.
UCLA
“It doesn't have just a static function. It has a bank of sensors that measure chemicals in the blood and feeds that information back to the device,” Kurtz says.
Other startups are getting in on the game. Nephria Bio, a spinout from the South Korean-based EOFlow, is working to develop a wearable dialysis device, akin to an insulin pump, that uses miniature cartridges with nanomaterial filters to clean blood (Harhay is a scientific advisor to Nephria). Ian Welsford, Nephria’s co-founder and CTO, says that the device’s design means that it can also be used to treat acute kidney injuries in resource-limited settings. These potentials have garnered interest and investment in artificial kidneys from the U.S. Department of Defense.
For his part, Burton is most interested in an implantable device, as that would give him the most freedom. Even having a regular outpatient procedure to change batteries or filters would be a minor inconvenience to him.
“Being plugged into a machine, that’s not mimicking life,” he says.
This article was first published by Leaps.org on May 5, 2022.
Study Shows “Living Drug” Can Provide a Lasting Cure for Cancer
A recent study by researchers at the University of Pennsylvania examined how CAR-T therapy helped Doug Olson beat a cancer death sentence for over a decade - and how it could work for more people.
Doug Olson was 49 when he was diagnosed with chronic lymphocytic leukemia, a blood cancer that strikes 21,000 Americans annually. Although the disease kills most patients within a decade, Olson’s case progressed more slowly, and courses of mild chemotherapy kept him healthy for 13 years. Then, when he was 62, the medication stopped working. The cancer had mutated, his doctor explained, becoming resistant to standard remedies. Harsher forms of chemo might buy him a few months, but their side effects would be debilitating. It was time to consider the treatment of last resort: a bone-marrow transplant.
Olson, a scientist who developed blood-testing instruments, knew the odds. There was only a 50 percent chance that a transplant would cure him. There was a 20 percent chance that the agonizing procedure—which involves destroying the patient’s marrow with chemo and radiation, then infusing his blood with donated stem cells—would kill him. If he survived, he would face the danger of graft-versus-host disease, in which the donor’s cells attack the recipient’s tissues. To prevent it, he would have to take immunosuppressant drugs, increasing the risk of infections. He could end up with pneumonia if one of his three grandchildren caught a sniffle. “I was being pushed into a corner,” Olson recalls, “with very little room to move.”
Soon afterward, however, his doctor revealed a possible escape route. He and some colleagues at the University of Pennsylvania’s Abramson Cancer Center were starting a clinical trial, he said, and Olson—still mostly symptom-free—might be a good candidate. The experimental treatment, known as CAR-T therapy, would use genetic engineering to turn his T lymphocytes (immune cells that guard against viruses and other pathogens) into a weapon against cancer.
In September 2010, technicians took some of Olson’s T cells to a laboratory, where they were programmed with new molecular marching orders and coaxed to multiply into an army of millions. When they were ready, a nurse inserted a catheter into his neck. At the turn of a valve, his soldiers returned home, ready to do battle.
“I felt like I’d won the lottery,” Olson says. But he was only the second person in the world to receive this “living drug,” as the University of Pennsylvania investigators called it. No one knew how long his remission would last.
Three weeks later, Olson was slammed with a 102-degree fever, nausea, and chills. The treatment had triggered two dangerous complications: cytokine release syndrome, in which immune chemicals inflame the patient’s tissues, and tumor lysis syndrome, in which toxins from dying cancer cells overwhelm the kidneys. But the crisis passed quickly, and the CAR-T cells fought on. A month after the infusion, the doctor delivered astounding news: “We can’t find any cancer in your body.”
“I felt like I’d won the lottery,” Olson says. But he was only the second person in the world to receive this “living drug,” as the University of Pennsylvania investigators called it. No one knew how long his remission would last.
An Unexpected Cure
In February 2022, the same cancer researchers reported a remarkable milestone: the trial’s first two patients had survived for more than a decade. Although Olson’s predecessor—a retired corrections officer named Bill Ludwig—died of COVID-19 complications in early 2021, both men had remained cancer-free. And the modified immune cells continued to patrol their territory, ready to kill suspected tumor cells the moment they arose.
“We can now conclude that CAR-T cells can actually cure patients with leukemia,” University of Pennsylvania immunologist Carl June, who spearheaded the development of the technique, told reporters. “We thought the cells would be gone in a month or two. The fact that they’ve survived 10 years is a major surprise.”
Even before the announcement, it was clear that CAR-T therapy could win a lasting reprieve for many patients with cancers that were once a death sentence. Since the Food and Drug Administration approved June’s version (marketed as Kymriah) in 2017, the agency has greenlighted five more such treatments for various types of leukemia, lymphoma, and myeloma. “Every single day, I take care of patients who would previously have been told they had no options,” says Rayne Rouce, a pediatric hematologist/oncologist at Texas Children’s Cancer Center. “Now we not only have a treatment option for those patients, but one that could potentially be the last therapy for their cancer that they’ll ever have to receive.”

Immunologist Carl June, middle, spearheaded development of the CAR-T therapy that gave patients Bill Ludwig, left, and Doug Olson, right, a lengthy reprieve on their terminal cancer diagnoses.
Penn Medicine
Yet the CAR-T approach doesn’t help everyone. So far, it has only shown success for blood cancers—and for those, the overall remission rate is 30 to 40 percent. “When it works, it works extraordinarily well,” says Olson’s former doctor, David Porter, director of Penn’s blood and bone marrow transplant program. “It’s important to know why it works, but it’s equally important to know why it doesn’t—and how we can fix that.”
The team’s study, published in the journal Nature, offers a wealth of data on what worked for these two patients. It may also hold clues for how to make the therapy effective for more people.
Building a Better T Cell
Carl June didn’t set out to cure cancer, but his serendipitous career path—and a personal tragedy—helped him achieve insights that had eluded other researchers. In 1971, hoping to avoid combat in Vietnam, he applied to the U.S. Naval Academy in Annapolis, Maryland. June showed a knack for biology, so the Navy sent him on to Baylor College of Medicine. He fell in love with immunology during a fellowship researching malaria vaccines in Switzerland. Later, the Navy deployed him to the Fred Hutchinson Cancer Research Center in Seattle to study bone marrow transplantation.
There, June became part of the first research team to learn how to culture T cells efficiently in a lab. After moving on to the National Naval Medical Center in the ’80s, he used that knowledge to combat the newly emerging AIDS epidemic. HIV, the virus that causes the disease, invades T cells and eventually destroys them. June and his post-doc Bruce Levine developed a method to restore patients’ depleted cell populations, using tiny magnetic beads to deliver growth-stimulating proteins. Infused into the body, the new T cells effectively boosted immune function.
In 1999, after leaving the Navy, June joined the University of Pennsylvania. His wife, who’d been diagnosed with ovarian cancer, died two years later, leaving three young children. “I had not known what it was like to be on the other side of the bed,” he recalls. Watching her suffer through grueling but futile chemotherapy, followed by an unsuccessful bone-marrow transplant, he resolved to focus on finding better cancer treatments. He started with leukemia—a family of diseases in which mutant white blood cells proliferate in the marrow.
Cancer is highly skilled at slipping through the immune system’s defenses. T cells, for example, detect pathogens by latching onto them with receptors designed to recognize foreign proteins. Leukemia cells evade detection, in part, by masquerading as normal white blood cells—that is, as part of the immune system itself.
June planned to use a viral vector no one had tried before: HIV.
To June, chimeric antigen receptor (CAR) T cells looked like a promising tool for unmasking and destroying the impostors. Developed in the early ’90s, these cells could be programmed to identify a target protein, and to kill any pathogen that displayed it. To do the programming, you spliced together snippets of DNA and inserted them into a disabled virus. Next, you removed some of the patient’s T cells and infected them with the virus, which genetically hijacked its new hosts—instructing them to find and slay the patient’s particular type of cancer cells. When the T cells multiplied, their descendants carried the new genetic code. You then infused those modified cells into the patient, where they went to war against their designated enemy.
Or that’s what happened in theory. Many scientists had tried to develop therapies using CAR-T cells, but none had succeeded. Although the technique worked in lab animals, the cells either died out or lost their potency in humans.
But June had the advantage of his years nurturing T cells for AIDS patients, as well as the technology he’d developed with Levine (who’d followed him to Penn with other team members). He also planned to use a viral vector no one had tried before: HIV, which had evolved to thrive in human T cells and could be altered to avoid causing disease. By the summer of 2010, he was ready to test CAR-T therapy against chronic lymphocytic leukemia (CLL), the most common form of the disease in adults.
Three patients signed up for the trial, including Doug Olson and Bill Ludwig. A portion of each man’s T cells were reprogrammed to detect a protein found only on B lymphocytes, the type of white blood cells affected by CLL. Their genetic instructions ordered them to destroy any cell carrying the protein, known as CD19, and to multiply whenever they encountered one. This meant the patients would forfeit all their B cells, not just cancerous ones—but regular injections of gamma globulins (a cocktail of antibodies) would make up for the loss.
After being infused with the CAR-T cells, all three men suffered high fevers and potentially life-threatening inflammation, but all pulled through without lasting damage. The third patient experienced a partial remission and survived for eight months. Olson and Ludwig were cured.
Learning What Works
Since those first infusions, researchers have developed reliable ways to prevent or treat the side effects of CAR-T therapy, greatly reducing its risks. They’ve also been experimenting with combination therapies—pairing CAR-T with chemo, cancer vaccines, and immunotherapy drugs called checkpoint inhibitors—to improve its success rate. But CAR-T cells are still ineffective for at least 60 percent of blood cancer patients. And they remain in the experimental stage for solid tumors (including pancreatic cancer, mesothelioma, and glioblastoma), whose greater complexity make them harder to attack.
The new Nature study offers clues that could fuel further advances. The Penn team “profiled these cells at a level where we can almost say, ‘These are the characteristics that a T cell would need to survive 10 years,’” says Rouce, the physician at Texas Children’s Cancer Center.
One surprising finding involves how CAR-T cells change in the body over time. At first, those that Olson and Ludwig received showed the hallmarks of “killer” T-cells (also known as CD8 cells)—highly active lymphocytes bent on exterminating every tumor cell in sight. After several months, however, the population shifted toward “helper” T-cells (or CD4s), which aid in forming long-term immune memory but are normally incapable of direct aggression. Over the years, the numbers swung back and forth, until only helper cells remained. Those cells showed markers suggesting they were too exhausted to function—but in the lab, they were able not only to recognize but to destroy cancer cells.
June and his team suspect that those tired-looking helper cells had enough oomph to kill off any B cells Olson and Ludwig made, keeping the pair’s cancers permanently at bay. If so, that could prompt new approaches to selecting cells for CAR-T therapy. Maybe starting with a mix of cell types—not only CD8s, but CD4s and other varieties—would work better than using CD8s alone. Or perhaps inducing changes in cell populations at different times would help.
Another potential avenue for improvement is starting with healthier cells. Evidence from this and other trials hints that patients whose T cells are more robust to begin with respond better when their cells are used in CAR-T therapy. The Penn team recently completed a clinical trial in which CLL patients were treated with ibrutinib—a drug that enhances T-cell function—before their CAR-T cells were manufactured. The response rate, says David Porter, was “very high,” with most patients remaining cancer-free a year after being infused with the souped-up cells.
Such approaches, he adds, are essential to achieving the next phase in CAR-T therapy: “Getting it to work not just in more people, but in everybody.”

Doug Olson enjoys nature - and having a future.
Penn Medicine
To grasp what that could mean, it helps to talk with Doug Olson, who’s now 75. In the years since his infusion, he has watched his four children forge careers, and his grandkids reach their teens. He has built a business and enjoyed the rewards of semi-retirement. He’s done volunteer and advocacy work for cancer patients, run half-marathons, sailed the Caribbean, and ridden his bike along the sun-dappled roads of Silicon Valley, his current home.
And in his spare moments, he has just sat there feeling grateful. “You don’t really appreciate the effect of having a lethal disease until it’s not there anymore,” he says. “The world looks different when you have a future.”
This article was first published on Leaps.org on March 24, 2022.
A Stomach Implant Saved Me. When Your Organs Fail, You Could Become a Cyborg, Too
Ordinary people are living better with chronic conditions thanks to a recent explosion of developments in medical implants.
Beware, cyborgs walk among us. They’re mostly indistinguishable from regular humans and are infiltrating every nook and cranny of society. For full disclosure, I’m one myself. No, we’re not deadly intergalactic conquerors like the Borg race of Star Trek fame, just ordinary people living better with chronic conditions thanks to medical implants.
In recent years there has been an explosion of developments in implantable devices that merge multiple technologies into gadgets that work in concert with human physiology for the treatment of serious diseases. Pacemakers for the heart are the best-known implants, as well as other cardiac devices like LVADs (left-ventricular assist devices) and implanted defibrillators. Next-generation devices address an array of organ failures, and many are intended as permanent. The driving need behind this technology: a critical, persistent shortage of implantable biological organs.
The demand for transplantable organs dwarfs their availability. There are currently over 100,000 people on the transplant waiting list in the U.S., compared to 40,000 transplants completed in 2021. But even this doesn’t reflect the number of people in dire straits who don’t qualify for a transplant because of things like frailty, smoking status and their low odds of surviving the surgery.
My journey to becoming a cyborg came about because of a lifelong medical condition characterized by pathologically low motility of the digestive system, called gastroparesis. Ever since I was in my teens, I’ve had chronic problems with severe nausea. Flareups can be totally incapacitating and last anywhere from hours to months, interspersed with periods of relief. The cycle is totally unpredictable, and for decades my condition went both un- and misdiagnosed by doctors who were not even aware that the condition existed. Over the years I was labeled with whatever fashionable but totally inappropriate medical label existed at the time, and not infrequently, hypochondria.
Living with the gastric pacer is easy. In fact, most of the time, I don’t even know it’s there.
One of the biggest turning points in my life came when a surgeon at the George Washington University Hospital, Dr. Frederick Brody, ordered a gastric emptying test that revealed gastroparesis. This was in 2009, and an implantable device, called a gastric pacer, had been approved by the FDA for compassionate use, meaning that no other treatments were available. The small device is like a pacemaker that’s implanted beneath the skin of the abdomen and is attached to the stomach through electrodes that carry electrical pulses that stimulate the stomach, making it contract as it’s supposed to.
Dr. Brody implanted the electrical wires and the device, and, once my stomach started to respond to the pulses, I got the most significant nausea relief I’d had in decades of futile treatments. It sounds cliché to say that my debt to Dr. Brody is immeasurable, but the pacer has given me more years of relative normalcy than I previously could have dreamed of.
I should emphasize that the pacer is not a cure. I still take a lot of medicine and have to maintain a soft, primarily vegetarian diet, and the condition has progressed with age. I have ups and downs, and can still have periods of severe illness, but there’s no doubt I would be far worse off without the electrical stimulation provided by the pacer.
Living with the gastric pacer is easy. In fact, most of the time, I don’t even know it’s there. It entails periodic visits with a surgeon who can adjust the strength of the electrical pulses using a wireless device, so when symptoms are worse, he or she can amp up the juice. If the pulses are too strong, they can cause annoying contractions in the abdominal muscles, but this is easily fixed with a simple wireless adjustment. The battery runs down after a few years, and when this happens the whole device has to be replaced in what is considered minor surgery.
Such devices could fill gaps in treating other organ failures. By far most of the people on transplant waiting lists are waiting for kidneys. Despite the fact that live donations are possible, there’s still a dire shortage of organs. A bright spot on the horizon is The Kidney Project, a program spearheaded by bioengineer Shuvo Roy at the University of California, San Francisco, which is developing a fully implantable artificial kidney. The device combines living cells with artificial materials and relies not on a battery, but on the patient’s own blood pressure to keep it functioning.
Several years into this project, a prototype of the kidney, about the size of a smart phone, has been successfully tested in pigs. The device seems to provide many of the functions of a biological kidney (unlike dialysis, which replaces only one main function) and reliably produces urine. One of its most critical components is a special artificial membrane, called a hemofilter, that filters out toxins and waste products from the blood without leaking important molecules like albumin. Since it allows for total mobility, the artificial kidney will provide patients with a higher quality of life than those on dialysis, and is in some important ways, even better than a biological transplant.
The beauty of the device is that, even though it contains kidney cells sourced, as of now, from cadavers or pigs, the cells are treated so that they can’t be rejected and the device doesn’t require the highly problematic immunosuppressant drugs a biological organ requires. “Anti-rejection drugs,” says Roy, “make you susceptible to all kinds of infections and damage the transplanted organ, causing steady deterioration. Eventually they kill the kidney. A biological transplant has about a 10-year limit,” after which the kidney fails and the body rejects it.
Eventually, says Roy, the cells used in the artificial kidney will be sourced from the patient himself, the ultimate genetic match. The patient’s adult stem cells can be used to produce some or all of the 25 to 30 specialized cells of a biological kidney that provide all the functions of a natural organ. People formerly on dialysis could drastically improve their functionality and quality of life without being tethered to a machine for hours at a time, three days a week.
As exciting as this project is, it suffers from a common theme in early biomedical research—keeping a steady stream of funding that will move the project from the lab, into human clinical trials and eventually to the bedside. “It’s the issue,” says Roy. “Potential investors want to see more data indicating that it works, but you need funding to create data. It’s a Catch-22 that puts you in a kind of no-man’s land of funding.” The constant pursuit of funding introduces a variable that makes it hard to predict when the kidney will make it to market, despite the enormous need for such a technology.
Another critical variable is if and when insurance companies will decide to cover transplants with the artificial kidney, so that it becomes affordable for the average person. But Roy thinks that this hurdle, too, will be crossed. Insurance companies stand to save a great deal of money compared to what they ordinarily spend on transplant patients. The cost of yearly maintenance will be a fraction of that associated with the tens of thousands of dollars for immunosuppressant drugs and the attendant complications associated with a biological transplant.
One estimate that the multidisciplinary team of researchers involved with The Kidney Project are still trying to establish is how long the artificial kidney will last once transplanted into the body. Animal trials so far have been looking at how the kidney works for 30 days, and will soon extend that study to 90 days. Additional studies will extend much farther into the future, but first the kidneys have to be implanted into people who can be followed over many years to answer this question. But unlike the gastric pacer and other implants, there won’t be a need for periodic surgeries to replace a depleted battery, and the stark improvements in quality of life compared to dialysis add a special dimension to the value of whatever time the kidney lasts.
Another life-saving implant could address a major scourge of the modern world—heart disease. Despite significant advances in recent decades, including the cardiac implants mentioned above, cardiovascular disease still causes one in three deaths across the world. One of the most promising developments in recent years is the Total Artificial Heart, a pneumatically driven device that can be used in patients with biventricular heart failure, affecting both sides of the heart, when a biological organ is not available.
The TAH is implanted in the chest cavity and has two tubes that snake down the body, come out through the abdomen and attach to a 13.5-pound external driver that the patient carries around in a backpack. It was first developed as a bridge to transplant, a temporary alternative while the patient waited for a biological heart to replace it. However, SynCardia Systems, LLC, the Tucson-based company that makes it, is now investigating whether the heart can be used on a long-term basis.
There’s good reason to think that this will be the case. I spoke with Daniel Teo, one of the board members of SynCardia, who said that so far, one patient lived with the TAH for six years and nine months, before he died of other causes. Another patient, still alive, has lived with the device for over five years and another one has lived with it for over four years. About 2,000 of these transplants have been done in patients waiting for biological hearts so far, and most have lived mobile, even active lives. One TAH recipient hiked for 600 miles, and another ran the 4.2-mile Pat Tillman Run, both while on the artificial heart. This is a far cry from their activities before surgery, while living with advanced heart failure.

Randy Shepard, a recipient of the Total Artificial Heart, teaches archery to his son.
Randy Shepard
If removing and replacing one’s biological heart with a synthetic device sounds scary, it is. But then so is replacing one’s heart with biological one. “The TAH is very emotionally loaded for most people,” says Teo. “People sometimes hold back because of philosophical, existential questions and other nonmedical reasons.” He also cites cultural reasons why some people could be hesitant to accept an artificial heart, saying that some religions could frown upon it, just as they forbid other medical interventions.
The first TAHs that were approved were 70 cubic centimeters in size and fit into the chest cavities of men and larger women, but there’s now a smaller, 50 cc size meant for women and adolescents. The FDA first cleared the 70 cc heart as a bridge to transplant in 2004, and the 50 cc model received approval in 2014. SynCardia’s focus now is on seeking FDA approval to use the heart on a long-term basis. There are other improvements in the works.
One issue being refined deals with the external driver that holds the pneumatic device for moving the blood through a patient’s body. The two tubes connecting the driver to the heart entail openings in the skin that could get infected, and carrying the backpack is less than ideal. The driver also makes an audible sound that some people find disturbing. The next generation TAH will be quieter and involve wearing a smaller, lighter device on a belt rather than carrying the backpack. SynCardia is also working toward a fully implantable heart that wouldn’t require any external components and would contain an energy source that can be recharged wirelessly.
Teo says the jury is out as to whether artificial hearts will ever obviate the need for biological organs, but the world’s number one killer isn’t going away any time soon. “The heart is one of the strongest organs,” he says, “but it’s not made to last forever. If you live long enough, the heart will eventually fail, and heart failure leads to the failure of other organs like the kidney, the lungs and the liver.” As long as this remains the case and as long as the current direction of research continues, artificial organs are likely to play an ever larger part of our everyday lives.
Oh, wait. Maybe we cyborgs will take over the world after all.

