Scientists are making machines, wearable and implantable, to act as kidneys
Recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now
Like all those whose kidneys have failed, Scott Burton’s life revolves around dialysis. For nearly two decades, Burton has been hooked up (or, since 2020, has hooked himself up at home) to a dialysis machine that performs the job his kidneys normally would. The process is arduous, time-consuming, and expensive. Except for a brief window before his body rejected a kidney transplant, Burton has depended on machines to take the place of his kidneys since he was 12-years-old. His whole life, the 39-year-old says, revolves around dialysis.
“Whenever I try to plan anything, I also have to plan my dialysis,” says Burton says, who works as a freelance videographer and editor. “It’s a full-time job in itself.”
Many of those on dialysis are in line for a kidney transplant that would allow them to trade thrice-weekly dialysis and strict dietary limits for a lifetime of immunosuppressants. Burton’s previous transplant means that his body will likely reject another donated kidney unless it matches perfectly—something he’s not counting on. It’s why he’s enthusiastic about the development of artificial kidneys, small wearable or implantable devices that would do the job of a healthy kidney while giving users like Burton more flexibility for traveling, working, and more.
Still, the devices aren’t ready for testing in humans—yet. But recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now, according to Jonathan Himmelfarb, a nephrologist at the University of Washington.
“It would liberate people with kidney failure,” Himmelfarb says.
An engineering marvel
Compared to the heart or the brain, the kidney doesn’t get as much respect from the medical profession, but its job is far more complex. “It does hundreds of different things,” says UCLA’s Ira Kurtz.
Kurtz would know. He’s worked as a nephrologist for 37 years, devoting his career to helping those with kidney disease. While his colleagues in cardiology and endocrinology have seen major advances in the development of artificial hearts and insulin pumps, little has changed for patients on hemodialysis. The machines remain bulky and require large volumes of a liquid called dialysate to remove toxins from a patient’s blood, along with gallons of purified water. A kidney transplant is the next best thing to someone’s own, functioning organ, but with over 600,000 Americans on dialysis and only about 100,000 kidney transplants each year, most of those in kidney failure are stuck on dialysis.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. Each of the 45 different cell types in the kidney do something different.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. To build an artificial heart, Kurtz says, you basically need to engineer a pump. An artificial pancreas needs to balance blood sugar levels with insulin secretion. While neither of these tasks is simple, they are fairly straightforward. The kidney, on the other hand, does more than get rid of waste products like urea and other toxins. Each of the 45 different cell types in the kidney do something different, helping to regulate electrolytes like sodium, potassium, and phosphorous; maintaining blood pressure and water balance; guiding the body’s hormonal and inflammatory responses; and aiding in the formation of red blood cells.

There's been little progress for patients during Ira Kurtz's 37 years as a nephrologist. Artificial kidneys would change that.
UCLA
Dialysis primarily filters waste, and does so well enough to keep someone alive, but it isn’t a true artificial kidney because it doesn’t perform the kidney’s other jobs, according to Kurtz, such as sensing levels of toxins, wastes, and electrolytes in the blood. Due to the size and water requirements of existing dialysis machines, the equipment isn’t portable. Physicians write a prescription for a certain duration of dialysis and assess how well it’s working with semi-regular blood tests. The process of dialysis itself, however, is conducted blind. Doctors can’t tell how much dialysis a patient needs based on kidney values at the time of treatment, says Meera Harhay, a nephrologist at Drexel University in Philadelphia.
But it’s the impact of dialysis on their day-to-day lives that creates the most problems for patients. Only one-quarter of those on dialysis are able to remain employed (compared to 85% of similar-aged adults), and many report a low quality of life. Having more flexibility in life would make a major different to her patients, Harhay says.
“Almost half their week is taken up by the burden of their treatment. It really eats away at their freedom and their ability to do things that add value to their life,” she says.
Art imitates life
The challenge for artificial kidney designers was how to compress the kidney’s natural functions into a portable, wearable, or implantable device that wouldn’t need constant access to gallons of purified and sterilized water. The other universal challenge they faced was ensuring that any part of the artificial kidney that would come in contact with blood was kept germ-free to prevent infection.
As part of last year’s KidneyX Prize, a partnership between the U.S. Department of Health and Human Services and the American Society of Nephrology, inventors were challenged to create prototypes for artificial kidneys. Himmelfarb’s team at the University of Washington’s Center for Dialysis Innovation won the prize by focusing on miniaturizing existing technologies to create a portable dialysis machine. The backpack sized AKTIV device (Ambulatory Kidney to Increase Vitality) will recycle dialysate in a closed loop system that removes urea from blood and uses light-based chemical reactions to convert the urea to nitrogen and carbon dioxide, which allows the dialysate to be recirculated.
Himmelfarb says that the AKTIV can be used when at home, work, or traveling, which will give users more flexibility and freedom. “If you had a 30-pound device that you could put in the overhead bins when traveling, you could go visit your grandkids,” he says.
Kurtz’s team at UCLA partnered with the U.S. Kidney Research Corporation and Arkansas University to develop a dialysate-free desktop device (about the size of a small printer) as the first phase of a progression that will he hopes will lead to something small and implantable. Part of the reason for the artificial kidney’s size, Kurtz says, is the number of functions his team are cramming into it. Not only will it filter urea from blood, but it will also use electricity to help regulate electrolyte levels in a process called electrodeionization. Kurtz emphasizes that these additional functions are what makes his design a true artificial kidney instead of just a small dialysis machine.
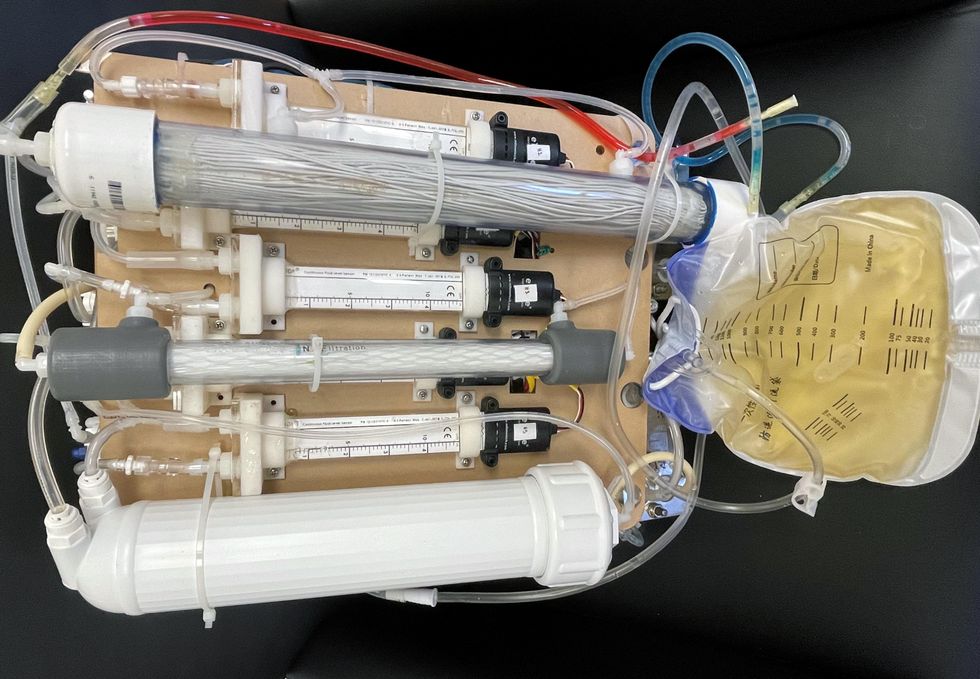
One version of an artificial kidney.
UCLA
“It doesn't have just a static function. It has a bank of sensors that measure chemicals in the blood and feeds that information back to the device,” Kurtz says.
Other startups are getting in on the game. Nephria Bio, a spinout from the South Korean-based EOFlow, is working to develop a wearable dialysis device, akin to an insulin pump, that uses miniature cartridges with nanomaterial filters to clean blood (Harhay is a scientific advisor to Nephria). Ian Welsford, Nephria’s co-founder and CTO, says that the device’s design means that it can also be used to treat acute kidney injuries in resource-limited settings. These potentials have garnered interest and investment in artificial kidneys from the U.S. Department of Defense.
For his part, Burton is most interested in an implantable device, as that would give him the most freedom. Even having a regular outpatient procedure to change batteries or filters would be a minor inconvenience to him.
“Being plugged into a machine, that’s not mimicking life,” he says.
Donna Shirley pictured at her home in Tulsa, with a model of the Sojourner rover she was in charge of that explored Mars.
When NASA's Perseverance rover landed successfully on Mars on February 18, 2021, calling it "one giant leap for mankind" – as Neil Armstrong said when he set foot on the moon in 1969 – would have been inaccurate. This year actually marked the fifth time the U.S. space agency has put a remote-controlled robotic exploration vehicle on the Red Planet. And it was a female engineer named Donna Shirley who broke new ground for women in science as the manager of both the Mars Exploration Program and the 30-person team that built Sojourner, the first rover to land on Mars on July 4, 1997.
For Shirley, the Mars Pathfinder mission was the climax of her 32-year career at NASA's Jet Propulsion Laboratory (JPL) in Pasadena, California. The Oklahoma-born scientist, who earned her Master's degree in aerospace engineering from the University of Southern California, saw her profile skyrocket with media appearances from CNN to the New York Times, and her autobiography Managing Martians came out in 1998. Now 79 and living in a Tulsa retirement community, she still embraces her status as a female pioneer.
"Periodically, I'll hear somebody say they got into the space program because of me, and that makes me feel really good," Shirley told Leaps.org. "I look at the mission control area, and there are a lot of women in there. I'm quite pleased I was able to break the glass ceiling."
Her $25-million, 25-pound microrover – powered by solar energy and designed to get rock samples and test soil chemistry for evidence of life – was named after Sojourner Truth, a 19th-century Black abolitionist and women's rights activist. Unlike Mars Pathfinder, Shirley didn't have to travel more than 131 million miles to reach her goal, but her path to scientific fame as a woman sometimes resembled an asteroid field.
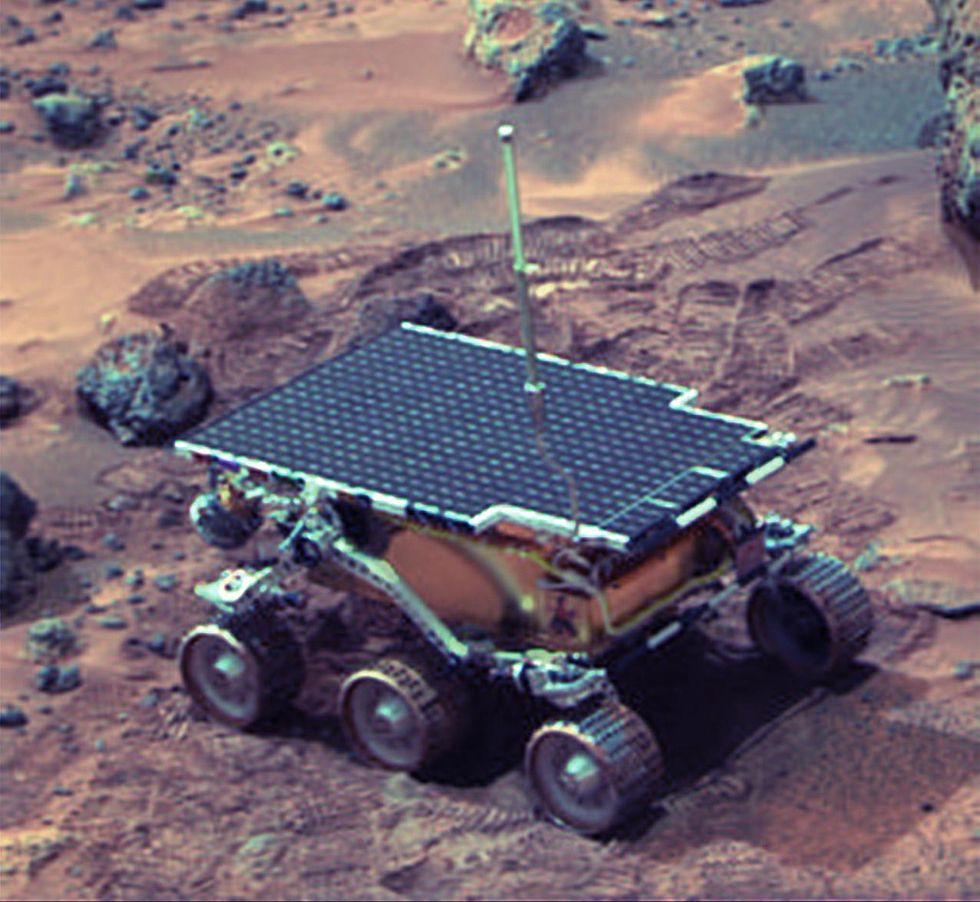 The Sojourner Rover in 1997 on Mars.NASA/JPL
The Sojourner Rover in 1997 on Mars.NASA/JPLAs a high-IQ tomboy growing up in Wynnewood, Oklahoma (pop. 2,300), Shirley yearned to escape. She decided to become an engineer at age 10 and took flying lessons at 15. Her extraterrestrial aspirations were fueled by Ray Bradbury's The Martian Chronicles and Arthur C. Clarke's The Sands of Mars. Yet when she entered the University of Oklahoma (OU) in 1958, her freshman academic advisor initially told her: "Girls can't be engineers." She ignored him.
Years later, Shirley would combat such archaic thinking, succeeding at JPL with her creative, collaborative management style. "If you look at the literature, you'll find that teams that are either led by or heavily involved with women do better than strictly male teams," she noted.
However, her career trajectory stalled at OU. Burned out by her course load and distracted by a broken engagement to marry a fellow student, she switched her major to professional writing. After graduation, she applied her aeronautical background as a McDonnell Aircraft technical writer, but her boss, she says, harassed her and she faced gender-based hostility from male co-workers.
Returning to OU, Shirley finished off her engineering degree and became a JPL aerodynamist in 1966 after answering an ad in the St. Louis Post-Dispatch. At first, she was the only female engineer among the research center's 2,000-odd engineers. She wore many hats, from designing planetary atmospheric entry vehicles to picking the launch date of November 4, 1973 for Mariner 10's mission to Venus and Mercury.
By the mid-1980's, she was managing teams that focused on robotics and Mars, delivering creative solutions when NASA budget cuts loomed. In 1989, the same year the Sojourner microrover concept was born, President George H.W. Bush announced his Space Exploration Initiative, including plans for a human mission to Mars by 2019.
That target, of course, wasn't attained, despite huge advances in technology and our understanding of the Martian environment. Today, Shirley believes humans could land on Mars by 2030. She became the founding director of the Science Fiction Museum and Hall of Fame in Seattle in 2004 after leaving NASA, and to this day, she enjoys checking out pop culture portrayals of Mars landings – even if they're not always accurate.
After the novel The Martian was published in 2011, which later was adapted into the hit film starring Matt Damon, Shirley phoned author Andy Weir: "You've got a major mistake in here. It says there's a storm that tries to blow the rocket over. But actually, the Mars atmosphere is so thin, it would never blow a rocket over!"
Fearlessly speaking her mind and seeking the stars helped Donna Shirley make history. However, a 2019 Washington Post story noted: "Women make up only about a third of NASA's workforce. They comprise just 28 percent of senior executive leadership positions and are only 16 percent of senior scientific employees." Whether it's traveling to Mars or trending toward gender equality, we've still got a long way to go.
Announcing March Event: "COVID Vaccines and the Return to Life: Part 1"
Leading medical and scientific experts will discuss the latest developments around the COVID-19 vaccines at our March 11th event.
EVENT INFORMATION
DATE:
Thursday, March 11th, 2021 at 12:30pm - 1:45pm EST
On the one-year anniversary of the global declaration of the pandemic, this virtual event will convene leading scientific and medical experts to discuss the most pressing questions around the COVID-19 vaccines. Planned topics include the effect of the new circulating variants on the vaccines, what we know so far about transmission dynamics post-vaccination, how individuals can behave post-vaccination, the myths of "good" and "bad" vaccines as more alternatives come on board, and more. A public Q&A will follow the expert discussion.
CONTACT:
kira@goodinc.com
LOCATION:
Zoom webinar
SPEAKERS:

Dr. Paul Offit speaking at Communicating Vaccine Science.
commons.wikimedia.orgDr. Paul Offit, M.D., is the director of the Vaccine Education Center and an attending physician in infectious diseases at the Children's Hospital of Philadelphia. He is a co-inventor of the rotavirus vaccine for infants, and he has lent his expertise to the advisory committees that review data on new vaccines for the CDC and FDA.

Dr. Monica Gandhi
UCSF Health
Dr. Monica Gandhi, M.D., MPH, is Professor of Medicine and Associate Division Chief (Clinical Operations/ Education) of the Division of HIV, Infectious Diseases, and Global Medicine at UCSF/ San Francisco General Hospital.

Dr. Onyema Ogbuagu, MBBCh, FACP, FIDSA
Yale Medicine
Dr. Onyema Ogbuagu, MBBCh, is an infectious disease physician at Yale Medicine who treats COVID-19 patients and leads Yale's clinical studies around COVID-19. He ran Yale's trial of the Pfizer/BioNTech vaccine.

Dr. Eric Topol
Dr. Topol's Twitter
Dr. Eric Topol, M.D., is a cardiologist, scientist, professor of molecular medicine, and the director and founder of Scripps Research Translational Institute. He has led clinical trials in over 40 countries with over 200,000 patients and pioneered the development of many routinely used medications.
REGISTER NOW
This event is the first of a four-part series co-hosted by LeapsMag, the Aspen Institute Science & Society Program, and the Sabin–Aspen Vaccine Science & Policy Group, with generous support from the Gordon and Betty Moore Foundation and the Howard Hughes Medical Institute.

Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.