Scientists are making machines, wearable and implantable, to act as kidneys
Recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now
Like all those whose kidneys have failed, Scott Burton’s life revolves around dialysis. For nearly two decades, Burton has been hooked up (or, since 2020, has hooked himself up at home) to a dialysis machine that performs the job his kidneys normally would. The process is arduous, time-consuming, and expensive. Except for a brief window before his body rejected a kidney transplant, Burton has depended on machines to take the place of his kidneys since he was 12-years-old. His whole life, the 39-year-old says, revolves around dialysis.
“Whenever I try to plan anything, I also have to plan my dialysis,” says Burton says, who works as a freelance videographer and editor. “It’s a full-time job in itself.”
Many of those on dialysis are in line for a kidney transplant that would allow them to trade thrice-weekly dialysis and strict dietary limits for a lifetime of immunosuppressants. Burton’s previous transplant means that his body will likely reject another donated kidney unless it matches perfectly—something he’s not counting on. It’s why he’s enthusiastic about the development of artificial kidneys, small wearable or implantable devices that would do the job of a healthy kidney while giving users like Burton more flexibility for traveling, working, and more.
Still, the devices aren’t ready for testing in humans—yet. But recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now, according to Jonathan Himmelfarb, a nephrologist at the University of Washington.
“It would liberate people with kidney failure,” Himmelfarb says.
An engineering marvel
Compared to the heart or the brain, the kidney doesn’t get as much respect from the medical profession, but its job is far more complex. “It does hundreds of different things,” says UCLA’s Ira Kurtz.
Kurtz would know. He’s worked as a nephrologist for 37 years, devoting his career to helping those with kidney disease. While his colleagues in cardiology and endocrinology have seen major advances in the development of artificial hearts and insulin pumps, little has changed for patients on hemodialysis. The machines remain bulky and require large volumes of a liquid called dialysate to remove toxins from a patient’s blood, along with gallons of purified water. A kidney transplant is the next best thing to someone’s own, functioning organ, but with over 600,000 Americans on dialysis and only about 100,000 kidney transplants each year, most of those in kidney failure are stuck on dialysis.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. Each of the 45 different cell types in the kidney do something different.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. To build an artificial heart, Kurtz says, you basically need to engineer a pump. An artificial pancreas needs to balance blood sugar levels with insulin secretion. While neither of these tasks is simple, they are fairly straightforward. The kidney, on the other hand, does more than get rid of waste products like urea and other toxins. Each of the 45 different cell types in the kidney do something different, helping to regulate electrolytes like sodium, potassium, and phosphorous; maintaining blood pressure and water balance; guiding the body’s hormonal and inflammatory responses; and aiding in the formation of red blood cells.

There's been little progress for patients during Ira Kurtz's 37 years as a nephrologist. Artificial kidneys would change that.
UCLA
Dialysis primarily filters waste, and does so well enough to keep someone alive, but it isn’t a true artificial kidney because it doesn’t perform the kidney’s other jobs, according to Kurtz, such as sensing levels of toxins, wastes, and electrolytes in the blood. Due to the size and water requirements of existing dialysis machines, the equipment isn’t portable. Physicians write a prescription for a certain duration of dialysis and assess how well it’s working with semi-regular blood tests. The process of dialysis itself, however, is conducted blind. Doctors can’t tell how much dialysis a patient needs based on kidney values at the time of treatment, says Meera Harhay, a nephrologist at Drexel University in Philadelphia.
But it’s the impact of dialysis on their day-to-day lives that creates the most problems for patients. Only one-quarter of those on dialysis are able to remain employed (compared to 85% of similar-aged adults), and many report a low quality of life. Having more flexibility in life would make a major different to her patients, Harhay says.
“Almost half their week is taken up by the burden of their treatment. It really eats away at their freedom and their ability to do things that add value to their life,” she says.
Art imitates life
The challenge for artificial kidney designers was how to compress the kidney’s natural functions into a portable, wearable, or implantable device that wouldn’t need constant access to gallons of purified and sterilized water. The other universal challenge they faced was ensuring that any part of the artificial kidney that would come in contact with blood was kept germ-free to prevent infection.
As part of last year’s KidneyX Prize, a partnership between the U.S. Department of Health and Human Services and the American Society of Nephrology, inventors were challenged to create prototypes for artificial kidneys. Himmelfarb’s team at the University of Washington’s Center for Dialysis Innovation won the prize by focusing on miniaturizing existing technologies to create a portable dialysis machine. The backpack sized AKTIV device (Ambulatory Kidney to Increase Vitality) will recycle dialysate in a closed loop system that removes urea from blood and uses light-based chemical reactions to convert the urea to nitrogen and carbon dioxide, which allows the dialysate to be recirculated.
Himmelfarb says that the AKTIV can be used when at home, work, or traveling, which will give users more flexibility and freedom. “If you had a 30-pound device that you could put in the overhead bins when traveling, you could go visit your grandkids,” he says.
Kurtz’s team at UCLA partnered with the U.S. Kidney Research Corporation and Arkansas University to develop a dialysate-free desktop device (about the size of a small printer) as the first phase of a progression that will he hopes will lead to something small and implantable. Part of the reason for the artificial kidney’s size, Kurtz says, is the number of functions his team are cramming into it. Not only will it filter urea from blood, but it will also use electricity to help regulate electrolyte levels in a process called electrodeionization. Kurtz emphasizes that these additional functions are what makes his design a true artificial kidney instead of just a small dialysis machine.
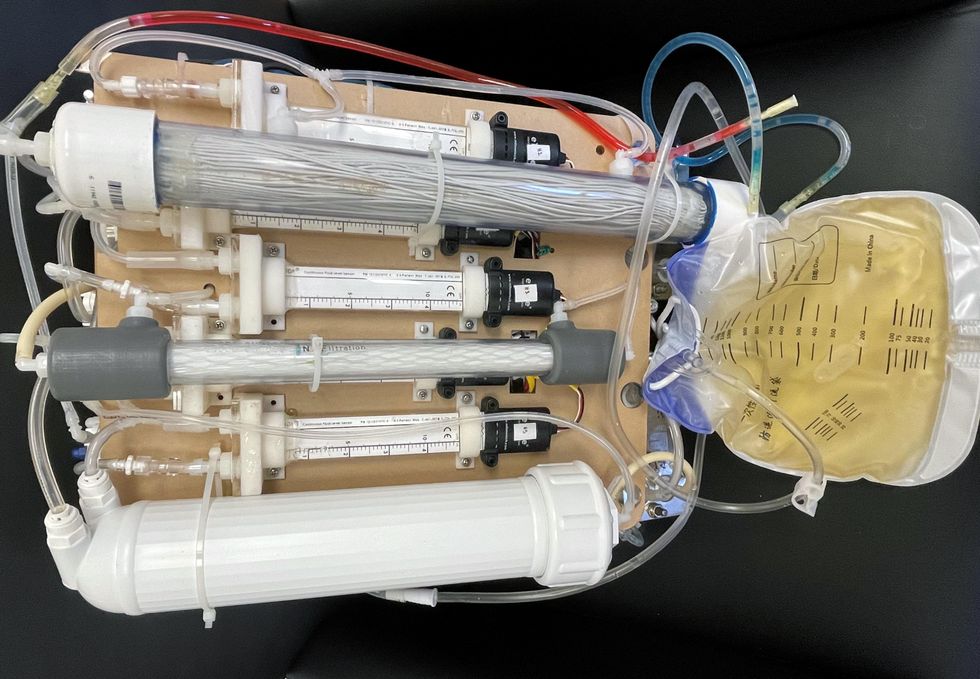
One version of an artificial kidney.
UCLA
“It doesn't have just a static function. It has a bank of sensors that measure chemicals in the blood and feeds that information back to the device,” Kurtz says.
Other startups are getting in on the game. Nephria Bio, a spinout from the South Korean-based EOFlow, is working to develop a wearable dialysis device, akin to an insulin pump, that uses miniature cartridges with nanomaterial filters to clean blood (Harhay is a scientific advisor to Nephria). Ian Welsford, Nephria’s co-founder and CTO, says that the device’s design means that it can also be used to treat acute kidney injuries in resource-limited settings. These potentials have garnered interest and investment in artificial kidneys from the U.S. Department of Defense.
For his part, Burton is most interested in an implantable device, as that would give him the most freedom. Even having a regular outpatient procedure to change batteries or filters would be a minor inconvenience to him.
“Being plugged into a machine, that’s not mimicking life,” he says.
Sharing land and other resources among farmers isn’t new. But research shows it may be increasingly relevant in a time of climatic upheaval.
The livestock trucks arrived all night. One after the other they backed up to the wood chute leading to a dusty corral and loosed their cargo — 580 head of cattle by the time the last truck pulled away at 3pm the next afternoon. Dan Probert, astride his horse, guided the cows to paddocks of pristine grassland stretching alongside the snow-peaked Wallowa Mountains. They’d spend the summer here grazing bunchgrass and clovers and biscuitroot. The scuffle of their hooves and nibbles of their teeth would mimic the elk, antelope and bison that are thought to have historically roamed this portion of northeastern Oregon’s Zumwalt Prairie, helping grasses grow and restoring health to the soil.
The cows weren’t Probert’s, although the fifth-generation rancher and one other member of the Carman Ranch Direct grass-fed beef collective also raise their own herds here for part of every year. But in spring, when the prairie is in bloom, Probert receives cattle from several other ranchers. As the grasses wither in October, the cows move on to graze fertile pastures throughout the Columbia Basin, which stretches across several Pacific Northwest states; some overwinter on a vegetable farm in central Washington, feeding on corn leaves and pea vines left behind after harvest.
Sharing land and other resources among farmers isn’t new. But research shows it may be increasingly relevant in a time of climatic upheaval, potentially influencing “farmers to adopt environmentally friendly practices and agricultural innovation,” according to a 2021 paper in the Journal of Economic Surveys. Farmers might share knowledge about reducing pesticide use, says Heather Frambach, a supply chain consultant who works with farmers in California and elsewhere. As a group they may better qualify for grants to monitor soil and water quality.
Most research around such practices applies to cooperatives, whose owner-members equally share governance and profits. But a collective like Carman Ranch’s — spearheaded by fourth-generation rancher Cory Carman, who purchases beef from eight other ranchers to sell under one “regeneratively” certified brand — shows when producers band together, they can achieve eco-benefits that would be elusive if they worked alone.
Vitamins and minerals in soil pass into plants through their roots, then into cattle as they graze, then back around as the cows walk around pooping.
Carman knows from experience. Taking over her family's land in 2003, she started selling grass-fed beef “because I really wanted to figure out how to not participate in the feedlot world, to have a healthier product. I didn't know how we were going to survive,” she says. Part of her land sits on a degraded portion of Zumwalt Prairie replete with invasive grasses; working to restore it, she thought, “What good does it do to kill myself trying to make this ranch more functional? If you want to make a difference, change has to be more than single entrepreneurs on single pieces of land. It has to happen at a community level.” The seeds of her collective were sown.
Raising 100 percent grass-fed beef requires land that’s got something for cows to graze in every season — which most collective members can’t access individually. So, they move cattle around their various parcels. It’s practical, but it also restores nutrient flows “to the way they used to move, from lowlands and canyons during the winter to higher-up places as the weather gets hot,” Carman says. Meaning, vitamins and minerals in soil pass into plants through their roots, then into cattle as they graze, then back around as the cows walk around pooping.

Cory Carman sells grass-fed beef, which requires land that’s got something for cows to graze in every season.
Courtesy Cory Carman
Each collective member has individual ecological goals: Carman brought in pigs to root out invasive grasses and help natives flourish. Probert also heads a more conventional grain-finished beef collective with 100 members, and their combined 6.5 million ranchland acres were eligible for a grant supporting climate-friendly practices, which compels them to improve soil and water health and biodiversity and make their product “as environmentally friendly as possible,” Probert says. The Washington veg farmer reduced tilling and pesticide use thanks to the ecoservices of visiting cows. Similarly, a conventional hay farmer near Carman has reduced his reliance on fertilizer by letting cattle graze the cover crops he plants on 80 acres.
Additionally, the collective must meet the regenerative standards promised on their label — another way in which they work together to achieve ecological goals. Says David LeZaks, formerly a senior fellow at finance-focused ecology nonprofit Croatan Institute, it’s hard for individual farmers to access monetary assistance. “But it's easier to get financing flowing when you increase the scale with cooperatives or collectives,” he says. “This supports producers in ways that can lead to better outcomes on the landscape.”
New, smaller scale farmers might gain the most from collective and cooperative models.
For example, it can help them minimize waste by using more of an animal, something our frugal ancestors excelled at. Small-scale beef producers normally throw out hides; Thousand Hills’ 50 regenerative beef producers together have enough to sell to Timberland to make carbon-neutral leather. In another example, working collectively resulted in the support of more diverse farms: Meadowlark Community Mill in Wisconsin went from working with one wheat grower, to sourcing from several organic wheat growers marketing flour under one premium brand.
Another example shows how these collaborations can foster greater equity, among other benefits: The Federation of Southern Cooperatives has a mission to support Black farmers as they build community health. It owns several hundred forest acres in Alabama, where it teaches members to steward their own forest land and use it to grow food — one member coop raises goats to graze forest debris and produce milk. Adding the combined acres of member forest land to the Federation’s, the group qualified for a federal conservation grant that will keep this resource available for food production, and community environmental and mental health benefits. “That's the value-add of the collective land-owner structure,” says Dãnia Davy, director of land retention and advocacy.
New, smaller scale farmers might gain the most from collective and cooperative models, says Jordan Treakle, national program coordinator of the National Family Farm Coalition (NFFC). Many of them enter farming specifically to raise healthy food in healthy ways — with organic production, or livestock for soil fertility. With land, equipment and labor prohibitively expensive, farming collectively allows shared costs and risk that buy farmers the time necessary to “build soil fertility and become competitive” in the marketplace, Treakle says. Just keeping them in business is an eco-win; when small farms fail, they tend to get sold for development or absorbed into less-diversified operations, so the effects of their success can “reverberate through the entire local economy.”
Frambach, the supply chain consultant, has been experimenting with what she calls “collaborative crop planning,” where she helps farmers strategize what they’ll plant as a group. “A lot of them grow based on what they hear their neighbor is going to do, and that causes really poor outcomes,” she says. “Nobody replanted cauliflower after the [atmospheric rivers in California] this year and now there's a huge shortage of cauliflower.” A group plan can avoid the under-planting that causes farmers to lose out on revenue.
It helps avoid overplanted crops, too, which small farmers might have to plow under or compost. Larger farmers, conversely, can sell surplus produce into the upcycling market — to Matriark Foods, for example, which turns it into value-add products like pasta sauce for companies like Sysco that supply institutional kitchens at colleges and hospitals. Frambach and Anna Hammond, Matriark’s CEO, want to collectivize smaller farmers so that they can sell to the likes of Matriark and “not lose an incredible amount of income,” Hammond says.
Ultimately, farming is fraught with challenges and even collectivizing doesn’t guarantee that farms will stay in business. But with agriculture accounting for almost 30 percent of greenhouse gas emissions globally, there's an “urgent” need to shift farming practices to more environmentally sustainable models, as well as a “demand in the marketplace for it,” says NFFC’s Treakle. “The growth of cooperative and collective farming can be a huge, huge boon for the ecological integrity of the system.”
Story by Big Think
We live in strange times, when the technology we depend on the most is also that which we fear the most. We celebrate cutting-edge achievements even as we recoil in fear at how they could be used to hurt us. From genetic engineering and AI to nuclear technology and nanobots, the list of awe-inspiring, fast-developing technologies is long.
However, this fear of the machine is not as new as it may seem. Technology has a longstanding alliance with power and the state. The dark side of human history can be told as a series of wars whose victors are often those with the most advanced technology. (There are exceptions, of course.) Science, and its technological offspring, follows the money.
This fear of the machine seems to be misplaced. The machine has no intent: only its maker does. The fear of the machine is, in essence, the fear we have of each other — of what we are capable of doing to one another.
How AI changes things
Sure, you would reply, but AI changes everything. With artificial intelligence, the machine itself will develop some sort of autonomy, however ill-defined. It will have a will of its own. And this will, if it reflects anything that seems human, will not be benevolent. With AI, the claim goes, the machine will somehow know what it must do to get rid of us. It will threaten us as a species.
Well, this fear is also not new. Mary Shelley wrote Frankenstein in 1818 to warn us of what science could do if it served the wrong calling. In the case of her novel, Dr. Frankenstein’s call was to win the battle against death — to reverse the course of nature. Granted, any cure of an illness interferes with the normal workings of nature, yet we are justly proud of having developed cures for our ailments, prolonging life and increasing its quality. Science can achieve nothing more noble. What messes things up is when the pursuit of good is confused with that of power. In this distorted scale, the more powerful the better. The ultimate goal is to be as powerful as gods — masters of time, of life and death.
Should countries create a World Mind Organization that controls the technologies that develop AI?
Back to AI, there is no doubt the technology will help us tremendously. We will have better medical diagnostics, better traffic control, better bridge designs, and better pedagogical animations to teach in the classroom and virtually. But we will also have better winnings in the stock market, better war strategies, and better soldiers and remote ways of killing. This grants real power to those who control the best technologies. It increases the take of the winners of wars — those fought with weapons, and those fought with money.
A story as old as civilization
The question is how to move forward. This is where things get interesting and complicated. We hear over and over again that there is an urgent need for safeguards, for controls and legislation to deal with the AI revolution. Great. But if these machines are essentially functioning in a semi-black box of self-teaching neural nets, how exactly are we going to make safeguards that are sure to remain effective? How are we to ensure that the AI, with its unlimited ability to gather data, will not come up with new ways to bypass our safeguards, the same way that people break into safes?
The second question is that of global control. As I wrote before, overseeing new technology is complex. Should countries create a World Mind Organization that controls the technologies that develop AI? If so, how do we organize this planet-wide governing board? Who should be a part of its governing structure? What mechanisms will ensure that governments and private companies do not secretly break the rules, especially when to do so would put the most advanced weapons in the hands of the rule breakers? They will need those, after all, if other actors break the rules as well.
As before, the countries with the best scientists and engineers will have a great advantage. A new international détente will emerge in the molds of the nuclear détente of the Cold War. Again, we will fear destructive technology falling into the wrong hands. This can happen easily. AI machines will not need to be built at an industrial scale, as nuclear capabilities were, and AI-based terrorism will be a force to reckon with.
So here we are, afraid of our own technology all over again.
What is missing from this picture? It continues to illustrate the same destructive pattern of greed and power that has defined so much of our civilization. The failure it shows is moral, and only we can change it. We define civilization by the accumulation of wealth, and this worldview is killing us. The project of civilization we invented has become self-cannibalizing. As long as we do not see this, and we keep on following the same route we have trodden for the past 10,000 years, it will be very hard to legislate the technology to come and to ensure such legislation is followed. Unless, of course, AI helps us become better humans, perhaps by teaching us how stupid we have been for so long. This sounds far-fetched, given who this AI will be serving. But one can always hope.