Scientists are making machines, wearable and implantable, to act as kidneys
Recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now
Like all those whose kidneys have failed, Scott Burton’s life revolves around dialysis. For nearly two decades, Burton has been hooked up (or, since 2020, has hooked himself up at home) to a dialysis machine that performs the job his kidneys normally would. The process is arduous, time-consuming, and expensive. Except for a brief window before his body rejected a kidney transplant, Burton has depended on machines to take the place of his kidneys since he was 12-years-old. His whole life, the 39-year-old says, revolves around dialysis.
“Whenever I try to plan anything, I also have to plan my dialysis,” says Burton says, who works as a freelance videographer and editor. “It’s a full-time job in itself.”
Many of those on dialysis are in line for a kidney transplant that would allow them to trade thrice-weekly dialysis and strict dietary limits for a lifetime of immunosuppressants. Burton’s previous transplant means that his body will likely reject another donated kidney unless it matches perfectly—something he’s not counting on. It’s why he’s enthusiastic about the development of artificial kidneys, small wearable or implantable devices that would do the job of a healthy kidney while giving users like Burton more flexibility for traveling, working, and more.
Still, the devices aren’t ready for testing in humans—yet. But recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now, according to Jonathan Himmelfarb, a nephrologist at the University of Washington.
“It would liberate people with kidney failure,” Himmelfarb says.
An engineering marvel
Compared to the heart or the brain, the kidney doesn’t get as much respect from the medical profession, but its job is far more complex. “It does hundreds of different things,” says UCLA’s Ira Kurtz.
Kurtz would know. He’s worked as a nephrologist for 37 years, devoting his career to helping those with kidney disease. While his colleagues in cardiology and endocrinology have seen major advances in the development of artificial hearts and insulin pumps, little has changed for patients on hemodialysis. The machines remain bulky and require large volumes of a liquid called dialysate to remove toxins from a patient’s blood, along with gallons of purified water. A kidney transplant is the next best thing to someone’s own, functioning organ, but with over 600,000 Americans on dialysis and only about 100,000 kidney transplants each year, most of those in kidney failure are stuck on dialysis.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. Each of the 45 different cell types in the kidney do something different.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. To build an artificial heart, Kurtz says, you basically need to engineer a pump. An artificial pancreas needs to balance blood sugar levels with insulin secretion. While neither of these tasks is simple, they are fairly straightforward. The kidney, on the other hand, does more than get rid of waste products like urea and other toxins. Each of the 45 different cell types in the kidney do something different, helping to regulate electrolytes like sodium, potassium, and phosphorous; maintaining blood pressure and water balance; guiding the body’s hormonal and inflammatory responses; and aiding in the formation of red blood cells.
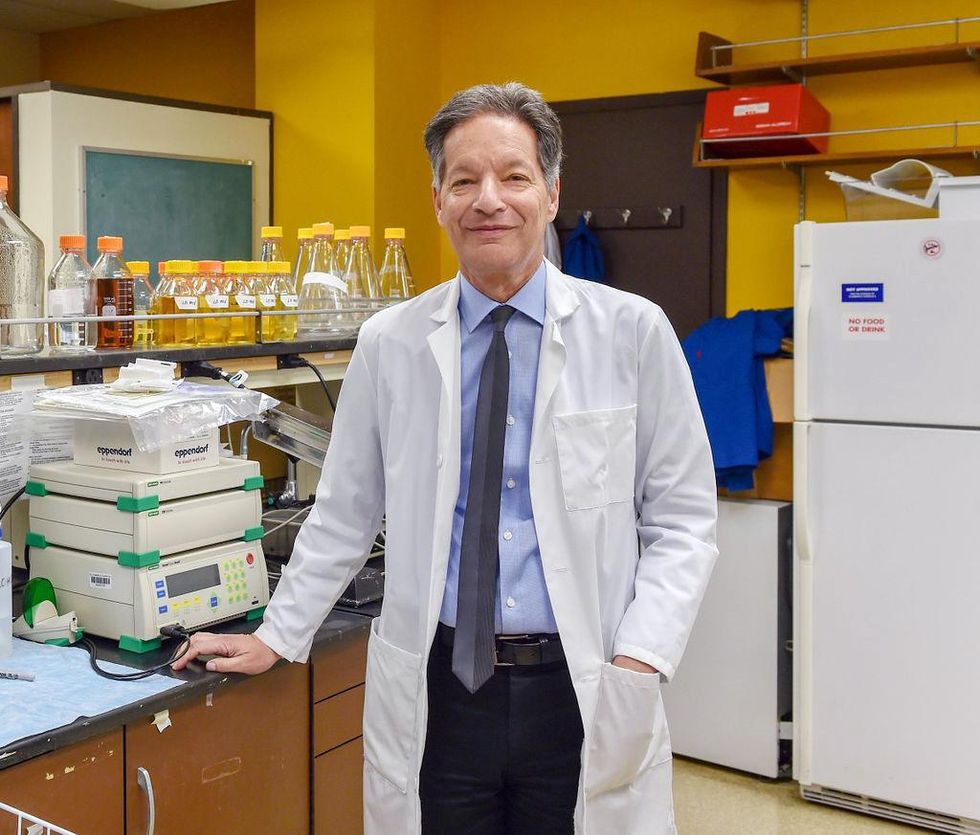
There's been little progress for patients during Ira Kurtz's 37 years as a nephrologist. Artificial kidneys would change that.
UCLA
Dialysis primarily filters waste, and does so well enough to keep someone alive, but it isn’t a true artificial kidney because it doesn’t perform the kidney’s other jobs, according to Kurtz, such as sensing levels of toxins, wastes, and electrolytes in the blood. Due to the size and water requirements of existing dialysis machines, the equipment isn’t portable. Physicians write a prescription for a certain duration of dialysis and assess how well it’s working with semi-regular blood tests. The process of dialysis itself, however, is conducted blind. Doctors can’t tell how much dialysis a patient needs based on kidney values at the time of treatment, says Meera Harhay, a nephrologist at Drexel University in Philadelphia.
But it’s the impact of dialysis on their day-to-day lives that creates the most problems for patients. Only one-quarter of those on dialysis are able to remain employed (compared to 85% of similar-aged adults), and many report a low quality of life. Having more flexibility in life would make a major different to her patients, Harhay says.
“Almost half their week is taken up by the burden of their treatment. It really eats away at their freedom and their ability to do things that add value to their life,” she says.
Art imitates life
The challenge for artificial kidney designers was how to compress the kidney’s natural functions into a portable, wearable, or implantable device that wouldn’t need constant access to gallons of purified and sterilized water. The other universal challenge they faced was ensuring that any part of the artificial kidney that would come in contact with blood was kept germ-free to prevent infection.
As part of last year’s KidneyX Prize, a partnership between the U.S. Department of Health and Human Services and the American Society of Nephrology, inventors were challenged to create prototypes for artificial kidneys. Himmelfarb’s team at the University of Washington’s Center for Dialysis Innovation won the prize by focusing on miniaturizing existing technologies to create a portable dialysis machine. The backpack sized AKTIV device (Ambulatory Kidney to Increase Vitality) will recycle dialysate in a closed loop system that removes urea from blood and uses light-based chemical reactions to convert the urea to nitrogen and carbon dioxide, which allows the dialysate to be recirculated.
Himmelfarb says that the AKTIV can be used when at home, work, or traveling, which will give users more flexibility and freedom. “If you had a 30-pound device that you could put in the overhead bins when traveling, you could go visit your grandkids,” he says.
Kurtz’s team at UCLA partnered with the U.S. Kidney Research Corporation and Arkansas University to develop a dialysate-free desktop device (about the size of a small printer) as the first phase of a progression that will he hopes will lead to something small and implantable. Part of the reason for the artificial kidney’s size, Kurtz says, is the number of functions his team are cramming into it. Not only will it filter urea from blood, but it will also use electricity to help regulate electrolyte levels in a process called electrodeionization. Kurtz emphasizes that these additional functions are what makes his design a true artificial kidney instead of just a small dialysis machine.
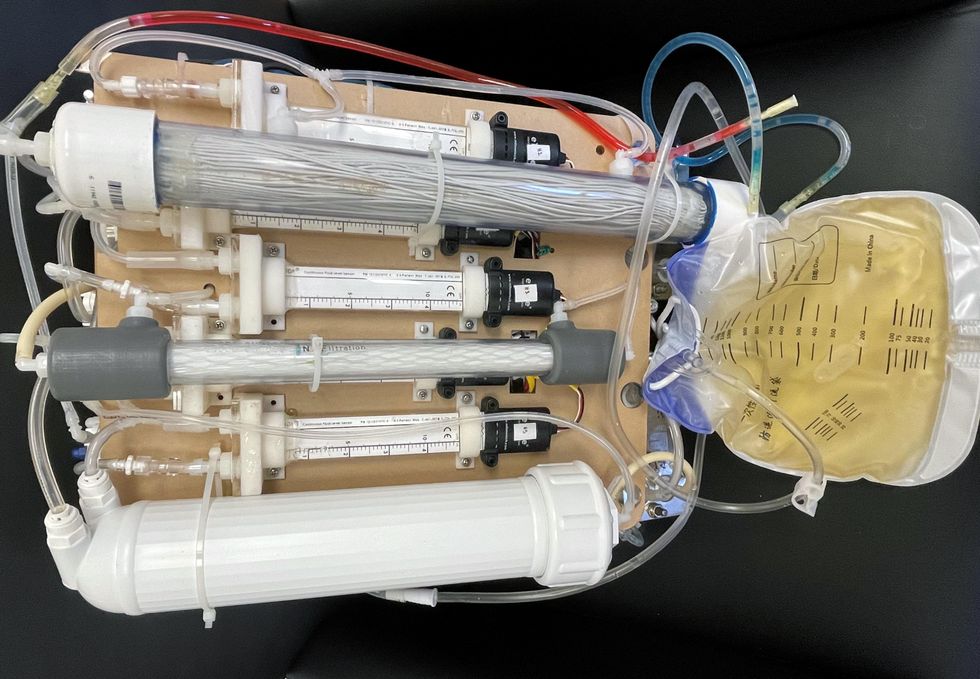
One version of an artificial kidney.
UCLA
“It doesn't have just a static function. It has a bank of sensors that measure chemicals in the blood and feeds that information back to the device,” Kurtz says.
Other startups are getting in on the game. Nephria Bio, a spinout from the South Korean-based EOFlow, is working to develop a wearable dialysis device, akin to an insulin pump, that uses miniature cartridges with nanomaterial filters to clean blood (Harhay is a scientific advisor to Nephria). Ian Welsford, Nephria’s co-founder and CTO, says that the device’s design means that it can also be used to treat acute kidney injuries in resource-limited settings. These potentials have garnered interest and investment in artificial kidneys from the U.S. Department of Defense.
For his part, Burton is most interested in an implantable device, as that would give him the most freedom. Even having a regular outpatient procedure to change batteries or filters would be a minor inconvenience to him.
“Being plugged into a machine, that’s not mimicking life,” he says.
Dec. 17th Event: The Latest on Omicron, Boosters, and Immunity
The Omicron variant poses new uncertainty for the vaccines, which four leading experts will address during our virtual event on December 17th, 2021.
This virtual event will convene leading scientific and medical experts to discuss the most pressing questions around the new Omicron variant, including what we know so far about its ability to evade COVID-19 vaccines, the role of boosters in eliciting heightened immunity, and the science behind variants and vaccines. A public Q&A will follow the expert discussion.
EVENT INFORMATION:
Date: Friday Dec 17, 2021
2:00pm - 3:30pm EST

Dr. Céline Gounder, MD, ScM, is the CEO/President/Founder of Just Human Productions, a non-profit multimedia organization. She is also the host and producer of American Diagnosis, a podcast on health and social justice, and Epidemic, a podcast about infectious disease epidemics and pandemics. She served on the Biden-Harris Transition COVID-19 Advisory Board.
 Dr. Theodora Hatziioannou, Ph.D., is a Research Associate Professor in the Laboratory of Retrovirology at The Rockefeller University. Her research includes identifying plasma samples from recovered COVID-19 patients that contain antibodies capable of neutralizing the SARS-CoV-2 coronavirus.
Dr. Theodora Hatziioannou, Ph.D., is a Research Associate Professor in the Laboratory of Retrovirology at The Rockefeller University. Her research includes identifying plasma samples from recovered COVID-19 patients that contain antibodies capable of neutralizing the SARS-CoV-2 coronavirus.

Dr. Onyema Ogbuagu, MBBCh, is an Associate Professor at Yale School of Medicine and an infectious disease specialist who treats COVID-19 patients and leads Yale’s clinical studies around COVID-19. He ran Yale’s trial of the Pfizer/BioNTech vaccine.

Dr. Eric Topol, M.D., is a cardiologist, scientist, professor of molecular medicine, and the director and founder of Scripps Research Translational Institute. He has led clinical trials in over 40 countries with over 200,000 patients and pioneered the development of many routinely used medications.
This event is the fourth of a four-part series co-hosted by Leaps.org, the Aspen Institute Science & Society Program, and the Sabin–Aspen Vaccine Science & Policy Group, with generous support from the Gordon and Betty Moore Foundation and the Howard Hughes Medical Institute.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
7 Things to Know about the U.S.’s Capability to Detect Omicron
A visualization of the original coronavirus causing COVID-19, which has now been detected across the globe in a highly mutated form called Omicron.
If the new variant Omicron isn’t here already – which many experts suspect that it is – it will be soon. While we wait for scientists to conduct the necessary research to characterize its transmissibility, potential fitness at immune evasion, and disease severity, we wanted to give Leaps.org readers a window into how the U.S. is positioned to detect the variant. So we spoke to Kelly Wroblewski, director of infectious diseases at the Association of Public Health Laboratories, a membership organization that represents state and local government health labs in the United States. Here are seven insights she shared.
1) If you test positive for COVID-19 with a standard PCR test, the diagnostic report will not tell you which variant you have. There are no diagnostic tests available for your doctor to order to identify variants. To find out the variant, the specimen must be sent to a commercial, clinical, academic, or public health laboratory for genetic sequencing.
2) Today, the U.S. sequences about 5 to 10 percent of all diagnostic specimens that test positive for SARS-CoV-2 in order to determine which variants are circulating and where. Last week nationally, for example, labs sequenced about 80,000 samples. This represents a massive increase from last year at this time, when labs were only sequencing about 8,000 specimens per week. Currently, 99.5 percent of circulating SARS-CoV-2 virus in the U.S. is the Delta variant.
3) The U.S. is “very well prepared” to detect Omicron, Wroblewski says, “particularly compared to where we were when the Alpha variant, or B117 first emerged.” Of the hunt for Omicron, she adds, “it’s very reminiscent of that time, except we are doing so much more sequencing and we have so much better coverage with our sequencing geographically, and we're doing it in a much more timely way. We have the ability to find emerging variants that are circulating in 0.01 percent of the population.”
4) Deciding which specimens to sample is not totally random. Samples that have more virus are likely to lead to better sequencing results. Labs also look to have a diverse set of representative samples, meaning across geographic regions and across gender, race, ethnicity, and age groups. Clinical diversity is also important, such as including pregnant women, severe in-patient cases, mild cases, etc.
5) Sequencing more is not necessarily better to find Omicron faster. “We will increase the number of sequences to a certain extent,” Wroblewski says. “Where we exhibit some caution is doing that indiscriminately isn’t the most effective use of time and resources. The important thing is to try to find Omicron, and if you increase your testing capacity too much, right now, it's still predominantly Delta in the U.S. by a long shot. So you’re mostly going to sequence Delta and you run the risk of delaying your discovery of Omicron, if you focus solely on increasing sequencing.”
So besides just ramping up the sheer numbers of sequencing, diagnostic labs across the country are now advised to preferentially use a certain PCR test made by Thermo Fisher that can help hasten the detection of Omicron. It turns out that Omicron’s specific mutations in the Spike protein mean that the Spike is not picked up on this PCR test, which yields a type of result called an S-gene target failure. Yet the test will still accurately pick up a COVID-19 diagnosis, because it detects two other gene targets on Omicron that are not mutated. “That S-gene target failure gives you a good indication that you may have Omicron. It’s a good early screen.”
Labs will then still need to sequence the whole genome to confirm it matches the Omicron sequence. “So right now, the new recommendation is to use [the Thermo Fisher test] as much as possible to give us a better chance of detecting Omicron more quickly.”
6) This Thermo Fisher test is “fairly widely used” in the U.S. already, so many labs are already well positioned to make the shift. “In early to mid 2020,” Wroblewski explains, “when the supply chain issue for testing was acute, many public health labs implemented five, six, seven, eight different tests, just so they could get enough supplies to do all the testing. Now that we're in a much better place supply-chain wise, it's very difficult and time consuming and cumbersome to maintain all those different test methods all the time, and many, many labs scaled back to only one or two. And so this [new recommendation] would just be shifting to two for some labs that will be shifting to them.”
7) Once Omicron is found here, labs will be focused on finding as many cases as possible, and the CDC will be conducting a variety of studies to determine the impact of the variant on diagnostics, therapeutics, and vaccines. Epidemiologists at the local, state, and federal level will analyze which populations it is spreading in, as well as the severity of the disease it causes. They will work to sort out different impacts on vaccinated vs. unvaccinated populations. The ultimate goal, Wroblewski concludes, is to “use all of that information to make better public health decisions and inform the public about what’s going on.”
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.