Why the Panic Over "Designer Babies" Is the Wrong Worry

BIG QUESTION OF THE MONTH: Should we use CRISPR, the new technique that enables precise DNA editing, to change the genes of human embryos to eradicate disease--or even to enhance desirable traits? LeapsMag invited three leading experts to weigh in.
CRISPR is producing an important revolution in the biosciences, a revolution that will change our world in fundamental ways. Its implications need to be discussed and debated, and not just by scientists and ethicists. Unfortunately, so far we are debating the wrong issues.
Controversy has raged about editing human genes, particularly the DNA of embryos that could pass the changes down to their descendants. This technology, human germline editing, seems highly unlikely to be broadly available for at least the next few decades; if and when it is, it may well be unimportant.
Human germline editing is unlikely to happen soon because it has important safety risks but almost no significant benefits.
Human germline editing is unlikely to happen soon because it has important safety risks but almost no significant benefits. The risks – harm to babies – are compelling. We care a lot about babies. A technology that worked 95 percent of the time (and produced disabled or dying infants "only" five percent of the time) would be a disaster. Our concern for babies will lead, at the least, to rigorous legal requirements for preapproval safety testing. Many countries will just impose flat bans.
But these risks also have implications beyond safety regulation. For this technology to take off, physicians, assisted reproduction clinics, and geneticists will have to be willing to put their reputations – and their malpractice liability – on the line. And prospective mothers will have to be willing to take unknown risks with their children.
Sometimes, large and unknown risks are worth taking, but not here. For the next few decades, human germline editing offers almost no substantial benefits, for health or for enhancement.
Prospective parents already have a tried and true alternative to avoid having children with genetic diseases: preimplantation genetic diagnosis (PGD). In PGD, clinicians remove cells from three- to five-day-old embryos. Those cells are then tested to see which embryos would inherit the disease and which would not. This technology has been in use for over 27 years and is safe and effective. Rather than engaging in editing an embryo's disease-causing DNA, parents can just select embryos without those DNA variations. For so-called autosomal recessive diseases, three out of four embryos, on average, will be disease free; for autosomal dominant diseases, half will be.
Only a handful of prospective parents would need to use gene editing to avoid genetic disease.
Couples where each has the same recessive condition (cystic fibrosis) or where one of them has the terrible luck to have two copies of the DNA variant for a dominant disease (Huntington's disease). In those cases, the prospective parents would need to stay alive long enough to be able, and be sufficiently healthy to want, to have children. In a world of 7.3 billion humans, there will be some such cases, but they will probably be no more than a few thousand – or hundred.
People are also concerned about germline editing for genetic enhancement. But this is also unlikely anytime soon. We know basically nothing about genetic variations that enhance people beyond normal. For example, we know hundreds of genes that, when damaged, affect intelligence – but these all cause very low intelligence. We know of no variations that non-trivially increase it.
Over the next few decades, we might (or might not) learn about complex diseases where several genes are involved, making embryo selection less useful. And we might (or might not) learn about genetic enhancements involving DNA sequences not typically found in prospective parents and so not available to embryo selection. By that time, the safety issues could be resolved.
And, even then, how worried should we be – and about what? A bit, but not very and not about much.
"The human germline genome is not the holy essence of humanity."
The human germline genome is not the holy essence of humanity. For one thing, it doesn't really exist. There are 7.3 billion human germline genomes; each of us has a different one. And those genomes change every generation. I do not have exactly the same genetic variations my parents received from my grandparents; my children do not have exactly the ones I received from my parents. The DNA changed, through mutation, during each generation.
And our editing will usually be insignificant in the context of the whole human genome. For medical purposes, we will change some rare DNA variations that cause disease into the much more common DNA variations that do not cause disease. Rare, nasty variants will become rarer, but civilization changes these frequencies all the time. For instance, the use of insulin has increased the number of people with DNA variations that predispose people to type 1 ("juvenile") diabetes – because now those people live long enough to reproduce. Even agriculture changed our DNA, leading, for example, to more copies of starch-digesting genes. And, in any event, what is the meaningful difference between "fixing" a disease gene in an embryo or waiting to fix it with gene therapy in a born baby . . . other than avoiding the need to repeat the gene therapy in the next generation?
If genetic enhancement ever becomes possible in a non-trivial way, it would raise important questions, but questions about enhancement generally and not fundamentally about genetics. Enhancement through drugs, prosthetics, brain-computer interfaces, genes, or tools (like the laptop I wrote this on) all raise similar ethical issues. We can use the decades we will have to try to think more systematically about the ethical and policy issues for all enhancements. We should not panic about germline genetic enhancement.
One superficially appealing argument is that we are not wise enough to change our own genomes. This ignores the fact that we have been changing our genomes, inadvertently, since at least the dawn of civilization. We do not have to be wise enough to change our genome perfectly; we just need to be wise enough to change it better than the random and unforeseen ways we change it now. That should not be beyond our power.
Human germline editing will not be a concern for several decades and it may never be an important concern. What should we be paying attention to?
Non-human genome editing. Governments, researchers, and even do-it-yourself hobbyists can use CRISPR, especially when coupled with a technique called "gene drive," to change the genomes of whole species of living things – domestic or wild; animal, vegetable, or microbial – cheaply, easily, and before we even know it is happening. We care much less about mosquito babies than human ones and our legal structures are not built for wise and nuanced regulation of this kind of genome editing. Those issues demand our urgent attention – if we can tear ourselves away from dramatic but less important visions of "designer babies."
Editor's Note: Check out the viewpoints expressing condemnation and enthusiastic support.
A robot server, controlled remotely by a disabled worker, delivers drinks to patrons at the DAWN cafe in Tokyo.
A sleek, four-foot tall white robot glides across a cafe storefront in Tokyo’s Nihonbashi district, holding a two-tiered serving tray full of tea sandwiches and pastries. The cafe’s patrons smile and say thanks as they take the tray—but it’s not the robot they’re thanking. Instead, the patrons are talking to the person controlling the robot—a restaurant employee who operates the avatar from the comfort of their home.
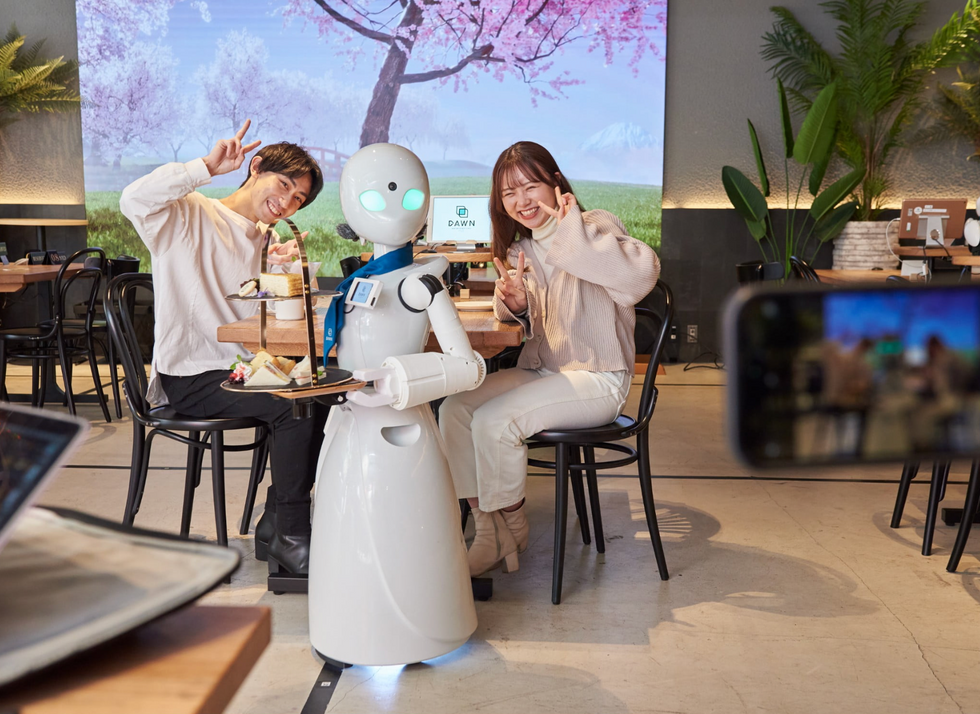
It’s a typical scene at DAWN, short for Diverse Avatar Working Network—a cafe that launched in Tokyo six years ago as an experimental pop-up and quickly became an overnight success. Today, the cafe is a permanent fixture in Nihonbashi, staffing roughly 60 remote workers who control the robots remotely and communicate to customers via a built-in microphone.
More than just a creative idea, however, DAWN is being hailed as a life-changing opportunity. The workers who control the robots remotely (known as “pilots”) all have disabilities that limit their ability to move around freely and travel outside their homes. Worldwide, an estimated 16 percent of the global population lives with a significant disability—and according to the World Health Organization, these disabilities give rise to other problems, such as exclusion from education, unemployment, and poverty.
These are all problems that Kentaro Yoshifuji, founder and CEO of Ory Laboratory, which supplies the robot servers at DAWN, is looking to correct. Yoshifuji, who was bedridden for several years in high school due to an undisclosed health problem, launched the company to help enable people who are house-bound or bedridden to more fully participate in society, as well as end the loneliness, isolation, and feelings of worthlessness that can sometimes go hand-in-hand with being disabled.
“It’s heartbreaking to think that [people with disabilities] feel they are a burden to society, or that they fear their families suffer by caring for them,” said Yoshifuji in an interview in 2020. “We are dedicating ourselves to providing workable, technology-based solutions. That is our purpose.”

Shota, Kuwahara, a DAWN employee with muscular dystrophy, agrees. "There are many difficulties in my daily life, but I believe my life has a purpose and is not being wasted," he says. "Being useful, able to help other people, even feeling needed by others, is so motivational."
A woman receives a mammogram, which can detect the presence of tumors in a patient's breast.
When a patient is diagnosed with early-stage breast cancer, having surgery to remove the tumor is considered the standard of care. But what happens when a patient can’t have surgery?
Whether it’s due to high blood pressure, advanced age, heart issues, or other reasons, some breast cancer patients don’t qualify for a lumpectomy—one of the most common treatment options for early-stage breast cancer. A lumpectomy surgically removes the tumor while keeping the patient’s breast intact, while a mastectomy removes the entire breast and nearby lymph nodes.
Fortunately, a new technique called cryoablation is now available for breast cancer patients who either aren’t candidates for surgery or don’t feel comfortable undergoing a surgical procedure. With cryoablation, doctors use an ultrasound or CT scan to locate any tumors inside the patient’s breast. They then insert small, needle-like probes into the patient's breast which create an “ice ball” that surrounds the tumor and kills the cancer cells.
Cryoablation has been used for decades to treat cancers of the kidneys and liver—but only in the past few years have doctors been able to use the procedure to treat breast cancer patients. And while clinical trials have shown that cryoablation works for tumors smaller than 1.5 centimeters, a recent clinical trial at Memorial Sloan Kettering Cancer Center in New York has shown that it can work for larger tumors, too.
In this study, doctors performed cryoablation on patients whose tumors were, on average, 2.5 centimeters. The cryoablation procedure lasted for about 30 minutes, and patients were able to go home on the same day following treatment. Doctors then followed up with the patients after 16 months. In the follow-up, doctors found the recurrence rate for tumors after using cryoablation was only 10 percent.
For patients who don’t qualify for surgery, radiation and hormonal therapy is typically used to treat tumors. However, said Yolanda Brice, M.D., an interventional radiologist at Memorial Sloan Kettering Cancer Center, “when treated with only radiation and hormonal therapy, the tumors will eventually return.” Cryotherapy, Brice said, could be a more effective way to treat cancer for patients who can’t have surgery.
“The fact that we only saw a 10 percent recurrence rate in our study is incredibly promising,” she said.

