Repairing Cells and Longevity Myths with Dr. Charles Brenner

Charles Brenner, a leading biochemist at City of Hope National Medical Center in L.A., discovered a vitamin precursor called NR that seems to enable repair of cellular damage that happens as we get older.
Meet Charles Brenner, the Longevity Skeptic. Brenner, a leading biochemist at City of Hope National Medical Center in L.A., has been attending the largest longevity conferences with one main purpose: to point out that some of the other speakers are full of it.
Brenner is "throwing cold water" on several scientists in the field of aging, accusing them of hyping various fountains of youth, despite limited evidence for these therapies.
In this podcast episode, Brenner sat down with Leaps.org to discuss his groundbreaking work on metabolism and his efforts to counter what he considers to be bad science.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
In addition to bringing his candor to conferences, Brenner is applying it in academic journals, publishing a paper in September, "A Science-Based Review of the World's Best-Selling Book on Aging," in which he pans the author of this bestseller, David Sinclair, a Harvard biologist, for talking up the potential for humans to live far past 100. These aspirations may sound nice, but they're not backed by science, Brenner says. He's had high-profile debates online with Sinclair and Aubrey de Grey, a prominent biomedical gerontologist.
Meanwhile, in his own lab work, Brenner is credited with identifying a vitamin precursor called NR that seems to enable repair of cellular damage that happens as we get older - a major discovery that he's helped turn into a supplement, commercialized with a company called ChromaDex.
Whether it's possible to extend human lifespan is a pressing question as investments in longevity startups are projected to increase from $40 billion to $600 billion over the next three years. The field of biological aging seems split on the question of whether "anti-aging" therapies can significantly lengthen our natural lifespans, as Sinclair believes. Brenner, Morgan Levine of Altos Labs and Matt Kaeberlein of the University of Washington have argued that the only realistic goal is to extend one's window of healthy years, or healthspan, rather than trying to break the biological ceiling of our species.
Brenner is an intriguing figure in these debates. Although he’s been introduced in public appearances as a longevity skeptic, he calls himself an optimist.
Links:
Charles Brenner, City of Hope
Charles Brenner on Twitter
Charles Brenner's debate with Aubrey de Grey
Brenner's paper, "A Science-Based Review of the World's Best-Selling Book on Aging"
Peter Attia's recent blog on NR supplements
Brad Stanfield's recent reaction to "David Sinclair vs Charles Brenner"
ChromaDex NR supplement
Life is Emerging: Review of Siddhartha Mukherjee’s Song of the Cell
A new book by Pulitzer-winning physician-scientist Siddhartha Mukherjee will be released from Simon & Schuster on October 25, 2022.
The DNA double helix is often the image spiraling at the center of 21st century advances in biomedicine and the growing bioeconomy. And yet, DNA is molecularly inert. DNA, the code for genes, is not alive and is not strictly necessary for life. Ought life be at the center of our communication of living systems? Is not the Cell a superior symbol of life and our manipulation of living systems?
A code for life isn’t a code without the life that instantiates it. A code for life must be translated. The cell is the basic unit of that translation. The cell is the minimal viable package of life as we know it. Therefore, cell biology is at the center of biomedicine’s greatest transformations, suggests Pulitzer-winning physician-scientist Siddhartha Mukherjee in his latest book, The Song of the Cell: The Exploration of Medicine and the New Human.
The Song of the Cell begins with the discovery of cells and of germ theory, featuring characters such as Louis Pasteur and Robert Koch, who brought the cell “into intimate contact with pathology and medicine.” This intercourse would transform biomedicine, leading to the insight that we can treat disease by thinking at the cellular level. The slightest rearrangement of sick cells might be the path toward alleviating suffering for the organism: eroding the cell walls of a bacterium while sparing our human cells; inventing a medium that coaxes sperm and egg to dance into cellular union for in vitro fertilization (IVF); designing molecular missiles that home to the receptors decorating the exterior of cancer cells; teaching adult skin cells to remember their embryonic state for regenerative medicines.
Mukherjee uses the bulk of the book to elucidate key cell types in the human body, along with their “connective relationships” that enable key organs and organ systems to function. This includes the immune system, the heart, the brain, and so on. Mukherjee’s distinctive style features compelling anecdotes and human stories that animate the scientific (and unscientific) processes that have led to our current state of understanding. In his chapter on neurons and the brain, for example, he integrates Santiago Ramon y Cajal’s meticulous black ink sketches of neurons into Mukherjee’s own personal encounter with clinical depression. In one lucid section, he interviews Dr. Helen Mayberg, a pioneering neurologist who takes seriously the descriptive power of her patients’ metaphors, as they suffer from “caves,” “holes,” “voids,” and “force fields” that render their lives gray. Dr. Mayberg aims to stimulate patients’ neuronal cells in a manner that brings back the color.
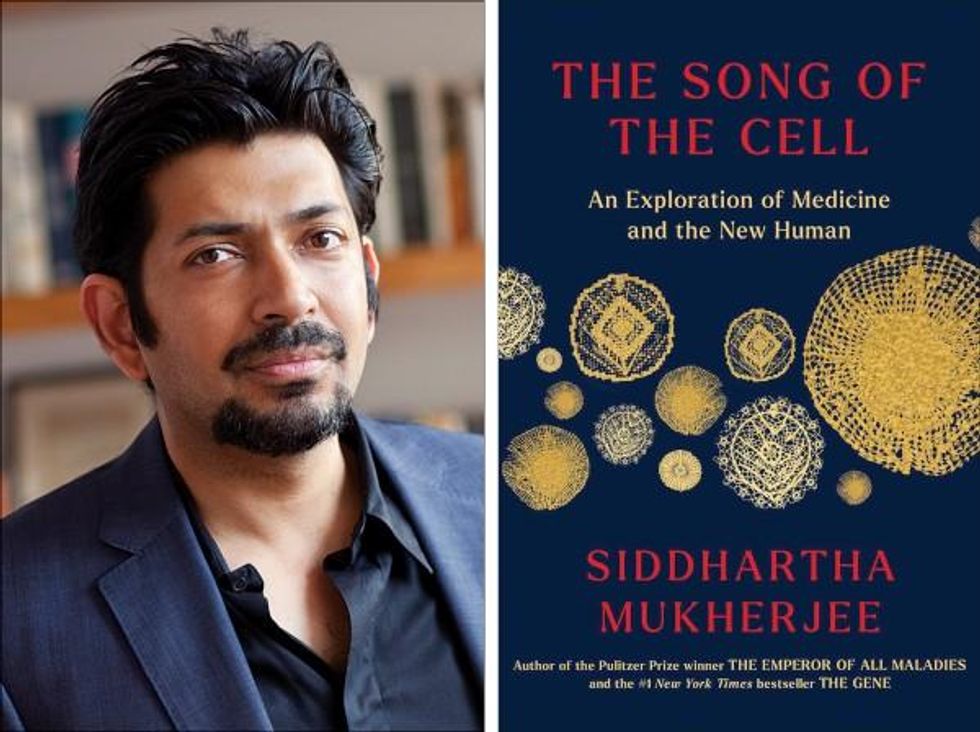
Beyond exposing the insight and inventiveness that has arisen out of cell-based thinking, it seems that Mukherjee’s bigger project is an epistemological one. The early chapters of The Song of the Cell continually hint at the potential for redefining the basic unit of biology as the cell rather than the gene. The choice to center biomedicine around cells is, above all, a conspicuous choice not to center it around genes (the subject of Mukherjee’s previous book, The Gene), because genes dominate popular science communication.
This choice of cells over genes is most welcome. Cells are alive. Genes are not. Letters—such as the As, Cs, Gs, and Ts that represent the nucleotides of DNA, which make up our genes—must be synthesized into a word or poem or song that offers a glimpse into deeper truths. A key idea embedded in this thinking is that of emergence. Whether in ancient myth or modern art, creation tends to be an emergent process, not a linearly coded script. The cell is our current best guess for the basic unit of life’s emergence, turning a finite set of chemical building blocks—nucleic acids, proteins, sugars, fats—into a replicative, evolving system for fighting stasis and entropy. The cell’s song is one for our times, for it is the song of biology’s emergence out of chemistry and physics, into the “frenetically active process” of homeostasis.
Re-centering our view of biology has practical consequences, too, for how we think about diagnosing and treating disease, and for inventing new medicines. Centering cells presents a challenge: which type of cell to place at the center? Rather than default to the apparent simplicity of DNA as a symbol because it represents the one master code for life, the tension in defining the diversity of cells—a mapping process still far from complete in cutting-edge biology laboratories—can help to create a more thoughtful library of cellular metaphors to shape both the practice and communication of biology.
Further, effective problem solving is often about operating at the right level, or the right scale. The cell feels like appropriate level at which to interrogate many of the diseases that ail us, because the senses that guide our own perceptions of sickness and health—the smoldering pain of inflammation, the tunnel vision of a migraine, the dizziness of a fluttering heart—are emergent.
This, unfortunately, is sort of where Mukherjee leaves the reader, under-exploring the consequences of a biology of emergence. Many practical and profound questions have to do with the ways that each scale of life feeds back on the others. In a tome on Cells and “the future human” I wished that Mukherjee had created more space for seeking the ways that cells will shape and be shaped by the future, of humanity and otherwise.
We are entering a phase of real-world bioengineering that features the modularization of cellular parts within cells, of cells within organs, of organs within bodies, and of bodies within ecosystems. In this reality, we would be unwise to assume that any whole is the mere sum of its parts.
For example, when discussing the regenerative power of pluripotent stem cells, Mukherjee raises the philosophical thought experiment of the Delphic boat, also known as the Ship of Theseus. The boat is made of many pieces of wood, each of which is replaced for repairs over the years, with the boat’s structure unchanged. Eventually none of the boat’s original wood remains: Is it the same boat?
Mukherjee raises the Delphic boat in one paragraph at the end of the chapter on stem cells, as a metaphor related to the possibility of stem cell-enabled regeneration in perpetuity. He does not follow any of the threads of potential answers. Given the current state of cellular engineering, about which Mukherjee is a world expert from his work as a physician-scientist, this book could have used an entire section dedicated to probing this question and, importantly, the ways this thought experiment falls apart.
We are entering a phase of real-world bioengineering that features the modularization of cellular parts within cells, of cells within organs, of organs within bodies, and of bodies within ecosystems. In this reality, we would be unwise to assume that any whole is the mere sum of its parts. Wholeness at any one of these scales of life—organelle, cell, organ, body, ecosystem—is what is at stake if we allow biological reductionism to assume away the relation between those scales.
In other words, Mukherjee succeeds in providing a masterful and compelling narrative of the lives of many of the cells that emerge to enliven us. Like his previous books, it is a worthwhile read for anyone curious about the role of cells in disease and in health. And yet, he fails to offer the broader context of The Song of the Cell.
As leading agronomist and essayist Wes Jackson has written, “The sequence of amino acids that is at home in the human cell, when produced inside the bacterial cell, does not fold quite right. Something about the E. coli internal environment affects the tertiary structure of the protein and makes it inactive. The whole in this case, the E. coli cell, affects the part—the newly made protein. Where is the priority of part now?” [1]
Beyond the ways that different kingdoms of life translate the same genetic code, the practical situation for humanity today relates to the ways that the different disciplines of modern life use values and culture to influence our genes, cells, bodies, and environment. It may be that humans will soon become a bit like the Delphic boat, infused with the buzz of fresh cells to repopulate different niches within our bodies, for healthier, longer lives. But in biology, as in writing, a mixed metaphor can cause something of a cacophony. For we are not boats with parts to be replaced piecemeal. And nor are whales, nor alpine forests, nor topsoil. Life isn’t a sum of parts, and neither is a song that rings true.
[1] Wes Jackson, "Visions and Assumptions," in Nature as Measure (p. 52-53).
You won't score many glamor points for using a neti pot, but it could be a worthwhile asset in fighting Covid-19, according to the author's experience and recent research.
Twice a day, morning and night, I use a neti pot to send a warm saltwater solution coursing through one nostril and out the other to flush out debris and pathogens. I started many years ago because of sinus congestion and infections and it has greatly reduced those problems. Along with vaccination when it became available, it seems to have helped with protecting me from developing Covid-19 symptoms despite being of an age and weight that puts me squarely at risk.
Now that supposition of protection has been backed up with evidence from a solidly designed randomized clinical trial. It found that irrigating your sinuses twice a day with a simple saltwater solution can lead to an 8.5-fold reduction in hospitalization from Covid-19. The study is another example of recent research that points to easy and inexpensive ways to help protect yourself and help control the epidemic.
Amy Baxter, the physician researcher behind the study at Augusta University, Medical College of Georgia, began the study in 2020, before a vaccine or monoclonal antibodies became available to counter the virus. She wanted to be able to offer another line of defense for people with limited access to healthcare.
The nasal cavity is the front door that the SARS-CoV-2 virus typically uses to enter the body, latching on to the ACE2 receptors on cells lining those tissue compartments to establish infection. Once the virus replicates here, infection spreads into the lungs and often other parts of the body, including the brain and gut. Some studies have shown that a mouthwash could reduce the viral load, but any effect on disease progression was less clear. Baxter reasoned that reducing the amount of virus in the nose might give the immune system a better chance to react and control that growth before it got out of hand.
She decided to test this approach in patients who had just tested positive for Covid-19, were over 55 years of age, and often had other risk factors for developing serious symptoms. It was the quickest and easiest way to get results. A traditional prevention study would have required many more volunteers, taken a longer period of follow up, and cost money she did not have.
The trial enrolled 79 participants within 24 hours of testing positive for Covid-19, and they agreed to follow the regimen of twice daily nasal irrigation. They were followed for 28 days. One patient was hospitalized; a 1.27% rate compared with 11% in a national sample control group of similar age people who tested positive for Covid-19. Patients who strictly adhered to nasal irrigation had fewer, shorter and less severe symptoms than people in the study who missed some of their saline rinses.
Baxter initially made the results of her clinical trial available as a preprint in the summer of 2021 and was dismayed when many of the comments were from anti-vaxxers who argued this was a reason why you did not need to get vaccinated. That was not her intent.
There are several mechanisms that explain why warm saltwater is so effective. First and most obvious is the physical force of the water that sweeps away debris just as a rainstorm sends trash into a street gutter and down a storm drain. It also lubricates the cilia, small hair-like structures whose job it is to move detritus away from cells for expulsion. Cilia are rich in ACE2 receptors and keeping them moving makes it harder for the virus to latch on to the receptors.
It turns out the saline has a direct effect on the virus itself. SARS-CoV-2 becomes activated when an enzyme called furin snips off part of its molecular structure, which allows the virus to grab on to the ACE2 receptor, but saline inhibits this process. Once inside a cell the virus replicates best in a low salt environment, but nasal cells absorb salt from the irrigation, which further slows viral replication, says Baxter.
Finally, “salt improves the jellification of liquid, it makes better and stickier mucus so that you can get those virus out,” she explains, lamenting, “Nobody cares about snot. I do now.”
She initially made the results of her clinical trial available as a preprint in the summer of 2021 and was dismayed when many of the comments were from anti-vaxxers who argued this was a reason why you did not need to get vaccinated. That was not her intent. Two journals rejected the paper, and Baxter believes getting caught up in the polarizing politics of Covid-19 was an important part of the reason why. She says that editors “didn't want to be associated with something that was being used by anti-vaxxers.” She strongly supports vaccination but realizes that additional and alternative approaches also are needed.
Premeasured packets of saline are inexpensive and can be purchased at any drug store. They are safe to use several times a day. Say you’re vaccinated but were in a situation where you fear you might have been exposed to SARS-CoV-2; an extra irrigation will clear out your sinuses and may reduce the risk of that possible exposure.
Baxter plans no further study in this area. She is returning to her primary research focus, which is pain control and reducing opioid use, but she hopes that others will expand on what she had done.