Why Neglected Tropical Diseases Should Matter to Americans

Kissing bugs can carry a parasite called Trypanosoma cruzi, which causes Chagas disease.
Daisy Hernández was five years old when one of her favorite aunts was struck with a mysterious illness. Tía Dora had stayed behind in Colombia when Daisy's mother immigrated to Union City, New Jersey. A schoolteacher in her late 20s, she began suffering from fevers and abdominal pain, and her belly grew so big that people thought she was pregnant. Exploratory surgery revealed that her large intestine had swollen to ten times its normal size, and she was fitted with a colostomy bag. Doctors couldn't identify the underlying problem—but whatever it was, they said, it would likely kill her within a year or two.
Tía Dora's sisters in New Jersey—Hernández's mother and two other aunts—weren't about to let that happen. They pooled their savings and flew her to New York City, where a doctor at Columbia-Presbyterian Medical Center with a penchant for obscure ailments provided a diagnosis: Chagas disease. Transmitted by the bite of triatomine insects, commonly known as kissing bugs, Chagas is endemic in many parts of Latin America. It's caused by the parasite Trypanoma cruzi, which usually settles in the heart, where it feeds on muscle tissue. In some cases, however, it attacks the intestines or esophagus. Tía Dora belonged to that minority.
In 1980, U.S. immigration laws were more forgiving than they are today. Tía Dora was able to have surgery to remove a part of her colon, despite not being a citizen or having a green card. She eventually married a legal resident and began teaching Spanish at an elementary school. Over the next three decades, she earned a graduate degree, built a career, and was widowed. Meanwhile, Chagas continued its slow devastation. "Every couple of years, we were back in the hospital with her," Hernández recalls. "When I was in high school, she started feeling like she couldn't swallow anything. It was the parasite, destroying the muscles of her esophagus."
When Tía Dora died in 2010, at 59, her niece was among the family members at her bedside. By then, Hernández had become a journalist and fiction writer. Researching a short story about Chagas disease, she discovered that it affected an estimated 6 million people in South America, Central America, and Mexico—as well as 300,000 in the United States, most of whom were immigrants from those places. "I was shocked to learn it wasn't rare," she says. "That made me hungry to know more about this disease, and about the families grappling with it."
Hernández's curiosity led her to write The Kissing Bug, a lyrical hybrid of memoir and science reporting that was published in June. It also led her to another revelation: Chagas is not unique. It's among the many maladies that global health experts refer to as neglected tropical diseases—often-disabling illnesses that afflict 1.7 billion people worldwide, while getting notably less attention than the "big three" of HIV/AIDs, malaria, and tuberculosis. NTDs cause fewer deaths than those plagues, but they wreak untold suffering and economic loss.
Shortly before Hernández's book hit the shelves, the World Health Organization released its 2021-2030 roadmap for fighting NTDs. The plan sets targets for controlling, eliminating, or eradicating all the diseases on the WHO's list, through measures ranging from developing vaccines to improving healthcare infrastructure, sanitation, and access to clean water. Experts agree that for the campaign to succeed, leadership from wealthy nations—particularly the United States—is essential. But given the inward turn of many such countries in recent years (evidenced in movements ranging from America First to Brexit), and the continuing urgency of the COVID-19 crisis, public support is far from guaranteed.
As Hernández writes: "It is easier to forget a disease that cannot be seen." NTDs primarily affect residents of distant lands. They kill only 80,000 people a year, down from 204,000 in 1990. So why should Americans to bother to look?
Breaking the circle of poverty and disease
The World Health Organization counts 20 diseases as NTDs. Along with Chagas, they include dengue and chikungunya, which cause high fevers and agonizing pain; elephantiasis, which deforms victims' limbs and genitals; onchocerciasis, which causes blindness; schistosomiasis, which can damage the heart, lungs, brain, and genitourinary system; helminths such as roundworm and whipworm, which cause anemia, stunted growth, and cognitive disabilities; and a dozen more. Such ailments often co-occur in the same patient, exacerbating each other's effects and those of illnesses such as malaria.
NTDs may be spread by insects, animals, soil, or tainted water; they may be parasitic, bacterial, viral, or—in the case of snakebite envenoming—non-infectious. What they have in common is their longtime neglect by public health agencies and philanthropies. In part, this reflects their typically low mortality rates. But the biggest factor is undoubtedly their disempowered patient populations.
"These diseases occur in the setting of poverty, and they cause poverty, because of their chronic and debilitating effects," observes Peter Hotez, dean of the National School of Tropical Medicine at Baylor University and co-director of the Texas Children's Hospital for Vaccine Development. And historically, the everyday miseries of impoverished people have seldom been a priority for those who set the global health agenda.
That began to change about 20 years ago, when Hotez and others developed the conceptual framework for NTDs and early proposals for combating them. The WHO released its first roadmap in 2012, targeting 17 NTDs for control, elimination, or eradication by 2020. (Rabies, snakebite, and dengue were added later.) Since then, the number of people at risk for NTDs has fallen by 600 million, and 42 countries have eliminated at least one such disease. Cases of dracunculiasis—known as Guinea worm disease, for the parasite that creates painful blisters in a patient's skin—have dropped from the millions to just 27 in 2020.
Yet the battle is not over, and the COVID-19 pandemic has disrupted prevention and treatment programs around the globe.
A new direction — and longstanding obstacles
The WHO's new roadmap sets even more ambitious goals for 2030. Among them: reducing by 90 percent the number of people requiring treatment for NTDs; eliminating at least one NTD in another 100 countries; and fully eradicating dracunculiasis and yaws, a disfiguring skin infection.
The plan also places an increased focus on "country ownership," relying on nations with high incidence of NTDs to design their own plans based on local expertise. "I was so excited to see that," says Kristina Talbert-Slagle, director of the Yale College Global Health Studies program. "No one is a better expert on how to address these situations than the people who deal with it day by day."
Another fresh approach is what the roadmap calls "cross-cutting" targets. "One of the really cool things about the plan is how much it emphasizes coordination among different sectors of the health system," says Claire Standley, a faculty member at Georgetown University's Center for Global Health Science and Security. "For example, it explicitly takes into account the zoonotic nature of many neglected tropical diseases—the fact that we have to think about animal health as well as human health when we tackle NTDs."
Whether this grand vision can be realized, however, will depend largely on funding—and that, in turn, is a question of political will in the countries most able to provide it. On the upside, the U.S. has ended its Trump-era feud with the WHO. "One thing that's been really encouraging," says Standley, "has been the strong commitment toward global cooperation from the current administration." Even under the previous president, the U.S. remained the single largest contributor to the global health kitty, spending over $100 million annually on NTDs—six times the figure in 2006, when such financing started.
On the downside, America's outlay has remained flat for several years, and the Biden administration has so far not moved to increase it. A "back-of-the-envelope calculation," says Hotez, suggests that the current level of aid could buy medications for the most common NTDs for about 200 million people a year. But the number of people who need treatment, he notes, is at least 750 million.
Up to now, the United Kingdom—long the world's second-most generous health aid donor—has taken up a large portion of the slack. But the UK last month announced deep cuts in its portfolio, eliminating 102 previously supported countries and leaving only 34. "That really concerns me," Hotez says.
The struggle for funds, he notes, is always harder for projects involving NTDs than for those aimed at higher-profile diseases. His lab, which he co-directs with microbiologist Maria Elena Bottazzi, started developing a COVID-19 vaccine soon after the pandemic struck, for example, and is now in Phase 3 trials. The team has been working on vaccines for Chagas, hookworm, and schistosomiasis for much longer, but trials for those potential game-changers lag behind. "We struggle to get the level of resources needed to move quickly," Hotez explains.
Two million reasons to care
One way to prompt a government to open its pocketbook is for voters to clamor for action. A longtime challenge with NTDs, however, has been getting people outside the hardest-hit countries to pay attention.
The reasons to care, global health experts argue, go beyond compassion. "When we have high NTD burden," says Talbert-Slagle, "it can prevent economic growth, prevent innovation, lead to more political instability." That, in turn, can lead to wars and mass migration, affecting economic and political events far beyond an affected country's borders.
Like Hernández's aunt Dora, many people driven out of NTD-wracked regions wind up living elsewhere. And that points to another reason to care about these diseases: Some of your neighbors might have them. In the U.S., up to 14 million people suffer from neglected parasitic infections—including 70,000 with Chagas in California alone.
When Hernández was researching The Kissing Bug, she worried that such statistics would provide ammunition to racists and xenophobes who claim that immigrants "bring disease" or exploit overburdened healthcare systems. (This may help explain some of the stigma around NTDs, which led Tía Dora to hide her condition from most people outside her family.) But as the book makes clear, these infections know no borders; they flourish wherever large numbers of people lack access to resources that most residents of rich countries take for granted.
Indeed, far from gaming U.S. healthcare systems, millions of low-income immigrants can't access them—or must wait until they're sick enough to go to an emergency room. Since Congress changed the rules in 1996, green card holders have to wait five years before they can enroll in Medicaid. Undocumented immigrants can never qualify.
Closing the great divide
Hernández uses a phrase borrowed from global health crusader Paul Farmer to describe this access gap: "the great epi divide." On one side, she explains, "people will die from cancer, from diabetes, from chronic illnesses later in life. On the other side of the epidemiological divide, people are dying because they can't get to the doctor, or they can't get medication. They don't have a hospital anywhere near them. When I read Dr. Farmer's work, I realized how much that applied to neglected diseases as well."
When it comes to Chagas disease, she says, the epi divide is embodied in the lack of a federal mandate for prenatal or newborn screening. Each year, according to the Centers for Disease Control and Prevention, up to 300 babies in the U.S. are born with Chagas, which can be passed from the mother in utero. The disease can be cured with medication if treated in infancy. (It can also be cured in adults in the acute stage, but is seldom detected in time.) Yet the CDC does not require screening for Chagas—even though newborns are tested for 15 diseases that are less common. According to one study, it would be 10 times cheaper to screen and treat babies and their mothers than to cover the costs related to the illness in later years. Few states make the effort.
The gap that enables NTDs to persist, Hernández argues, is the same one that has led to COVID-19 death rates in Black and Latinx communities that are double those elsewhere in America. To close it, she suggests, caring is not enough.
"When I was working on my book," she says, "I thought about HIV in the '80s, when it had so much stigma that no one wanted to talk about it. Then activists stepped up and changed the conversation. I thought a lot about breast cancer, which was stigmatized for years, until people stepped forward and started speaking out. I thought about Lyme disease. And it wasn't only patients—it was also allies, right? The same thing needs to happen with neglected diseases around the world. Allies need to step up and make demands on policymakers. We need to make some noise."
New tech for prison reform spreads to 11 states
The U.S. has the highest incarceration rate in the world, costing $182 billion per year, partly because its antiquated data systems often fail to identify people who should be released. A tech nonprofit is trying to change that.
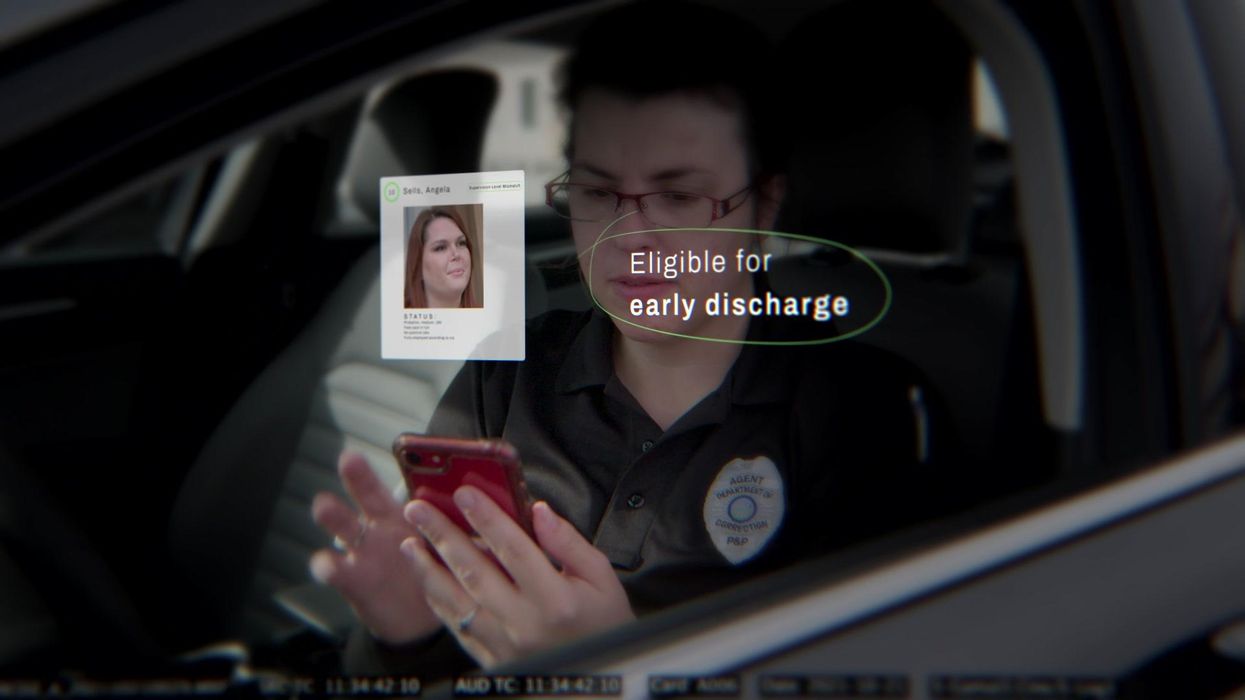
A new non-profit called Recidiviz is using data technology to reduce the size of the U.S. criminal justice system. The bi-coastal company (SF and NYC) is currently working with 11 states to improve their systems and, so far, has helped remove nearly 69,000 people — ones left floundering in jail or on parole when they should have been released.
“The root cause is fragmentation,” says Clementine Jacoby, 31, a software engineer who worked at Google before co-founding Recidiviz in 2019. In the 1970s and 80s, the U.S. built a series of disconnected data systems, and this patchwork is still being used by criminal justice authorities today. It requires parole officers to manually calculate release dates, leading to errors in many cases. “[They] have done everything they need to do to earn their release, but they're still stuck in the system,” Jacoby says.
Recidiviz has built a platform that connects the different databases, with the goal of identifying people who are already qualified for release but remain behind bars or on supervision. “Think of Recidiviz like Google Maps,” says Jacoby, who worked on Maps when she was at the tech giant. Google Maps takes in data from different sources – satellite images, street maps, local business data — and organizes it into one easy view. “Recidiviz does something similar with criminal justice data,” Jacoby explains, “making it easy to identify people eligible to come home or to move to less intensive levels of supervision.”
People like Jacoby’s uncle. His experience with incarceration is what inspired her passion for criminal justice reform in the first place.
The problems are vast
The U.S. has the highest incarceration rate in the world — 2 million people according to the watchdog group, Prison Policy Initiative — at a cost of $182 billion a year. The numbers could be a lot lower if not for an array of problems including inaccurate sentencing calculations, flawed algorithms and parole violations laws.
Sentencing miscalculations
To determine eligibility for release, the current system requires corrections officers to check 21 different requirements spread across five different databases for each of the 90 to 100 people under their supervision. These manual calculations are time prohibitive, says Jacoby, and fall victim to human error.
In addition, Recidiviz found that policies aimed at helping to reduce the prison population don’t always work correctly. A key example is time off for good behavior laws that allow inmates to earn one day off for every 30 days of good behavior. Some states' data systems are built to calculate time off as one day per month of good behavior, rather than per day. Over the course of a decade-long sentence, Jacoby says these miscalculations can lead to a huge discrepancy in the calculated release data and the actual release date.
Algorithms
Commercial algorithm-based software systems for risk assessment continue to be widely used in the criminal justice system, even though a 2018 study published in Science Advances exposed their limitations. After the study went viral, it took three years for the Justice Department to issue a report on their own flawed algorithms used to reduce the federal prison population as part of the 2018 First Step Act. The program, it was determined, overestimated the risk of putting inmates of color into early-release programs.
Despite its name, Recidiviz does not build these types of algorithms for predicting recidivism, or whether someone will commit another crime after being released from prison. Rather, Jacoby says the company’s "descriptive analytics” approach is specifically intended to weed out incarceration inequalities and avoid algorithmic pitfalls.
Parole violation laws
Research shows that 350,000 people a year — about a quarter of the total prison population — are sent back not because they’ve committed another crime, but because they’ve broken a specific rule of their probation. “Things that wouldn't send you or I to prison, but would send someone on parole,” such as crossing county lines or being in the presence of alcohol when they shouldn’t be, are inflating the prison population, says Jacoby.
It’s personal for the co-founder and CEO
“I grew up with an uncle who went into the prison system,” Jacoby says. At 19, he was sentenced to ten years in prison for a non-violent crime. A few months after being released from jail, he was sent back for a non-violent parole violation.
“For my family, the fact that one in four prison admissions are driven not by a crime but by someone who's broken a rule on probation and parole was really profound because that happened to my uncle,” Jacoby says. The experience led her to begin studying criminal justice in high school, then college. She continued her dive into how the criminal justice system works as part of her Passion Project while at Google, a program that allows employees to spend 20 percent of their time on pro-bono work. Two colleagues whose family members had also been stuck in the system joined her.
As part of the project, Jacoby interviewed hundreds of people involved in the criminal justice system. “Those on the right, those on the left, agreed that bad data was slowing down reform,” she says. Their research brought them to North Dakota where they began to understand the root of the problem. The corrections department is making “huge, consequential decisions every day [without] … the data,” Jacoby says. In a new video by Recidiviz not yet released, Jacoby recounts her exchange with the state’s director of corrections who told her, “‘It’s not that we have the data and we just don’t know how to make it public; we don’t have the information you think we have.'"
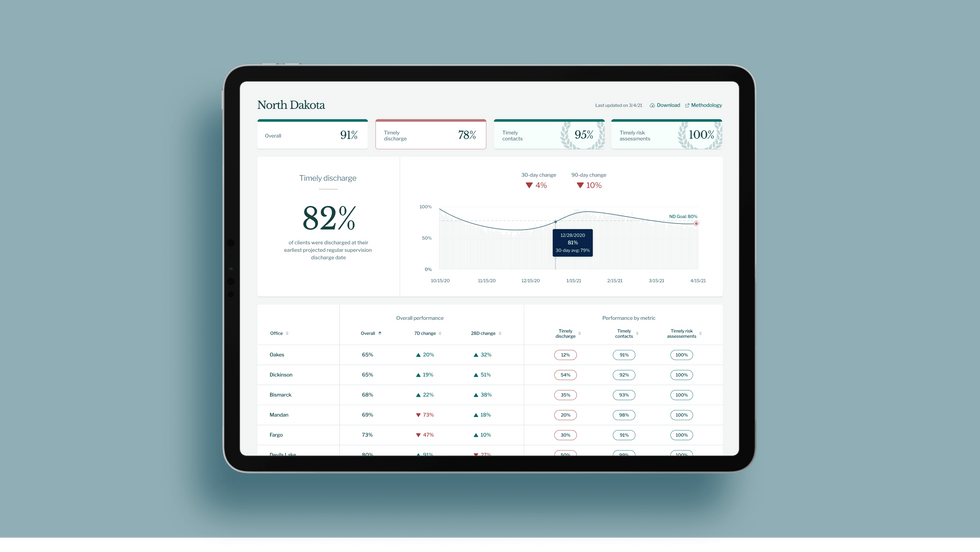
A mock-up (with fake data) of the types of dashboards and insights that Recidiviz provides to state governments.
Recidiviz
As a software engineer, Jacoby says the comment made no sense to her — until she witnessed it first-hand. “We spent a lot of time driving around in cars with corrections directors and parole officers watching them use these incredibly taxing, frankly terrible, old data systems,” Jacoby says.
As they weeded through thousands of files — some computerized, some on paper — they unearthed the consequences of bad data: Hundreds of people in prison well past their release date and thousands more whose release from parole was delayed because of minor paperwork issues. They found individuals stuck in parole because they hadn’t checked one last item off their eligibility list — like simply failing to provide their parole officer with a paystub. And, even when parolees advocated for themselves, the archaic system made it difficult for their parole officers to confirm their eligibility, so they remained in the system. Jacoby and her team also unpacked specific policies that drive racial disparities — such as fines and fees.
The Solution
It’s more than a trivial technical challenge to bring the incomplete, fragmented data onto a 21st century data platform. It takes months for Recidiviz to sift through a state’s information systems to connect databases “with the goal of tracking a person all the way through their journey and find out what’s working for 18- to 25-year-old men, what’s working for new mothers,” explains Jacoby in the video.
TED Talk: How bad data traps people in the U.S. justice system

TED Fellow Clementine Jacoby's TED Talk went live on Jan. 13. It describes how we can fix bad data in the criminal justice system, "bringing thousands of people home, reducing costs and improving public safety along the way."
Clementine Jacoby • TED2022
Ojmarrh Mitchell, an associate professor in the School of Criminology and Criminal Justice at Arizona State University, who is not involved with the company, says what Recidiviz is doing is “remarkable.” His perspective goes beyond academic analysis. In his pre-academic years, Mitchell was a probation officer, working within the framework of the “well known, but invisible” information sharing issues that plague criminal justice departments. The flexibility of Recidiviz’s approach is what makes it especially innovative, he says. “They identify the specific gaps in each jurisdiction and tailor a solution for that jurisdiction.”
On the downside, the process used by Recidiviz is “a bit opaque,” Mitchell says, with few details available on how Recidiviz designs its tools and tracks outcomes. By sharing more information about how its actions lead to progress in a given jurisdiction, Recidiviz could help reformers in other places figure out which programs have the best potential to work well.
The eleven states in which Recidiviz is working include California, Colorado, Maine, Michigan, Missouri, Pennsylvania and Tennessee. And a pilot program launched last year in Idaho, if scaled nationally, with could reduce the number of people in the criminal justice system by a quarter of a million people, Jacoby says. As part of the pilot, rather than relying on manual calculations, Recidiviz is equipping leaders and the probation officers with actionable information with a few clicks of an app that Recidiviz built.
Mitchell is disappointed that there’s even the need for Recidiviz. “This is a problem that government agencies have a responsibility to address,” he says. “But they haven’t.” For one company to come along and fill such a large gap is “remarkable.”
How Leqembi became the biggest news in Alzheimer’s disease in 40 years, and what comes next
Betsy Groves, 73, with her granddaughter. Groves learned in 2021 that she has Alzheimer's disease. She hopes to take Leqembi, a drug approved by the FDA last week.
A few months ago, Betsy Groves traveled less than a mile from her home in Cambridge, Mass. to give a talk to a bunch of scientists. The scientists, who worked for the pharmaceutical companies Biogen and Eisai, wanted to know how she lived her life, how she thought about her future, and what it was like when a doctor’s appointment in 2021 gave her the worst possible news. Groves, 73, has Alzheimer’s disease. She caught it early, through a lumbar puncture that showed evidence of amyloid, an Alzheimer’s hallmark, in her cerebrospinal fluid. As a way of dealing with her diagnosis, she joined the Alzheimer’s Association’s National Early-Stage Advisory Board, which helped her shift into seeing her diagnosis as something she could use to help others.
After her talk, Groves stayed for lunch with the scientists, who were eager to put a face to their work. Biogen and Eisai were about to release the first drug to successfully combat Alzheimer’s in 40 years of experimental disaster. Their drug, which is known by the scientific name lecanemab and the marketing name Leqembi, was granted accelerated approval by the U.S. Food and Drug Administration last Friday, Jan. 6, after a study in 1,800 people showed that it reduced cognitive decline by 27 percent over 18 months.
It is no exaggeration to say that this result is a huge deal. The field of Alzheimer’s drug development has been absolutely littered with failures. Almost everything researchers have tried has tanked in clinical trials. “Most of the things that we've done have proven not to be effective, and it's not because we haven’t been taking a ton of shots at goal,” says Anton Porsteinsson, director of the University of Rochester Alzheimer's Disease Care, Research, and Education Program, who worked on the lecanemab trial. “I think it's fair to say you don't survive in this field unless you're an eternal optimist.”
As far back as 1984, a cure looked like it was within reach: Scientists discovered that the sticky plaques that develop in the brains of those who have Alzheimer’s are made up of a protein fragment called beta-amyloid. Buildup of beta-amyloid seemed to be sufficient to disrupt communication between, and eventually kill, memory cells. If that was true, then the cure should be straightforward: Stop the buildup of beta-amyloid; stop the Alzheimer’s disease.
It wasn’t so simple. Over the next 38 years, hundreds of drugs designed either to interfere with the production of abnormal amyloid or to clear it from the brain flamed out in trials. It got so bad that neuroscience drug divisions at major pharmaceutical companies (AstraZeneca, Pfizer, Bristol-Myers, GSK, Amgen) closed one by one, leaving the field to smaller, scrappier companies, like Cambridge-based Biogen and Tokyo-based Eisai. Some scientists began to dismiss the amyloid hypothesis altogether: If this protein fragment was so important to the disease, why didn’t ridding the brain of it do anything for patients? There was another abnormal protein that showed up in the brains of Alzheimer’s patients, called tau. Some researchers defected to the tau camp, or came to believe the proteins caused damage in combination.
The situation came to a head in 2021, when the FDA granted provisional approval to a drug called aducanumab, marketed as Aduhelm, against the advice of its own advisory council. The approval was based on proof that Aduhelm reduced beta-amyloid in the brain, even though one research trial showed it had no effect on people’s symptoms or daily life. Aduhelm could also cause serious side effects, like brain swelling and amyloid related imaging abnormalities (known as ARIA, these are basically micro-bleeds that appear on MRI scans). Without a clear benefit to memory loss that would make these risks worth it, Medicare refused to pay for Aduhelm among the general population. Two congressional committees launched an investigation into the drug’s approval, citing corporate greed, lapses in protocol, and an unjustifiably high price. (Aduhelm was also produced by the pharmaceutical company Biogen.)
To be clear, Leqembi is not the cure Alzheimer’s researchers hope for. While the drug is the first to show clear signs of a clinical benefit, the scientific establishment is split on how much of a difference Leqembi will make in the real world.
So far, Leqembi is like Aduhelm in that it has been given accelerated approval only for its ability to remove amyloid from the brain. Both are monoclonal antibodies that direct the immune system to attack and clear dysfunctional beta-amyloid. The difference is that, while that’s all Aduhelm was ever shown to do, Leqembi’s makers have already asked the FDA to give it full approval – a decision that would increase the likelihood that Medicare will cover it – based on data that show it also improves Alzheimer’s sufferer’s lives. Leqembi targets a different type of amyloid, a soluble version called “protofibrils,” and that appears to change the effect. “It can give individuals and their families three, six months longer to be participating in daily life and living independently,” says Claire Sexton, PhD, senior director of scientific programs & outreach for the Alzheimer's Association. “These types of changes matter for individuals and for their families.”
To be clear, Leqembi is not the cure Alzheimer’s researchers hope for. It does not halt or reverse the disease, and people do not get better. While the drug is the first to show clear signs of a clinical benefit, the scientific establishment is split on how much of a difference Leqembi will make in the real world. It has “a rather small effect,” wrote NIH Alzheimer’s researcher Madhav Thambisetty, MD, PhD, in an email to Leaps.org. “It is unclear how meaningful this difference will be to patients, and it is unlikely that this level of difference will be obvious to a patient (or their caregivers).” Another issue is cost: Leqembi will become available to patients later this month, but Eisai is setting the price at $26,500 per year, meaning that very few patients will be able to afford it unless Medicare chooses to reimburse them for it.
The same side effects that plagued Aduhelm are common in Leqembi treatment as well. In many patients, amyloid doesn’t just accumulate around neurons, it also forms deposits in the walls of blood vessels. Blood vessels that are shot through with amyloid are more brittle. If you infuse a drug that targets amyloid, brittle blood vessels in the brain can develop leakage that results in swelling or bleeds. Most of these come with no symptoms, and are only seen during testing, which is why they are called “imaging abnormalities.” But in situations where patients have multiple diseases or are prescribed incompatible drugs, they can be serious enough to cause death. The three deaths reported from Leqembi treatment (so far) are enough to make Thambisetty wonder “how well the drug may be tolerated in real world clinical practice where patients are likely to be sicker and have multiple other medical conditions in contrast to carefully selected patients in clinical trials.”
Porsteinsson believes that earlier detection of Alzheimer’s disease will be the next great advance in treatment, a more important step forward than Leqembi’s approval.
Still, there are reasons to be excited. A successful Alzheimer’s drug can pave the way for combination studies, in which patients try a known effective drug alongside newer, more experimental ones; or preventative studies, which take place years before symptoms occur. It also represents enormous strides in researchers’ understanding of the disease. For example, drug dosages have increased massively—in some cases quadrupling—from the early days of Alzheimer’s research. And patient selection for studies has changed drastically as well. Doctors now know that you’ve got to catch the disease early, through PET-scans or CSF tests for amyloid, if you want any chance of changing its course.
Porsteinsson believes that earlier detection of Alzheimer’s disease will be the next great advance in treatment, a more important step forward than Leqembi’s approval. His lab already uses blood tests for different types of amyloid, for different types of tau, and for measures of neuroinflammation, neural damage, and synaptic health, but commercially available versions from companies like C2N, Quest, and Fuji Rebio are likely to hit the market in the next couple of years. “[They are] going to transform the diagnosis of Alzheimer's disease,” Porsteinsson says. “If someone is experiencing memory problems, their physicians will be able to order a blood test that will tell us if this is the result of changes in your brain due to Alzheimer's disease. It will ultimately make it much easier to identify people at a very early stage of the disease, where they are most likely to benefit from treatment.”
Learn more about new blood tests to detect Alzheimer's
Early detection can help patients for more philosophical reasons as well. Betsy Groves credits finding her Alzheimer’s early with giving her the space to understand and process the changes that were happening to her before they got so bad that she couldn’t. She has been able to update her legal documents and, through her role on the Advisory Group, help the Alzheimer’s Association with developing its programs and support services for people in the early stages of the disease. She still drives, and because she and her husband love to travel, they are hoping to get out of grey, rainy Cambridge and off to Texas or Arizona this spring.
Because her Alzheimer’s disease involves amyloid deposits (a “substantial portion” do not, says Claire Sexton, which is an additional complication for research), and has not yet reached an advanced stage, Groves may be a good candidate to try Leqembi. She says she’d welcome the opportunity to take it. If she can get access, Groves hopes the drug will give her more days to be fully functioning with her husband, daughters, and three grandchildren. Mostly, she avoids thinking about what the latter stages of Alzheimer’s might be like, but she knows the time will come when it will be her reality. “So whatever lecanemab can do to extend my more productive ways of engaging with relationships in the world,” she says. “I'll take that in a minute.”