Why Neglected Tropical Diseases Should Matter to Americans

Kissing bugs can carry a parasite called Trypanosoma cruzi, which causes Chagas disease.
Daisy Hernández was five years old when one of her favorite aunts was struck with a mysterious illness. Tía Dora had stayed behind in Colombia when Daisy's mother immigrated to Union City, New Jersey. A schoolteacher in her late 20s, she began suffering from fevers and abdominal pain, and her belly grew so big that people thought she was pregnant. Exploratory surgery revealed that her large intestine had swollen to ten times its normal size, and she was fitted with a colostomy bag. Doctors couldn't identify the underlying problem—but whatever it was, they said, it would likely kill her within a year or two.
Tía Dora's sisters in New Jersey—Hernández's mother and two other aunts—weren't about to let that happen. They pooled their savings and flew her to New York City, where a doctor at Columbia-Presbyterian Medical Center with a penchant for obscure ailments provided a diagnosis: Chagas disease. Transmitted by the bite of triatomine insects, commonly known as kissing bugs, Chagas is endemic in many parts of Latin America. It's caused by the parasite Trypanoma cruzi, which usually settles in the heart, where it feeds on muscle tissue. In some cases, however, it attacks the intestines or esophagus. Tía Dora belonged to that minority.
In 1980, U.S. immigration laws were more forgiving than they are today. Tía Dora was able to have surgery to remove a part of her colon, despite not being a citizen or having a green card. She eventually married a legal resident and began teaching Spanish at an elementary school. Over the next three decades, she earned a graduate degree, built a career, and was widowed. Meanwhile, Chagas continued its slow devastation. "Every couple of years, we were back in the hospital with her," Hernández recalls. "When I was in high school, she started feeling like she couldn't swallow anything. It was the parasite, destroying the muscles of her esophagus."
When Tía Dora died in 2010, at 59, her niece was among the family members at her bedside. By then, Hernández had become a journalist and fiction writer. Researching a short story about Chagas disease, she discovered that it affected an estimated 6 million people in South America, Central America, and Mexico—as well as 300,000 in the United States, most of whom were immigrants from those places. "I was shocked to learn it wasn't rare," she says. "That made me hungry to know more about this disease, and about the families grappling with it."
Hernández's curiosity led her to write The Kissing Bug, a lyrical hybrid of memoir and science reporting that was published in June. It also led her to another revelation: Chagas is not unique. It's among the many maladies that global health experts refer to as neglected tropical diseases—often-disabling illnesses that afflict 1.7 billion people worldwide, while getting notably less attention than the "big three" of HIV/AIDs, malaria, and tuberculosis. NTDs cause fewer deaths than those plagues, but they wreak untold suffering and economic loss.
Shortly before Hernández's book hit the shelves, the World Health Organization released its 2021-2030 roadmap for fighting NTDs. The plan sets targets for controlling, eliminating, or eradicating all the diseases on the WHO's list, through measures ranging from developing vaccines to improving healthcare infrastructure, sanitation, and access to clean water. Experts agree that for the campaign to succeed, leadership from wealthy nations—particularly the United States—is essential. But given the inward turn of many such countries in recent years (evidenced in movements ranging from America First to Brexit), and the continuing urgency of the COVID-19 crisis, public support is far from guaranteed.
As Hernández writes: "It is easier to forget a disease that cannot be seen." NTDs primarily affect residents of distant lands. They kill only 80,000 people a year, down from 204,000 in 1990. So why should Americans to bother to look?
Breaking the circle of poverty and disease
The World Health Organization counts 20 diseases as NTDs. Along with Chagas, they include dengue and chikungunya, which cause high fevers and agonizing pain; elephantiasis, which deforms victims' limbs and genitals; onchocerciasis, which causes blindness; schistosomiasis, which can damage the heart, lungs, brain, and genitourinary system; helminths such as roundworm and whipworm, which cause anemia, stunted growth, and cognitive disabilities; and a dozen more. Such ailments often co-occur in the same patient, exacerbating each other's effects and those of illnesses such as malaria.
NTDs may be spread by insects, animals, soil, or tainted water; they may be parasitic, bacterial, viral, or—in the case of snakebite envenoming—non-infectious. What they have in common is their longtime neglect by public health agencies and philanthropies. In part, this reflects their typically low mortality rates. But the biggest factor is undoubtedly their disempowered patient populations.
"These diseases occur in the setting of poverty, and they cause poverty, because of their chronic and debilitating effects," observes Peter Hotez, dean of the National School of Tropical Medicine at Baylor University and co-director of the Texas Children's Hospital for Vaccine Development. And historically, the everyday miseries of impoverished people have seldom been a priority for those who set the global health agenda.
That began to change about 20 years ago, when Hotez and others developed the conceptual framework for NTDs and early proposals for combating them. The WHO released its first roadmap in 2012, targeting 17 NTDs for control, elimination, or eradication by 2020. (Rabies, snakebite, and dengue were added later.) Since then, the number of people at risk for NTDs has fallen by 600 million, and 42 countries have eliminated at least one such disease. Cases of dracunculiasis—known as Guinea worm disease, for the parasite that creates painful blisters in a patient's skin—have dropped from the millions to just 27 in 2020.
Yet the battle is not over, and the COVID-19 pandemic has disrupted prevention and treatment programs around the globe.
A new direction — and longstanding obstacles
The WHO's new roadmap sets even more ambitious goals for 2030. Among them: reducing by 90 percent the number of people requiring treatment for NTDs; eliminating at least one NTD in another 100 countries; and fully eradicating dracunculiasis and yaws, a disfiguring skin infection.
The plan also places an increased focus on "country ownership," relying on nations with high incidence of NTDs to design their own plans based on local expertise. "I was so excited to see that," says Kristina Talbert-Slagle, director of the Yale College Global Health Studies program. "No one is a better expert on how to address these situations than the people who deal with it day by day."
Another fresh approach is what the roadmap calls "cross-cutting" targets. "One of the really cool things about the plan is how much it emphasizes coordination among different sectors of the health system," says Claire Standley, a faculty member at Georgetown University's Center for Global Health Science and Security. "For example, it explicitly takes into account the zoonotic nature of many neglected tropical diseases—the fact that we have to think about animal health as well as human health when we tackle NTDs."
Whether this grand vision can be realized, however, will depend largely on funding—and that, in turn, is a question of political will in the countries most able to provide it. On the upside, the U.S. has ended its Trump-era feud with the WHO. "One thing that's been really encouraging," says Standley, "has been the strong commitment toward global cooperation from the current administration." Even under the previous president, the U.S. remained the single largest contributor to the global health kitty, spending over $100 million annually on NTDs—six times the figure in 2006, when such financing started.
On the downside, America's outlay has remained flat for several years, and the Biden administration has so far not moved to increase it. A "back-of-the-envelope calculation," says Hotez, suggests that the current level of aid could buy medications for the most common NTDs for about 200 million people a year. But the number of people who need treatment, he notes, is at least 750 million.
Up to now, the United Kingdom—long the world's second-most generous health aid donor—has taken up a large portion of the slack. But the UK last month announced deep cuts in its portfolio, eliminating 102 previously supported countries and leaving only 34. "That really concerns me," Hotez says.
The struggle for funds, he notes, is always harder for projects involving NTDs than for those aimed at higher-profile diseases. His lab, which he co-directs with microbiologist Maria Elena Bottazzi, started developing a COVID-19 vaccine soon after the pandemic struck, for example, and is now in Phase 3 trials. The team has been working on vaccines for Chagas, hookworm, and schistosomiasis for much longer, but trials for those potential game-changers lag behind. "We struggle to get the level of resources needed to move quickly," Hotez explains.
Two million reasons to care
One way to prompt a government to open its pocketbook is for voters to clamor for action. A longtime challenge with NTDs, however, has been getting people outside the hardest-hit countries to pay attention.
The reasons to care, global health experts argue, go beyond compassion. "When we have high NTD burden," says Talbert-Slagle, "it can prevent economic growth, prevent innovation, lead to more political instability." That, in turn, can lead to wars and mass migration, affecting economic and political events far beyond an affected country's borders.
Like Hernández's aunt Dora, many people driven out of NTD-wracked regions wind up living elsewhere. And that points to another reason to care about these diseases: Some of your neighbors might have them. In the U.S., up to 14 million people suffer from neglected parasitic infections—including 70,000 with Chagas in California alone.
When Hernández was researching The Kissing Bug, she worried that such statistics would provide ammunition to racists and xenophobes who claim that immigrants "bring disease" or exploit overburdened healthcare systems. (This may help explain some of the stigma around NTDs, which led Tía Dora to hide her condition from most people outside her family.) But as the book makes clear, these infections know no borders; they flourish wherever large numbers of people lack access to resources that most residents of rich countries take for granted.
Indeed, far from gaming U.S. healthcare systems, millions of low-income immigrants can't access them—or must wait until they're sick enough to go to an emergency room. Since Congress changed the rules in 1996, green card holders have to wait five years before they can enroll in Medicaid. Undocumented immigrants can never qualify.
Closing the great divide
Hernández uses a phrase borrowed from global health crusader Paul Farmer to describe this access gap: "the great epi divide." On one side, she explains, "people will die from cancer, from diabetes, from chronic illnesses later in life. On the other side of the epidemiological divide, people are dying because they can't get to the doctor, or they can't get medication. They don't have a hospital anywhere near them. When I read Dr. Farmer's work, I realized how much that applied to neglected diseases as well."
When it comes to Chagas disease, she says, the epi divide is embodied in the lack of a federal mandate for prenatal or newborn screening. Each year, according to the Centers for Disease Control and Prevention, up to 300 babies in the U.S. are born with Chagas, which can be passed from the mother in utero. The disease can be cured with medication if treated in infancy. (It can also be cured in adults in the acute stage, but is seldom detected in time.) Yet the CDC does not require screening for Chagas—even though newborns are tested for 15 diseases that are less common. According to one study, it would be 10 times cheaper to screen and treat babies and their mothers than to cover the costs related to the illness in later years. Few states make the effort.
The gap that enables NTDs to persist, Hernández argues, is the same one that has led to COVID-19 death rates in Black and Latinx communities that are double those elsewhere in America. To close it, she suggests, caring is not enough.
"When I was working on my book," she says, "I thought about HIV in the '80s, when it had so much stigma that no one wanted to talk about it. Then activists stepped up and changed the conversation. I thought a lot about breast cancer, which was stigmatized for years, until people stepped forward and started speaking out. I thought about Lyme disease. And it wasn't only patients—it was also allies, right? The same thing needs to happen with neglected diseases around the world. Allies need to step up and make demands on policymakers. We need to make some noise."
The U.S. must fund more biotech innovation – or other countries will catch up faster than you think
In the coming years, U.S. market share in biotech will decline unless the federal government makes investments to improve the quality and quantity of U.S. research, writes the author.
The U.S. has approximately 58 percent of the market share in the biotech sector, followed by China with 11 percent. However, this market share is the result of several years of previous research and development (R&D) – it is a present picture of what happened in the past. In the future, this market share will decline unless the federal government makes investments to improve the quality and quantity of U.S. research in biotech.
The effectiveness of current R&D can be evaluated in a variety of ways such as monies invested and the number of patents filed. According to the UNESCO Institute for Statistics, the U.S. spends approximately 2.7 percent of GDP on R&D ($476,459.0M), whereas China spends 2 percent ($346,266.3M). However, investment levels do not necessarily translate into goods that end up contributing to innovation.
Patents are a better indication of innovation. The biotech industry relies on patents to protect their investments, making patenting a key tool in the process of translating scientific discoveries that can ultimately benefit patients. In 2020, China filed 1,497,159 patents, a 6.9 percent increase in growth rate. In contrast, the U.S. filed 597,172, a 3.9 percent decline. When it comes to patents filed, China has approximately 45 percent of the world share compared to 18 percent for the U.S.
So how did we get here? The nature of science in academia allows scientists to specialize by dedicating several years to advance discovery research and develop new inventions that can then be licensed by biotech companies. This makes academic science critical to innovation in the U.S. and abroad.
Academic scientists rely on government and foundation grants to pay for R&D, which includes salaries for faculty, investigators and trainees, as well as monies for infrastructure, support personnel and research supplies. Of particular interest to academic scientists to cover these costs is government support such as Research Project Grants, also known as R01 grants, the oldest grant mechanism from the National Institutes of Health. Unfortunately, this funding mechanism is extremely competitive, as applications have a success rate of only about 20 percent. To maximize the chances of getting funded, investigators tend to limit the innovation of their applications, since a project that seems overambitious is discouraged by grant reviewers.
Considering the difficulty in obtaining funding, the limited number of opportunities for scientists to become independent investigators capable of leading their own scientific projects, and the salaries available to pay for scientists with a doctoral degree, it is not surprising that the U.S. is progressively losing its workforce for innovation.
This approach affects the future success of the R&D enterprise in the U.S. Pursuing less innovative work tends to produce scientific results that are more obvious than groundbreaking, and when a discovery is obvious, it cannot be patented, resulting in fewer inventions that go on to benefit patients. Even though there are governmental funding options available for scientists in academia focused on more groundbreaking and translational projects, those options are less coveted by academic scientists who are trying to obtain tenure and long-term funding to cover salaries and other associated laboratory expenses. Therefore, since only a small percent of projects gets funded, the likelihood of scientists interested in pursuing academic science or even research in general keeps declining over time.
Efforts to raise the number of individuals who pursue a scientific education are paying off. However, the number of job openings for those trainees to carry out independent scientific research once they graduate has proved harder to increase. These limitations are not just in the number of faculty openings to pursue academic science, which are in part related to grant funding, but also the low salary available to pay those scientists after they obtain their doctoral degree, which ranges from $53,000 to $65,000, depending on years of experience.
Thus, considering the difficulty in obtaining funding, the limited number of opportunities for scientists to become independent investigators capable of leading their own scientific projects, and the salaries available to pay for scientists with a doctoral degree, it is not surprising that the U.S. is progressively losing its workforce for innovation, which results in fewer patents filed.
Perhaps instead of encouraging scientists to propose less innovative projects in order to increase their chances of getting grants, the U.S. government should give serious consideration to funding investigators for their potential for success -- or the success they have already achieved in contributing to the advancement of science. Such a funding approach should be tiered depending on career stage or years of experience, considering that 42 years old is the median age at which the first R01 is obtained. This suggests that after finishing their training, scientists spend 10 years before they establish themselves as independent academic investigators capable of having the appropriate funds to train the next generation of scientists who will help the U.S. maintain or even expand its market share in the biotech industry for years to come. Patenting should be given more weight as part of the academic endeavor for promotion purposes, or governmental investment in research funding should be increased to support more than just 20 percent of projects.
Remaining at the forefront of biotech innovation will give us the opportunity to not just generate more jobs, but it will also allow us to attract the brightest scientists from all over the world. This talented workforce will go on to train future U.S. scientists and will improve our standard of living by giving us the opportunity to produce the next generation of therapies intended to improve human health.
This problem cannot rely on just one solution, but what is certain is that unless there are more creative changes in funding approaches for scientists in academia, eventually we may be saying “remember when the U.S. was at the forefront of biotech innovation?”
New gene therapy helps patients with rare disease. One mother wouldn't have it any other way.
A biotech in Cambridge, Mass., is targeting a rare disease called cystinosis with gene therapy. It's been effective for five patients in a clinical trial that's still underway.
Three years ago, Jordan Janz of Consort, Alberta, knew his gene therapy treatment for cystinosis was working when his hair started to darken. Pigmentation or melanin production is just one part of the body damaged by cystinosis.
“When you have cystinosis, you’re either a redhead or a blonde, and you are very pale,” attests Janz, 23, who was diagnosed with the disease just eight months after he was born. “After I got my new stem cells, my hair came back dark, dirty blonde, then it lightened a little bit, but before it was white blonde, almost bleach blonde.”
According to Cystinosis United, about 500 to 600 people have the rare genetic disease in the U.S.; an estimated 20 new cases are diagnosed each year.
Located in Cambridge, Mass., AVROBIO is a gene therapy company that targets cystinosis and other lysosomal storage disorders, in which toxic materials build up in the cells. Janz is one of five patients in AVROBIO’s ongoing Phase 1/2 clinical trial of a gene therapy for cystinosis called AVR-RD-04.
Recently, AVROBIO compiled positive clinical data from this first and only gene therapy trial for the disease. The data show the potential of the therapy to genetically modify the patients’ own hematopoietic stem cells—a certain type of cell that’s capable of developing into all different types of blood cells—to express the functional protein they are deficient in. It stabilizes or reduces the impact of cystinosis on multiple tissues with a single dose.
Medical researchers have found that more than 80 different mutations to a gene called CTNS are responsible for causing cystinosis. The most common mutation results in a deficiency of the protein cystinosin. That protein functions as a transporter that regulates a lot metabolic processes in the cells.
“One of the first things we see in patients clinically is an accumulation of a particular amino acid called cystine, which grows toxic cystine crystals in the cells that cause serious complications,” explains Essra Rihda, chief medical officer for AVROBIO. “That happens in the cells across the tissues and organs of the body, so the disease affects many parts of the body.”

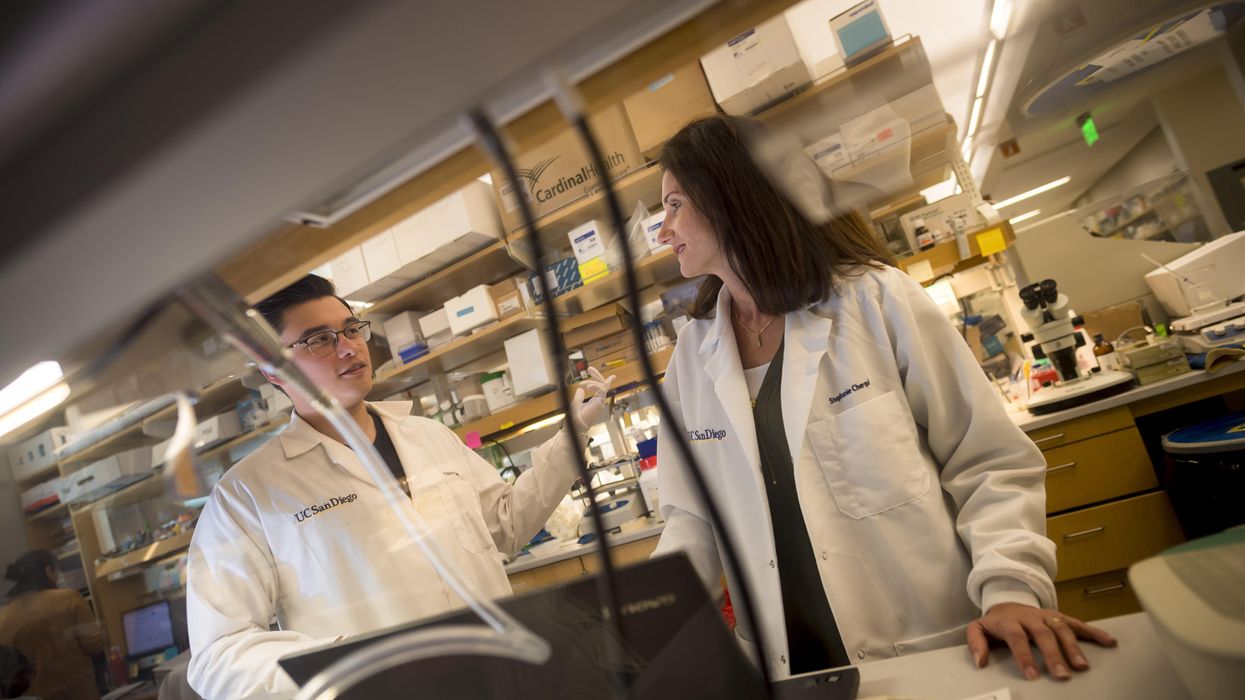
Jordan Janz, 23, meets Stephanie Cherqui, the principal investigator of his gene therapy trial, before the trial started in 2019.
Jordan Janz
According to Rihda, although cystinosis can occur in kids and adults, the most severe form of the disease affects infants and makes up about 95 percent of overall cases. Children typically appear healthy at birth, but around six to 18 months, they start to present for medical attention with failure to thrive.
Additionally, infants with cystinosis often urinate frequently, a sign of polyuria, and they are thirsty all the time, since the disease usually starts in the kidneys. Many develop chronic kidney disease that ultimately progresses to the point where the kidney no longer supports the body’s needs. At that stage, dialysis is required and then a transplant. From there the disease spreads to many other organs, including the eyes, muscles, heart, nervous system, etc.
“The gene for cystinosis is expressed in every single tissue we have, and the accumulation of this toxic buildup alters all of the organs of the patient, so little by little all of the organs start to fail,” says Stephanie Cherqui, principal investigator of Cherqui Lab, which is part of UC San Diego’s Department of Pediatrics.
Since the 1950s, a drug called cysteamine showed some therapeutic effect on cystinosis. It was approved by the FDA in 1994 to prevent damage that may be caused by the buildup of cystine crystals in organs. Prior to FDA approval, Cherqui says, children were dying of the disease before they were ten-years-old or after a kidney transplant. By taking oral cysteamine, they can live from 20 to 50 years longer. But it’s a challenging drug because it has to be taken every 6 or 12 hours, and there are serious gastric side effects such as nausea and diarrhea.
“With all of the complications they develop, the typical patient takes 40 to 60 pills a day around the clock,” Cherqui says. “They literally have a suitcase of medications they have to carry everywhere, and all of those medications don’t stop the progression of the disease, and they still die from it.”
Cherqui has been a proponent of gene therapy to treat children’s disorders since studying cystinosis while earning her doctorate in 2002. Today, her lab focuses on developing stem cell and gene therapy strategies for degenerative, hereditary disorders such as cystinosis that affect multiple systems of the body. “Because cystinosis expresses in every tissue in the body, I decided to use the blood-forming stem cells that we have in our bone marrow,” she explains. “These cells can migrate to anywhere in the body where the person has an injury from the disease.”
AVROBIO’s hematopoietic stem cell gene therapy approach collects stem cells from the patient’s bone marrow. They then genetically modify the stem cells to give the patient a copy of the healthy CTNS gene, which the person either doesn’t have or it’s defective.
The patient first undergoes apheresis, a medical procedure in which their blood is passed through an apparatus that separates out the diseased stem cells, and a process called conditioning is used to help eliminate the damaged cells so they can be replaced by the infusion of the patient’s genetically modified stem cells. Once they become engrafted into the patient’s bone marrow, they reproduce into a lot of daughter cells, and all of those daughter cells contain the CTNS gene. Those cells are able to express the healthy, functional, active protein throughout the body to correct the metabolic problem caused by cystinosis.
“What we’re seeing in the adult patients who have been dosed to date is the consistent and sustained engraftment of our genetically modified cells, 17 to 27 months post-gene therapy, so that’s very encouraging and positive,” says Rihda, the chief medical officer at AVROBIO.
When Janz was 11-years-old, his mother got him enrolled in the trial of a new form of cysteamine that would only need to be taken every 12 hours instead of every six. Two years later, she made sure he was the first person on the list for Cherqui’s current stem cell gene therapy trial.
AVROBIO researchers have also confirmed stabilization or improvement in motor coordination and visual perception in the trial participants, suggesting a potential impact on the neuropathology of the disease. Data from five dosed patients show strong safety and tolerability as well as reduced accumulation of cystine crystals in cells across multiple tissues in the first three patients. None of the five patients need to take oral cysteamine.
Janz’s mother, Barb Kulyk, whom he credits with always making him take his medications and keeping him hydrated, had been following Cherqui’s research since his early childhood. When Janz was 11-years-old, she got him enrolled in the trial of a new form of cysteamine that would only need to be taken every 12 hours instead of every six. When he was 17, the FDA approved that drug. Two years later, his mother made sure he was the first person on the list for Cherqui’s current stem cell gene therapy trial. He received his new stem cells on October 7th, 2019, went home in January 2020, and returned to working full time in February.

Jordan Janz, pictured here with his girlfriend, has a new lease on life, plus a new hair color.
Jordan Janz
He notes that his energy level is significantly better, and his mother has noticed much improvement in him and his daily functioning: He rarely vomits or gets nauseous in the morning, and he has more color in his face as well as his hair. Although he could finish his participation at any time, he recently decided to continue in the clinical trial.
Before the trial, Janz was taking 56 pills daily. He is completely off all of those medications and only takes pills to keep his kidneys working. Because of the damage caused by cystinosis over the course of his life, he’s down to about 20 percent kidney function and will eventually need a transplant.
“Some day, though, thanks to Dr. Cherqui’s team and AVROBIO’s work, when I get a new kidney, cystinosis won’t destroy it,” he concludes.