Nobel Prize goes to technology for mRNA vaccines

Katalin Karikó, pictured, and Drew Weissman won the Nobel Prize for advances in mRNA research that led to the first Covid vaccines.
When Drew Weissman received a call from Katalin Karikó in the early morning hours this past Monday, he assumed his longtime research partner was calling to share a nascent, nagging idea. Weissman, a professor of medicine at the Perelman School of Medicine at the University of Pennsylvania, and Karikó, a professor at Szeged University and an adjunct professor at UPenn, both struggle with sleep disturbances. Thus, middle-of-the-night discourses between the two, often over email, has been a staple of their friendship. But this time, Karikó had something more pressing and exciting to share: They had won the 2023 Nobel Prize in Physiology or Medicine.
The work for which they garnered the illustrious award and its accompanying $1,000,000 cash windfall was completed about two decades ago, wrought through long hours in the lab over many arduous years. But humanity collectively benefited from its life-saving outcome three years ago, when both Moderna and Pfizer/BioNTech’s mRNA vaccines against COVID were found to be safe and highly effective at preventing severe disease. Billions of doses have since been given out to protect humans from the upstart viral scourge.
“I thought of going somewhere else, or doing something else,” said Katalin Karikó. “I also thought maybe I’m not good enough, not smart enough. I tried to imagine: Everything is here, and I just have to do better experiments.”
Unlocking the power of mRNA
Weissman and Karikó unlocked mRNA vaccines for the world back in the early 2000s when they made a key breakthrough. Messenger RNA molecules are essentially instructions for cells’ ribosomes to make specific proteins, so in the 1980s and 1990s, researchers started wondering if sneaking mRNA into the body could trigger cells to manufacture antibodies, enzymes, or growth agents for protecting against infection, treating disease, or repairing tissues. But there was a big problem: injecting this synthetic mRNA triggered a dangerous, inflammatory immune response resulting in the mRNA’s destruction.
While most other researchers chose not to tackle this perplexing problem to instead pursue more lucrative and publishable exploits, Karikó stuck with it. The choice sent her academic career into depressing doldrums. Nobody would fund her work, publications dried up, and after six years as an assistant professor at the University of Pennsylvania, Karikó got demoted. She was going backward.
“I thought of going somewhere else, or doing something else,” Karikó told Stat in 2020. “I also thought maybe I’m not good enough, not smart enough. I tried to imagine: Everything is here, and I just have to do better experiments.”
A tale of tenacity
Collaborating with Drew Weissman, a new professor at the University of Pennsylvania, in the late 1990s helped provide Karikó with the tenacity to continue. Weissman nurtured a goal of developing a vaccine against HIV-1, and saw mRNA as a potential way to do it.
“For the 20 years that we’ve worked together before anybody knew what RNA is, or cared, it was the two of us literally side by side at a bench working together,” Weissman said in an interview with Adam Smith of the Nobel Foundation.
In 2005, the duo made their 2023 Nobel Prize-winning breakthrough, detailing it in a relatively small journal, Immunity. (Their paper was rejected by larger journals, including Science and Nature.) They figured out that chemically modifying the nucleoside bases that make up mRNA allowed the molecule to slip past the body’s immune defenses. Karikó and Weissman followed up that finding by creating mRNA that’s more efficiently translated within cells, greatly boosting protein production. In 2020, scientists at Moderna and BioNTech (where Karikó worked from 2013 to 2022) rushed to craft vaccines against COVID, putting their methods to life-saving use.
The future of vaccines
Buoyed by the resounding success of mRNA vaccines, scientists are now hurriedly researching ways to use mRNA medicine against other infectious diseases, cancer, and genetic disorders. The now ubiquitous efforts stand in stark contrast to Karikó and Weissman’s previously unheralded struggles years ago as they doggedly worked to realize a shared dream that so many others shied away from. Katalin Karikó and Drew Weissman were brave enough to walk a scientific path that very well could have ended in a dead end, and for that, they absolutely deserve their 2023 Nobel Prize.
This article originally appeared on Big Think, home of the brightest minds and biggest ideas of all time.
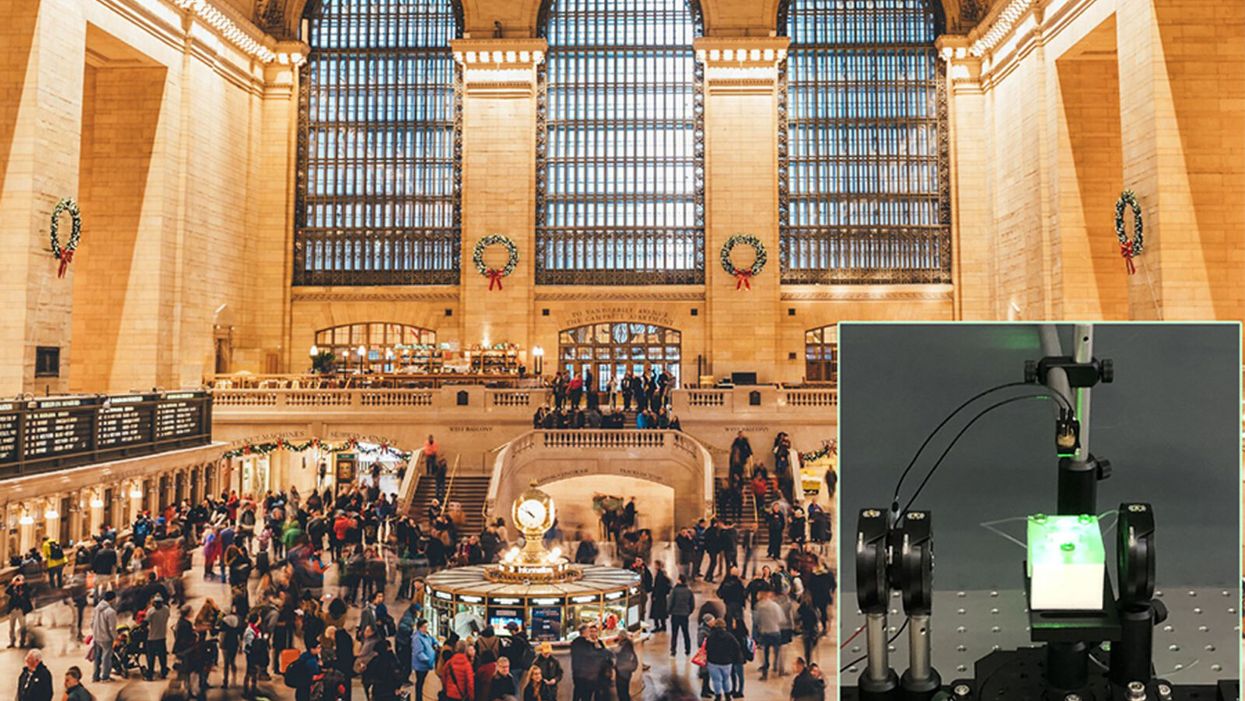
A biosensor in development (inset) could potentially be used to detect novel viruses in transit hubs like Grand Central Station in New York City.
The unprecedented scale and impact of the COVID-19 pandemic has caused scientists and engineers around the world to stop whatever they were working on and shift their research toward understanding a novel virus instead.
"We have confidence that we can use our system in the next pandemic."
For Guangyu Qiu, normally an environmental engineer at the Swiss Federal Laboratories for Materials Science and Technology, that means finding a clever way to take his work on detecting pollution in the air and apply it to living pathogens instead. He's developing a new type of biosensor to make disease diagnostics and detection faster and more accurate than what's currently available.
But even though this pandemic was the impetus for designing a new biosensor, Qiu actually has his eye on future disease outbreaks. He admits that it's unlikely his device will play a role in quelling this virus, but says researchers already need to be thinking about how to make better tools to fight the next one — because there will be a next one.
"In the last 20 years, there [have been] three different coronavirus [outbreaks] ... so we have to prepare for the coming one," Qiu says. "We have confidence that we can use our system in the next pandemic."
"A Really, Really Neat Idea"
His main concern is the diagnostic tool that's currently front and center for testing patients for SARS-Cov-2, the virus causing the novel coronavirus disease. The tool, called PCR (short for reverse transcription polymerase chain reaction), is the gold standard because it excels at detecting viruses in even very small samples of mucus. PCR can amplify genetic material in the limited sample and look for a genetic code matching the virus in question. But in many parts of the world, mucus samples have to be sent out to laboratories for that work, and results can take days to return. PCR is also notoriously prone to false positives and negatives.
"I read a lot of newspapers that report[ed] ... a lot of false negative or false positive results at the very beginning of the outbreak," Qiu says. "It's not good for protecting people to prevent further transmission of the disease."
So he set out to build a more sensitive device—one that's less likely to give you a false result. Qiu's biosensor relies on an idea similar to the dual-factor authentication required of anyone trying to access a secure webpage. Instead of verifying that a virus is really present by using one way of detecting genetic code, as with PCR, this biosensor asks for two forms of ID.
SARS-CoV-2 is what's called an RNA virus, which means it has a single strand of genetic code, unlike double-stranded DNA. Inside Qiu's biosensor are receptors with the complementary code for this particular virus' RNA; if the virus is present, its RNA will bind with the receptors, locking together like velcro. The biosensor also contains a prism and a laser that work together to verify that this RNA really belongs to SARS-CoV-2 by looking for a specific wavelength of light and temperature.
If the biosensor doesn't detect either, or only registers a match for one and not the other, then it can't produce a positive result. This multi-step authentication process helps make sure that the RNA binding with the receptors isn't a genetically similar coronavirus like SARS-CoV, known for its 2003 outbreak, or MERS-CoV, which caused an epidemic in 2012.
It could also be fitted to detect future novel viruses once their genomes are sequenced.
The dual-feature design of this biosensor "is a really, really neat idea that I have not seen before with other sensor technology," says Erin Bromage, a professor of infection and immunology at the University of Massachusetts Dartmouth; he was not involved in designing or testing Qiu's biosensor. "It makes you feel more secure that when you have a positive, you've really got a positive."
The light and temperature sensors are not in themselves new inventions, but the combination is a first. The part of the device that uses light to detect particles is actually central to Qiu's normal stream of environmental research, and is a versatile tool he's been working with for a long time to detect aerosols in the atmosphere and heavy metals in drinking water.
Bromage says this is a plus. "It's not high-risk in the sense that how they do this is unique, or not validated. They've taken aspects of really proven technology and sort of combined it together."
This new biosensor is still a prototype that will take at least another 12 months to validate in real world scenarios, though. The device is sound from a biological perspective and is sensitive enough to reliably detect SARS-CoV-2 — and to not be tricked by genetically similar viruses like SARS-CoV — but there is still a lot of engineering work that needs to be done in order for it to work outside the lab. Qiu says it's unlikely that the sensor will help minimize the impact of this pandemic, but the RNA receptors, prism, and laser inside the device can be customized to detect other viruses that may crop up in the future.
"If we choose another sequence—like SARS, like MERS, or like normal seasonal flu—we can detect other viruses, or even bacteria," Qiu says. "This device is very flexible."
It could also be fitted to detect future novel viruses once their genomes are sequenced.
The Long-Term Vision: Hospitals and Transit Hubs
The device has been designed to connect with two other systems: an air sampler and a microprocessor because the goal is to make it portable, and able to pick up samples from the air in hospitals or public areas like train stations or airports. A virus could hopefully be detected before it silently spreads and erupts into another global pandemic. In the case of SARS-CoV-2, there has been conflicting research about whether or not the virus is truly airborne (though it can be spread by droplets that briefly move through the air after a cough or sneeze), whereas the highly contagious RNA virus that causes measles can remain in the air for up to two hours.
"They've got a lot on the front end to work out," Bromage says. "They've got to work out how to capture and concentrate a virus, extract the RNA from the virus, and then get it onto the sensor. That's some pretty big hurdles, and may take some engineering that doesn't exist right now. But, if they can do that, then that works out really quite well."
One of the major obstacles in containing the COVID-19 pandemic has been in deploying accurate, quick tools that can be used for early detection of a virus outbreak and for later tracing its spread. That will still be true the next time a novel virus rears its head, and it's why Qiu feels that even if his biosensor can't help just yet, the research is still worth the effort.
It could also be fitted to detect future novel viruses once their genomes are sequenced.
The dual-feature design of this biosensor "is a really, really neat idea that I have not seen before with other sensor technology," says Erin Bromage, a professor of infection and immunology at the University of Massachusetts Dartmouth; he was not involved in designing or testing Qiu's biosensor. "It makes you feel more secure that when you have a positive, you've really got a positive."
The light and temperature sensors are not in themselves new inventions, but the combination is a first. The part of the device that uses light to detect particles is actually central to Qiu's normal stream of environmental research, and is a versatile tool he's been working with for a long time to detect aerosols in the atmosphere and heavy metals in drinking water.
Bromage says this is a plus. "It's not high-risk in the sense that how they do this is unique, or not validated. They've taken aspects of really proven technology and sort of combined it together."
This new biosensor is still a prototype that will take at least another 12 months to validate in real world scenarios, though. The device is sound from a biological perspective and is sensitive enough to reliably detect SARS-CoV-2 — and to not be tricked by genetically similar viruses like SARS-CoV — but there is still a lot of engineering work that needs to be done in order for it to work outside the lab. Qiu says it's unlikely that the sensor will help minimize the impact of this pandemic, but the RNA receptors, prism, and laser inside the device can be customized to detect other viruses that may crop up in the future.
"If we choose another sequence—like SARS, like MERS, or like normal seasonal flu—we can detect other viruses, or even bacteria," Qiu says. "This device is very flexible."
It could also be fitted to detect future novel viruses once their genomes are sequenced.
The Long-Term Vision: Hospitals and Transit Hubs
The device has been designed to connect with two other systems: an air sampler and a microprocessor because the goal is to make it portable, and able to pick up samples from the air in hospitals or public areas like train stations or airports. A virus could hopefully be detected before it silently spreads and erupts into another global pandemic. In the case of SARS-CoV-2, there has been conflicting research about whether or not the virus is truly airborne (though it can be spread by droplets that briefly move through the air after a cough or sneeze), whereas the highly contagious RNA virus that causes measles can remain in the air for up to two hours.
"They've got a lot on the front end to work out," Bromage says. "They've got to work out how to capture and concentrate a virus, extract the RNA from the virus, and then get it onto the sensor. That's some pretty big hurdles, and may take some engineering that doesn't exist right now. But, if they can do that, then that works out really quite well."
One of the major obstacles in containing the COVID-19 pandemic has been in deploying accurate, quick tools that can be used for early detection of a virus outbreak and for later tracing its spread. That will still be true the next time a novel virus rears its head, and it's why Qiu feels that even if his biosensor can't help just yet, the research is still worth the effort.
Spina Bifida Claimed My Son's Mobility. Incredible Breakthroughs May Let Future Kids Run Free.
Sarah Watts's son Henry was born with spina bifida and can't stand or walk without assistance.
When our son Henry, now six, was diagnosed with spina bifida at his 20-week ultrasound, my husband and I were in shock. It took us more than a few minutes to understand what the doctor was telling us.
When Henry was diagnosed in 2012, postnatal surgery was still the standard of care – but that was about to change.
Neither of us had any family history of birth defects. Our fifteen-month-old daughter, June, was in perfect health.
But more than that, spina bifida – a malformation of the neural tube that eventually becomes the baby's spine – is woefully complex. The defect, the doctor explained, was essentially a hole in Henry's lower spine from which his spinal nerves were protruding – and because they were exposed to my amniotic fluid, those nerves were already permanently damaged. After birth, doctors could push the nerves back into his body and sew up the hole, but he would likely experience some level of paralysis, bladder and bowel dysfunction, and a buildup of cerebrospinal fluid that would require a surgical implant called a shunt to correct. The damage was devastating – and irreversible.
We returned home with June and spent the next few days cycling between disbelief and total despair. But within a week, the maternal-fetal medicine specialist who diagnosed Henry called us up and gave us the first real optimism we had felt in days: There was a new, experimental surgery for spina bifida that was available in just a handful of hospitals around the country. Rather than waiting until birth to repair the baby's defect, some doctors were now trying out a prenatal repair, operating on the baby via c-section, closing the defect, and then keeping the mother on strict bedrest until it was time for the baby to be delivered, just before term.
This new surgery carried risks, he told us – but if it went well, there was a chance Henry wouldn't need a shunt. And because repairing the defect during my pregnancy meant the spinal nerves were exposed for a shorter amount of time, that meant we'd be preventing nerve damage – and less nerve damage meant that there was a chance he'd be able to walk.
Did we want in? the doctor asked.
Had I known more about spina bifida and the history of its treatment, this surgery would have seemed even more miraculous. Not too long ago, the standard of care for babies born with spina bifida was to simply let them die without medical treatment. In fact, it wasn't until the early 1950s that doctors even attempted to surgically repair the baby's defect at all, instead of opting to let the more severe cases die of meningitis from their open wound. (Babies who had closed spina bifida – a spinal defect covered by skin – sometimes survived past infancy, but rarely into adulthood).
But in the 1960s and 1970s, as more doctors started repairing defects and the shunting technology improved, patients with spina bifida began to survive past infancy. When catheterization was introduced, spina bifida patients who had urinary dysfunction, as is common, were able to preserve their renal function into adulthood, and they began living even longer. Within a few decades, spina bifida was no longer considered a death sentence; people were living fuller, happier lives.
When Henry was diagnosed in 2012, postnatal surgery was still the standard of care – but that was about to change. The first major clinical trial for prenatal surgery and spina bifida, called Management of Myelomeningocele (MOMS) had just concluded, and its objective was to see whether repairing the baby's defect in utero would be beneficial. In the trial, doctors assigned eligible women to undergo prenatal surgery in the second trimester of their pregnancies and then followed up with their children throughout the first 30 months of the child's life.
The results were groundbreaking: Not only did the children in the surgery group perform better on motor skills and cognitive tests than did patients in the control group, only 40 percent of patients ended up needing shunts compared to 80 percent of patients who had postnatal surgery. The results were so overwhelmingly positive that the trial was discontinued early (and is now, happily, the medical standard of care). Our doctor relayed this information to us over the phone, breathless, and left my husband and me to make our decision.
After a few days of consideration, and despite the benefits, my husband and I actually ended up opting for the postnatal surgery instead. Prenatal surgery, although miraculous, would have required extensive travel for us, as well as giving birth in a city thousands of miles from home with no one to watch our toddler while my husband worked and I recovered. But other parents I met online throughout our pregnancy did end up choosing prenatal surgery for their children – and the majority of them now walk with little assistance and only a few require shunting.
Even more amazing to me is that now – seven years after Henry's diagnosis, and not quite a decade since the landmark MOMS trial – the standard of care could be about to change yet again.
Regardless of whether they have postnatal or prenatal surgery, most kids with spina bifida still experience some level of paralysis and rely on wheelchairs and walkers to move around. Now, researchers at UC Davis want to augment the fetal surgery with a stem cell treatment, using human placenta-derived mesenchymal stromal cells (PMSCs) and affixing them to a cellular scaffold on the baby's defect, which not only protects the spinal cord from further damage but actually encourages cellular regeneration as well.
The hope is that this treatment will restore gross motor function after the baby is born – and so far, in animal trials, that's exactly what's happening. Fetal sheep, who were induced with spinal cord injuries in utero, were born with complete motor function after receiving prenatal surgery and PMSCs. In 2017, a pair of bulldogs born with spina bifida received the stem cell treatment a few weeks after birth – and two months after surgery, both dogs could run and play freely, whereas before they had dragged their hind legs on the ground behind them. UC Davis researchers hope to bring this treatment into human clinical trials within the next year.
A century ago, a diagnosis of spina bifida meant almost certain death. Today, most children with spina bifida live into adulthood, albeit with significant disabilities. But thanks to research and innovation, it's entirely possible that within my lifetime – and certainly within Henry's – for the first time in human history, the disabilities associated with spina bifida could be a thing of the past.