Jurassic Park Without the Scary Parts: How Stem Cells May Rescue the Near-Extinct Rhinoceros

The Northern white rhinoceros Nola, the last one in the U.S. at that time in 2015, pictured here with author Jeanne Loring and Oliver Ryder (in truck), with a film crew and keepers in the San Diego Zoo's savanna. Nola sadly passed away that year.
I am a stem cell scientist. In my day job I work on developing ways to use stem cells to treat neurological disease – human disease. This is the story about how I became part of a group dedicated to rescuing the northern white rhinoceros from extinction.
The earth is now in an era that is called the "sixth mass extinction." The first extinction, 400 million years ago, put an end to 86 percent of the existing species, including most of the trilobites. When the earth grew hotter, dustier, or darker, it lost fish, amphibians, reptiles, plants, dinosaurs, mammals and birds. Each extinction event wiped out 80 to 90 percent of the life on the planet at the time. The first 5 mass extinctions were caused by natural disasters: volcanoes, fires, a meteor. But humans can take credit for the 6th.
Because of human activities that destroy habitats, creatures are now becoming extinct at a rate that is higher than any previously experienced. Some animals, like the giant panda and the California condor, have been pulled back from the brink of extinction by conserving their habitats, breeding in captivity, and educating the public about their plight.
But not the northern white rhino. This gentle giant is a vegetarian that can weigh up to 5,000 pounds. The rhino's weakness is its horn, which has become a valuable commodity because of the mistaken idea that it grants power and has medicinal value. Horns are not medicine; the horns are made of keratin, the same protein that is in fingernails. But as recently as 2017 more than 1,000 rhinos were slaughtered each year to harvest their horns.
All 6 rhino species are endangered. But the northern white has been devastated. Only two members of this species are alive now: Najin, age 32, and her daughter Fatu, 21, live in a protected park in Kenya. They are social animals and would prefer the company of other rhinos of their kind; but they can't know that they are the last two survivors of their entire species. No males exist anymore. The last male, Sudan, died in 2018 at age 45.
We are celebrating a huge milestone in the efforts to use stem cells to rescue the rhino.
I became involved in the rhino rescue project on a sunny day in February, 2008 at the San Diego Wild Animal Park in Escondido, about 30 miles north of my lab in La Jolla. My lab had relocated a couple of months earlier to Scripps Research Institute to start the Center for Regenerative Medicine for human stem cell research. To thank my staff for their hard work, I wanted to arrange a special treat. I contacted my friend Oliver Ryder, who is director of the Institute for Conservation Research at the zoo, to see if I could take them on a safari, a tour in a truck through the savanna habitat at the park.
This was the first of the "stem cell safaris" that the lab would enjoy over the next few years. On the safari we saw elands and cape buffalo, and fed giraffes and rhinos. And we talked about stem cells; in particular, we discussed a surprising technological breakthrough recently reported by the Japanese scientist Shinya Yamanaka that enabled conversion of ordinary skin cells into pluripotent stem cells.
Pluripotent stem cells can develop into virtually any cell type in the body. They exist when we are very young embryos; five days after we were just fertilized eggs, we became blastocysts, invisible tiny balls of a few hundred cells packed with the power to develop into an entire human being. Long before we are born, these cells of vast potential transform into highly specialized cells that generate our brains, our hearts, and everything else.
Human pluripotent stem cells from blastocysts can be cultured in the lab, and are called embryonic stem cells. But thanks to Dr. Yamanaka, anyone can have their skin cells reprogrammed into pluripotent stem cells, just like the ones we had when we were embryos. Dr. Yamanaka won the Nobel Prize for these cells, called "induced pluripotent stem cells" (iPSCs) several years later.
On our safari we realized that if we could make these reprogrammed stem cells from human skin cells, why couldn't we make them from animals' cells? How about endangered animals? Could such stem cells be made from animals whose skin cells had been being preserved since the 1970s in the San Diego Zoo's Frozen Zoo®? Our safari leader, Oliver Ryder, was the curator of the Frozen Zoo and knew what animal cells were stored in its giant liquid nitrogen tanks at −196°C (-320° F). The Frozen Zoo was established by Dr. Kurt Benirschke in 1975 in the hope that someday the collection would aid in rescue of animals that were on the brink of extinction. The frozen collection reached 10,000 cell lines this year.
We returned to the lab after the safari, and I asked my scientists if any of them would like to take on the challenge of making reprogrammed stem cells from endangered species. My new postdoctoral fellow, Inbar Friedrich Ben-Nun, raised her hand. Inbar had arrived only a few weeks earlier from Israel, and she was excited about doing something that had never been done before. Oliver picked the animals we would use. He chose his favorite animal, the critically endangered northern white rhinoceros, and the drill, which is an endangered primate related to the mandrill monkey,
When Inbar started work on reprogramming cells from the Frozen Zoo, there were 8 living northern rhinoceros around the world: Nola, Angalifu, Nesari, Nabire, Suni, Sudan, Najin, and Fatu. We chose to reprogram Fatu, the youngest of the remaining animals.
Through sheer determination and trial and error, Inbar got the reprogramming technique to work, and in 2011 we published the first report of iPSCs from endangered species in the scientific journal Nature Methods. The cover of the journal featured a drawing of an ark packed with animals that might someday be rescued through iPSC technology. By 2011, one of the 8 rhinos, Nesari, had died.
This kernel of hope for using iPSCs to rescue rhinos grew over the next 10 years. The zoo built the Rhino Rescue Center, and brought in 6 females of the closely related species, the southern white rhinoceros, from Africa. Southern white rhino populations are on the rise, and it appears that this species will survive, at least in captivity. The females are destined to be surrogate mothers for embryos made from northern white rhino cells, when eventually we hope to generate sperm and eggs from the reprogrammed stem cells, and fertilize the eggs in vitro, much the same as human IVF.

The author, Jeanne Loring, at the Rhino Rescue Center with one of the southern white rhino surrogates.
David Barker
As this project has progressed, we've been saddened by the loss of all but the last two remaining members of the species. Nola, the last northern white rhino in the U.S., who was at the San Diego Zoo, died in 2015.
But we are celebrating a huge milestone in the efforts to use stem cells to rescue the rhino. Just over a month ago, we reported that by reprogramming cells preserved in the Frozen Zoo, we produced iPSCs from stored cells of 9 northern white rhinos: Fatu, Najin, Nola, Suni, Nadi, Dinka, Nasima, Saut, and Angalifu. We also reprogrammed cells from two of the southern white females, Amani and Wallis.
We don't know when it will be possible to make a northern white rhino embryo; we have to figure out how to use methods already developed for laboratory mice to generate sperm and eggs from these cells. The male rhino Angalifu died in 2014, but ever since I saw beating heart cells derived from his very own cells in a culture dish, I've felt hope that he will one day have children who will seed a thriving new herd of northern white rhinos.
Scientists are making machines, wearable and implantable, to act as kidneys
Recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen soon.
Like all those whose kidneys have failed, Scott Burton’s life revolves around dialysis. For nearly two decades, Burton has been hooked up (or, since 2020, has hooked himself up at home) to a dialysis machine that performs the job his kidneys normally would. The process is arduous, time-consuming, and expensive. Except for a brief window before his body rejected a kidney transplant, Burton has depended on machines to take the place of his kidneys since he was 12-years-old. His whole life, the 39-year-old says, revolves around dialysis.
“Whenever I try to plan anything, I also have to plan my dialysis,” says Burton says, who works as a freelance videographer and editor. “It’s a full-time job in itself.”
Many of those on dialysis are in line for a kidney transplant that would allow them to trade thrice-weekly dialysis and strict dietary limits for a lifetime of immunosuppressants. Burton’s previous transplant means that his body will likely reject another donated kidney unless it matches perfectly—something he’s not counting on. It’s why he’s enthusiastic about the development of artificial kidneys, small wearable or implantable devices that would do the job of a healthy kidney while giving users like Burton more flexibility for traveling, working, and more.
Still, the devices aren’t ready for testing in humans—yet. But recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen soon, according to Jonathan Himmelfarb, a nephrologist at the University of Washington.
“It would liberate people with kidney failure,” Himmelfarb says.
An engineering marvel
Compared to the heart or the brain, the kidney doesn’t get as much respect from the medical profession, but its job is far more complex. “It does hundreds of different things,” says UCLA’s Ira Kurtz.
Kurtz would know. He’s worked as a nephrologist for 37 years, devoting his career to helping those with kidney disease. While his colleagues in cardiology and endocrinology have seen major advances in the development of artificial hearts and insulin pumps, little has changed for patients on hemodialysis. The machines remain bulky and require large volumes of a liquid called dialysate to remove toxins from a patient’s blood, along with gallons of purified water. A kidney transplant is the next best thing to someone’s own, functioning organ, but with over 600,000 Americans on dialysis and only about 100,000 kidney transplants each year, most of those in kidney failure are stuck on dialysis.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. Each of the 45 different cell types in the kidney do something different.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. To build an artificial heart, Kurtz says, you basically need to engineer a pump. An artificial pancreas needs to balance blood sugar levels with insulin secretion. While neither of these tasks is simple, they are fairly straightforward. The kidney, on the other hand, does more than get rid of waste products like urea and other toxins. Each of the 45 different cell types in the kidney do something different, helping to regulate electrolytes like sodium, potassium, and phosphorous; maintaining blood pressure and water balance; guiding the body’s hormonal and inflammatory responses; and aiding in the formation of red blood cells.
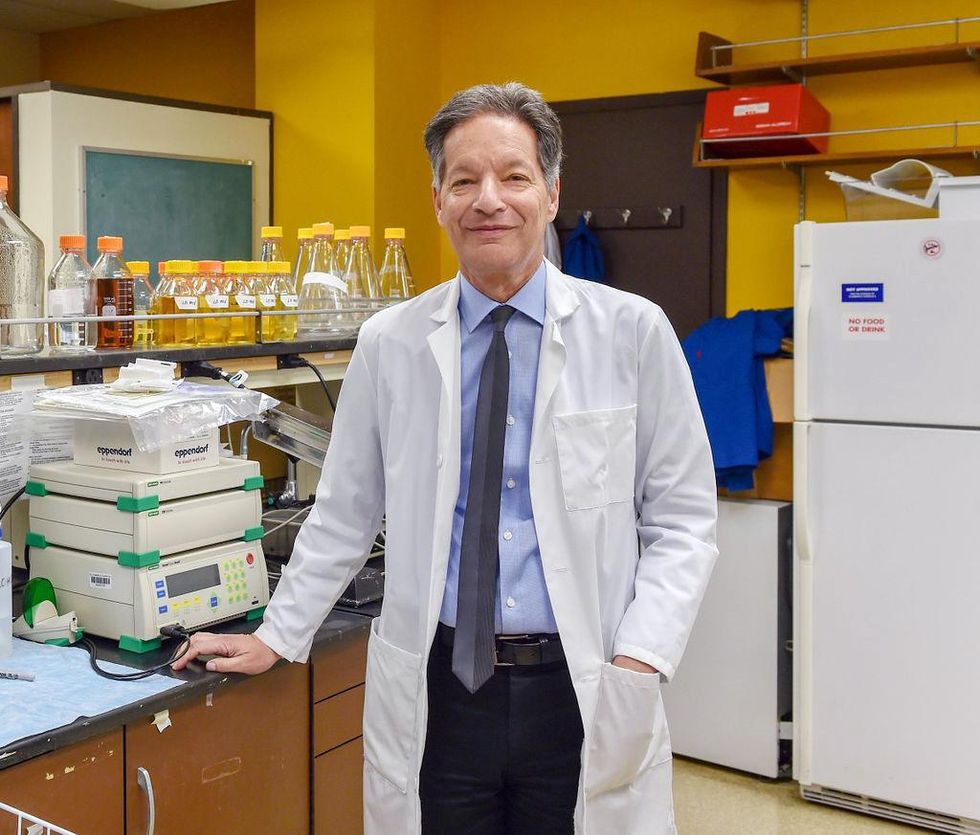
There's been little progress for patients during Ira Kurtz's 37 years as a nephrologist. Artificial kidneys would change that.
UCLA
Dialysis primarily filters waste, and does so well enough to keep someone alive, but it isn’t a true artificial kidney because it doesn’t perform the kidney’s other jobs, according to Kurtz, such as sensing levels of toxins, wastes, and electrolytes in the blood. Due to the size and water requirements of existing dialysis machines, the equipment isn’t portable. Physicians write a prescription for a certain duration of dialysis and assess how well it’s working with semi-regular blood tests. The process of dialysis itself, however, is conducted blind. Doctors can’t tell how much dialysis a patient needs based on kidney values at the time of treatment, says Meera Harhay, a nephrologist at Drexel University in Philadelphia.
But it’s the impact of dialysis on their day-to-day lives that creates the most problems for patients. Only one-quarter of those on dialysis are able to remain employed (compared to 85% of similar-aged adults), and many report a low quality of life. Having more flexibility in life would make a major different to her patients, Harhay says.
“Almost half their week is taken up by the burden of their treatment. It really eats away at their freedom and their ability to do things that add value to their life,” she says.
Art imitates life
The challenge for artificial kidney designers was how to compress the kidney’s natural functions into a portable, wearable, or implantable device that wouldn’t need constant access to gallons of purified and sterilized water. The other universal challenge they faced was ensuring that any part of the artificial kidney that would come in contact with blood was kept germ-free to prevent infection.
As part of the 2021 KidneyX Prize, a partnership between the U.S. Department of Health and Human Services and the American Society of Nephrology, inventors were challenged to create prototypes for artificial kidneys. Himmelfarb’s team at the University of Washington’s Center for Dialysis Innovation won the prize by focusing on miniaturizing existing technologies to create a portable dialysis machine. The backpack sized AKTIV device (Ambulatory Kidney to Increase Vitality) will recycle dialysate in a closed loop system that removes urea from blood and uses light-based chemical reactions to convert the urea to nitrogen and carbon dioxide, which allows the dialysate to be recirculated.
Himmelfarb says that the AKTIV can be used when at home, work, or traveling, which will give users more flexibility and freedom. “If you had a 30-pound device that you could put in the overhead bins when traveling, you could go visit your grandkids,” he says.
Kurtz’s team at UCLA partnered with the U.S. Kidney Research Corporation and Arkansas University to develop a dialysate-free desktop device (about the size of a small printer) as the first phase of a progression that will he hopes will lead to something small and implantable. Part of the reason for the artificial kidney’s size, Kurtz says, is the number of functions his team are cramming into it. Not only will it filter urea from blood, but it will also use electricity to help regulate electrolyte levels in a process called electrodeionization. Kurtz emphasizes that these additional functions are what makes his design a true artificial kidney instead of just a small dialysis machine.
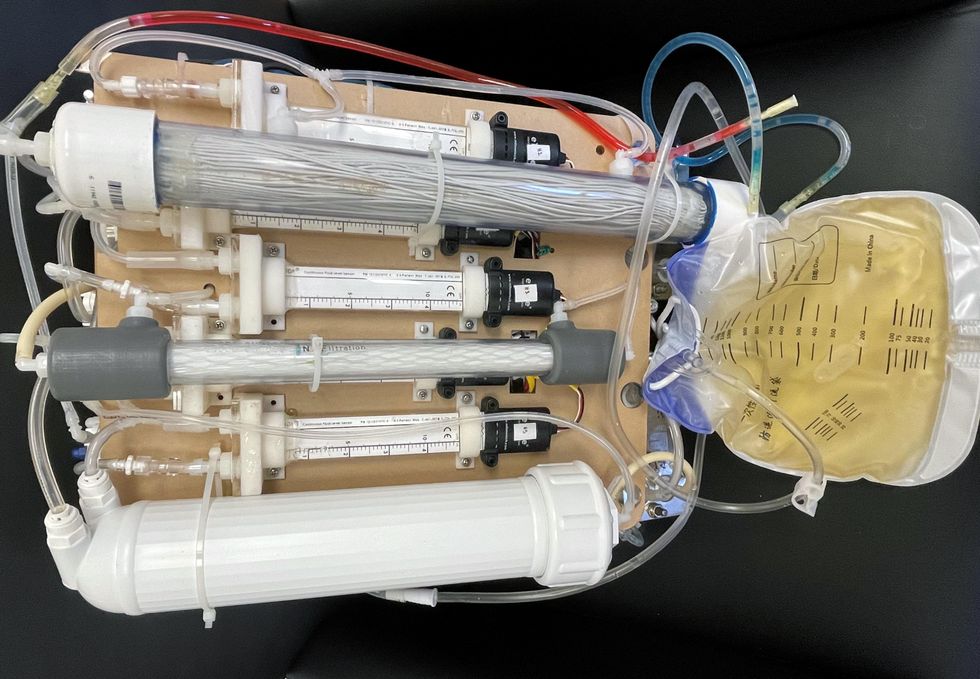
One version of an artificial kidney.
UCLA
“It doesn't have just a static function. It has a bank of sensors that measure chemicals in the blood and feeds that information back to the device,” Kurtz says.
Other startups are getting in on the game. Nephria Bio, a spinout from the South Korean-based EOFlow, is working to develop a wearable dialysis device, akin to an insulin pump, that uses miniature cartridges with nanomaterial filters to clean blood (Harhay is a scientific advisor to Nephria). Ian Welsford, Nephria’s co-founder and CTO, says that the device’s design means that it can also be used to treat acute kidney injuries in resource-limited settings. These potentials have garnered interest and investment in artificial kidneys from the U.S. Department of Defense.
For his part, Burton is most interested in an implantable device, as that would give him the most freedom. Even having a regular outpatient procedure to change batteries or filters would be a minor inconvenience to him.
“Being plugged into a machine, that’s not mimicking life,” he says.
This article was first published by Leaps.org on May 5, 2022.
With this new technology, hospitals and pharmacies could make vaccines and medicines onsite
New research focuses on methods that could change medicine-making worldwide. The scientists propose bursting cells open, removing their DNA and using the cellular gears inside to make therapies.
Most modern biopharmaceutical medicines are produced by workhorse cells—typically bacterial but sometimes mammalian. The cells receive the synthesizing instructions on a snippet of a genetic code, which they incorporate into their DNA. The cellular machinery—ribosomes, RNAs, polymerases, and other compounds—read and use these instructions to build the medicinal molecules, which are harvested and administered to patients.
Although a staple of modern pharma, this process is complex and expensive. One must first insert the DNA instructions into the cells, which they may or may not uptake. One then must grow the cells, keeping them alive and well, so that they produce the required therapeutics, which then must be isolated and purified. To make this at scale requires massive bioreactors and big factories from where the drugs are distributed—and may take a while to arrive where they’re needed. “The pandemic showed us that this method is slow and cumbersome,” says Govind Rao, professor of biochemical engineering who directs the Center for Advanced Sensor Technology at the University of Maryland, Baltimore County (UMBC). “We need better methods that can work faster and can work locally where an outbreak is happening.”
Rao and his team of collaborators, which spans multiple research institutions, believe they have a better approach that may change medicine-making worldwide. They suggest forgoing the concept of using living cells as medicine-producers. Instead, they propose breaking the cells and using the remaining cellular gears for assembling the therapeutic compounds. Instead of inserting the DNA into living cells, the team burst them open, and removed their DNA altogether. Yet, the residual molecular machinery of ribosomes, polymerases and other cogwheels still functioned the way it would in a cell. “Now if you drop your DNA drug-making instructions into that soup, this machinery starts making what you need,” Rao explains. “And because you're no longer worrying about living cells, it becomes much simpler and more efficient.” The collaborators detail their cell-free protein synthesis or CFPS method in their recent paper published in preprint BioAxiv.
While CFPS does not use living cells, it still needs the basic building blocks to assemble proteins from—such as amino acids, nucleotides and certain types of enzymes. These are regularly added into this “soup” to keep the molecular factory chugging. “We just mix everything in as a batch and we let it integrate,” says James Robert Swartz, professor of chemical engineering and bioengineering at Stanford University and co-author of the paper. “And we make sure that we provide enough oxygen.” Rao likens the process to making milk from milk powder.
For a variety of reasons—from the field’s general inertia to regulatory approval hurdles—the method hasn’t become mainstream. The pandemic rekindled interest in medicines that can be made quickly and easily, so it drew more attention to the technology.
The idea of a cell-free protein synthesis is older than one might think. Swartz first experimented with it around 1997, when he was a chemical engineer at Genentech. While working on engineering bacteria to make pharmaceuticals, he discovered that there was a limit to what E. coli cells, the workhorse darling of pharma, could do. For example, it couldn’t grow and properly fold some complex proteins. “We tried many genetic engineering approaches, many fermentation, development, and environmental control approaches,” Swartz recalls—to no avail.
“The organism had its own agenda,” he quips. “And because everything was happening within the organism, we just couldn't really change those conditions very easily. Some of them we couldn’t change at all—we didn’t have control.”
It was out of frustration with the defiant bacteria that a new idea took hold. Could the cells be opened instead, so that the protein-forming reactions could be influenced more easily? “Obviously, we’d lose the ability for them to reproduce,” Swartz says. But that also meant that they no longer needed to keep the cells alive and could focus on making the specific reactions happen. “We could take the catalysts, the enzymes, and the more complex catalysts and activate them, make them work together, much as they would in a living cell, but the way we wanted.”
In 1998, Swartz joined Stanford, and began perfecting the biochemistry of the cell-free method, identifying the reactions he wanted to foster and stopping those he didn’t want. He managed to make the idea work, but for a variety of reasons—from the field’s general inertia to regulatory approval hurdles—the method hasn’t become mainstream. The pandemic rekindled interest in medicines that can be made quickly and easily, so it drew more attention to the technology. For their BioArxiv paper, the team tested the method by growing a specific antiviral protein called griffithsin.
First identified by Barry O’Keefe at National Cancer Institute over a decade ago, griffithsin is an antiviral known to interfere with many viruses’ ability to enter cells—including HIV, SARS, SARS-CoV-2, MERS and others. Originally isolated from the red algae Griffithsia, it works differently from antibodies and antibody cocktails.
Most antiviral medicines tend to target the specific receptors that viruses use to gain entry to the cells they infect. For example, SARS-CoV-2 uses the infamous spike protein to latch onto the ACE2 receptor of mammalian cells. The antibodies or other antiviral molecules stick to the spike protein, shutting off its ability to cling onto the ACE2 receptors. Unfortunately, the spike proteins mutate very often, so the medicines lose their potency. On the contrary, griffithsin has the ability to cling to the different parts of viral shells called capsids—namely to the molecules of mannose, a type of sugar. That extra stuff, glued all around the capsid like dead weight, makes it impossible for the virus to squeeze into the cell.
“Every time we have a vaccine or an antibody against a specific SARS-CoV-2 strain, that strain then mutates and so you lose efficacy,” Rao explains. “But griffithsin molecules glom onto the viral capsid, so the capsid essentially becomes a sticky mess and can’t enter the cell.” Mannose molecules also don’t mutate as easily as viruses’ receptors, so griffithsin-based antivirals do not have to be constantly updated. And because mannose molecules are found on many viruses’ capsids, it makes griffithsin “a universal neutralizer,” Rao explains.
“When griffithsin was discovered, we recognized that it held a lot of promise as a potential antiviral agent,” O’Keefe says. In 2010, he published a paper about griffithsin efficacy in neutralizing viruses of the corona family—after the first SARS outbreak in the early 2000s, the scientific community was interested in such antivirals. Yet, griffithsin is still not available as an off-the-shelf product. So during the Covid pandemic, the team experimented with synthesizing griffithsin using the cell-free production method. They were able to generate potent griffithsin in less than 24 hours without having to grow living cells.
The antiviral protein isn't the only type of medicine that can be made cell-free. The proteins needed for vaccine production could also be made the same way. “Such portable, on-demand drug manufacturing platforms can produce antiviral proteins within hours, making them ideal for combating future pandemics,” Rao says. “We would be able to stop the pandemic before it spreads.”
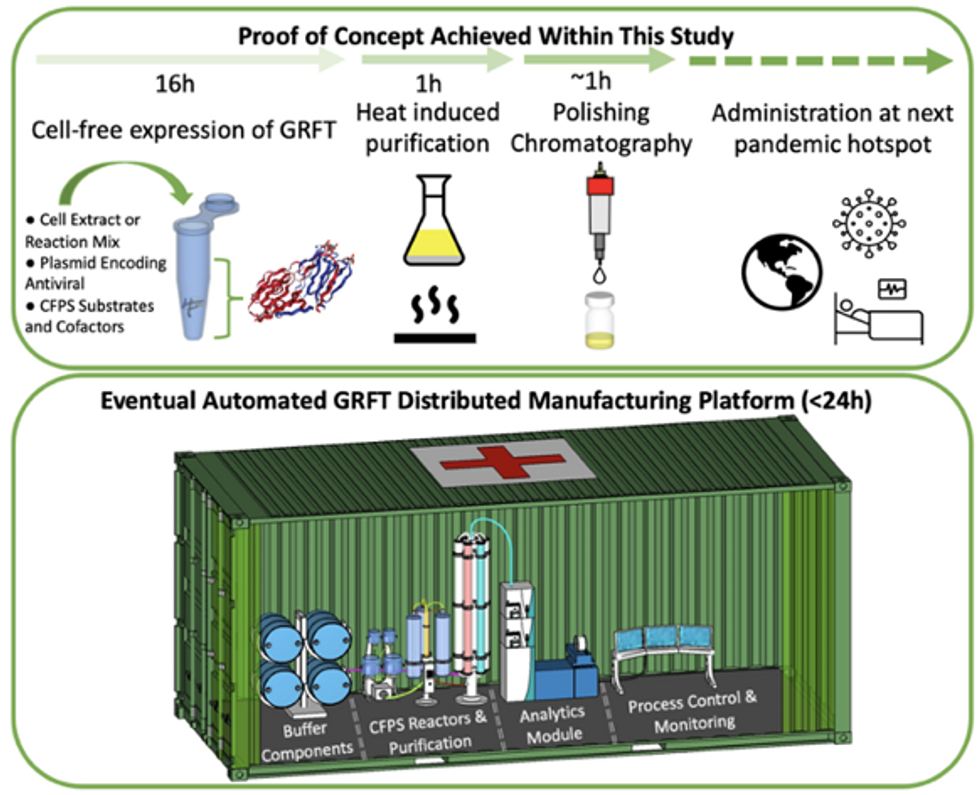
Top: Describes the process used in the study. Bottom: Describes how the new medicines and vaccines could be made at the site of a future viral outbreak.
Image courtesy of Rao and team, sourced from An approach to rapid distributed manufacturing of broad spectrumanti-viral griffithsin using cell-free systems to mitigate pandemics.
Rao’s idea is to perfect the technology to the point that any hospital or pharmacy can load up the media containing molecular factories, mix up the required amino acids, nucleotides and enzymes, and harvest the meds within hours. That will allow making medicines onsite and on demand. “That would be a self-contained production unit, so that you could just ship the production wherever the pandemic is breaking out,” says Swartz.
These units and the meds they produce, will, of course, have to undergo rigorous testing. “The biggest hurdles will be validating these against conventional technology,” Rao says. The biotech industry is risk-averse and prefers the familiar methods. But if this approach works, it may go beyond emergency situations and revolutionize the medicine-making paradigm even outside hospitals and pharmacies. Rao hopes that someday the method might become so mainstream that people may be able to buy and operate such reactors at home. “You can imagine a diabetic patient making insulin that way, or some other drugs,” Rao says. It would work not unlike making baby formula from the mere white powder. Just add water—and some oxygen, too.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.