The Skinny on Fat and Covid-19
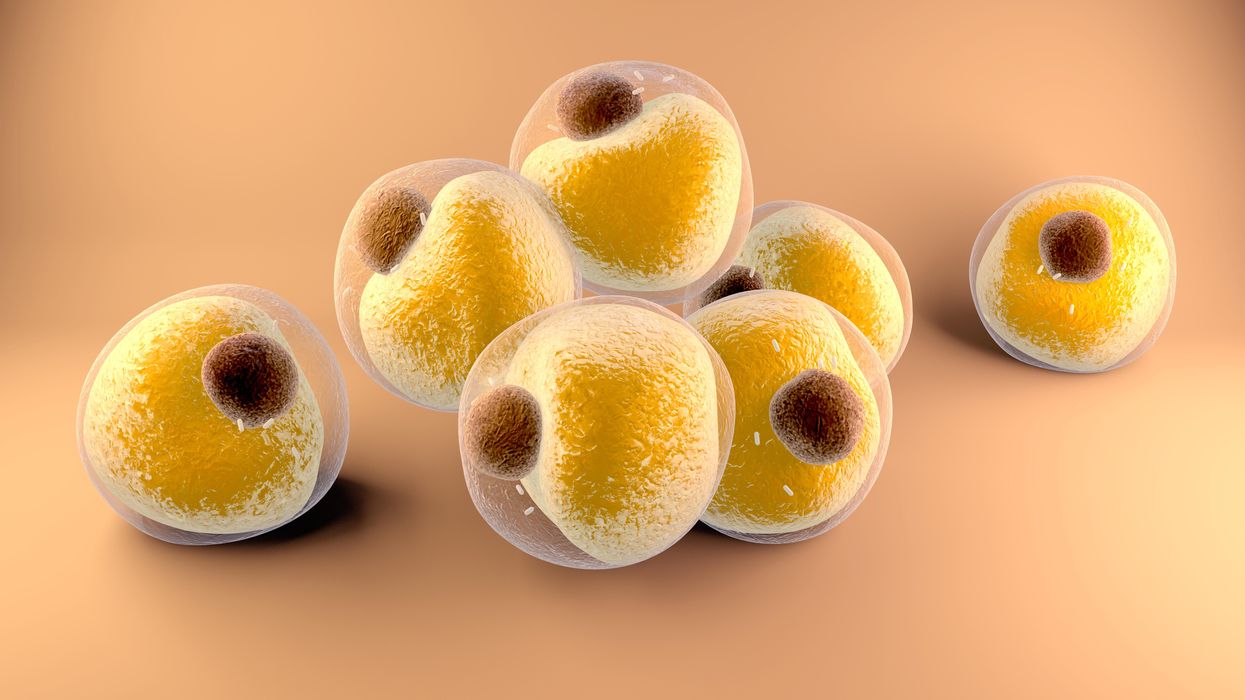
Researchers at Stanford have found that the virus that causes Covid-19 can infect fat cells, which could help explain why obesity is linked to worse outcomes for those who catch Covid-19.
Obesity is a risk factor for worse outcomes for a variety of medical conditions ranging from cancer to Covid-19. Most experts attribute it simply to underlying low-grade inflammation and added weight that make breathing more difficult.
Now researchers have found a more direct reason: SARS-CoV-2, the virus that causes Covid-19, can infect adipocytes, more commonly known as fat cells, and macrophages, immune cells that are part of the broader matrix of cells that support fat tissue. Stanford University researchers Catherine Blish and Tracey McLaughlin are senior authors of the study.
Most of us think of fat as the spare tire that can accumulate around the middle as we age, but fat also is present closer to most internal organs. McLaughlin's research has focused on epicardial fat, “which sits right on top of the heart with no physical barrier at all,” she says. So if that fat got infected and inflamed, it might directly affect the heart.” That could help explain cardiovascular problems associated with Covid-19 infections.
Looking at tissue taken from autopsy, there was evidence of SARS-CoV-2 virus inside the fat cells as well as surrounding inflammation. In fat cells and immune cells harvested from health humans, infection in the laboratory drove "an inflammatory response, particularly in the macrophages…They secreted proteins that are typically seen in a cytokine storm” where the immune response runs amok with potential life-threatening consequences. This suggests to McLaughlin “that there could be a regional and even a systemic inflammatory response following infection in fat.”
It is easy to see how the airborne SARS-CoV-2 virus infects the nose and lungs, but how does it get into fat tissue? That is a mystery and the source of ample speculation.
The macrophages studied by McLaughlin and Blish were spewing out inflammatory proteins, While the the virus within them was replicating, the new viral particles were not able to replicate within those cells. It was a different story in the fat cells. “When [the virus] gets into the fat cells, it not only replicates, it's a productive infection, which means the resulting viral particles can infect another cell,” including microphages, McLaughlin explains. It seems to be a symbiotic tango of the virus between the two cell types that keeps the cycle going.
It is easy to see how the airborne SARS-CoV-2 virus infects the nose and lungs, but how does it get into fat tissue? That is a mystery and the source of ample speculation.
Macrophages are mobile; they engulf and carry invading pathogens to lymphoid tissue in the lymph nodes, tonsils and elsewhere in the body to alert T cells of the immune system to the pathogen. Perhaps some of them also carry the virus through the bloodstream to more distant tissue.
ACE2 receptors are the means by which SARS-CoV-2 latches on to and enters most cells. They are not thought to be common on fat cells, so initially most researchers thought it unlikely they would become infected.
However, while some cell receptors always sit on the surface of the cell, other receptors are expressed on the surface only under certain conditions. Philipp Scherer, a professor of internal medicine and director of the Touchstone Diabetes Center at the University of Texas Southwestern Medical Center, suggests that, in people who have obesity, “There might be higher levels of dysfunctional [fat cells] that facilitate entry of the virus,” either through transiently expressed ACE2 or other receptors. Inflammatory proteins generated by macrophages might contribute to this process.
Another hypothesis is that viral RNA might be smuggled into fat cells as cargo in small bits of material called extracellular vesicles, or EVs, that can travel between cells. Other researchers have shown that when EVs express ACE2 receptors, they can act as decoys for SARS-CoV-2, where the virus binds to them rather than a cell. These scientists are working to create drugs that mimic this decoy effect as an approach to therapy.
Do fat cells play a role in Long Covid? “Fat cells are a great place to hide. You have all the energy you need and fat cells turn over very slowly; they have a half-life of ten years,” says Scherer. Observational studies suggest that acute Covid-19 can trigger the onset of diabetes especially in people who are overweight, and that patients taking medicines to regulate their diabetes “were actually quite protective” against acute Covid-19. Scherer has funding to study the risks and benefits of those drugs in animal models of Long Covid.
McLaughlin says there are two areas of potential concern with fat tissue and Long Covid. One is that this tissue might serve as a “big reservoir where the virus continues to replicate and is sent out” to other parts of the body. The second is that inflammation due to infected fat cells and macrophages can result in fibrosis or scar tissue forming around organs, inhibiting their function. Once scar tissue forms, the tissue damage becomes more difficult to repair.
Current Covid-19 treatments work by stopping the virus from entering cells through the ACE2 receptor, so they likely would have no effect on virus that uses a different mechanism. That means another approach will have to be developed to complement the treatments we already have. So the best advice McLaughlin can offer today is to keep current on vaccinations and boosters and lose weight to reduce the risk associated with obesity.
In this new video, we capture examples from history when people rejected scientific breakthroughs at first, only for the march of progress to continue.
What makes people turn against science? After two years of a global pandemic, the world has never felt more divided on questions of science. But this is not a new phenomenon. People have resisted scientific and technological advances throughout history.
This video by Leaps.org, with support from the Gordon and Betty Moore Foundation, captures noteworthy examples from history when people rejected science. What do these cases have in common? Scientific breakthroughs can be revolutionary, but revolutions can be disorienting and anxiety-producing. They transform our livelihoods, culture and even our understanding of what it means to be human. But there's reason for optimism. Many of history’s controversies were overcome. Science has a way of enduring, because it changes things for the better.
Scientists search for a universal coronavirus vaccine
Stephen Zeichner, an infectious disease specialist at the University of Virginia Medical Center, has made progress with an early stage universal coronavirus vaccine.
The Covid-19 pandemic had barely begun when VBI Vaccines, a biopharmaceutical company based in Cambridge, Massachusetts, initiated their search for a universal coronavirus vaccine.
It was March 2020, and while most pharmaceutical companies were scrambling to initiate vaccine programs which specifically targeted the SARS-CoV-2 virus, VBI’s executives were already keen to look at the broader picture.
Having observed the SARS and MERS coronavirus outbreaks over the last two decades, Jeff Baxter, CEO of VBI Vaccines, was aware that SARS-CoV-2 is unlikely to be the last coronavirus to move from an animal host into humans. “It's absolutely apparent that the future is to create a vaccine which gives more broad protection against not only pre-existing coronaviruses, but those that will potentially make the leap into humans in future,” says Baxter.
It was a prescient decision. Over the last two years, more biotechs and pharma companies have joined the search to find a vaccine which might be able to protect against all coronaviruses, along with dozens of academic research groups. Last September, the US National Institutes of Health dedicated $36 million specifically to pan-coronavirus vaccine research, while the global Coalition for Epidemic Preparedness Innovations (CEPI) has earmarked $200 million towards the effort.
Until October 2021, the very concept of whether it might be
theoretically possible to vaccinate against multiple coronaviruses remained an open question. But then a groundbreaking study renewed optimism.
The emergence of new variants of Covid-19 over the past year, particularly the highly mutated Omicron variant, has added greater impetus to find broader spectrum vaccines. But until October 2021, the very concept of whether it might be theoretically possible to vaccinate against multiple coronaviruses remained an open question. After all, scientists have spent decades trying to develop a similar vaccine for influenza with little success.
But then a groundbreaking study from renowned virologist Linfa Wang, who runs the emerging infectious diseases program at Duke-National University of Singapore Medical School, provided renewed optimism.
Wang found that eight SARS survivors who had been injected with the Pfizer/BioNTech Covid-19 vaccine had neutralising antibodies in their blood against SARS, the Alpha, Beta and Delta variants of SARS-CoV-2, and five other coronaviruses which reside in bats and pangolins. He concluded that the combination of past coronavirus infection, and immunization with a messenger RNA vaccine, had resulted in a wider spectrum of protection than might have been expected.
“This is a significant study because it showed that pre-existing immunity to one coronavirus could help with the elicitation of cross-reactive antibodies when immunizing with a second coronavirus,” says Kevin Saunders, Director of Research at the Duke Human Vaccine Institute in North Carolina, which is developing a universal coronavirus vaccine. “It provides a strategy to perhaps broaden the immune response against coronaviruses.”
In the next few months, some of the first data is set to emerge looking at whether this kind of antibody response could be elicited by a single universal coronavirus vaccine. In April 2021, scientists at the Walter Reed Army Institute of Research in Silver Spring, Maryland, launched a Phase I clinical trial of their vaccine, with a spokesman saying that it was successful, and the full results will be announced soon.
The Walter Reed researchers have already released preclinical data, testing the vaccine in non-human primates where it was found to have immunising capabilities against a range of Covid-19 variants as well as the original SARS virus. If the Phase I trial displays similar efficacy, a larger Phase II trial will begin later this year.
Two different approaches
Broadly speaking, scientists are taking two contrasting approaches to the task of finding a universal coronavirus vaccine. The Walter Reed Army Institute of Research, VBI Vaccines – who plan to launch their own clinical trial in the summer – and the Duke Human Vaccine Institute – who are launching a Phase I trial in early 2023 – are using a soccer-ball shaped ferritin nanoparticle studded with different coronavirus protein fragments.
VBI Vaccines is looking to elicit broader immune responses by combining SARS, SARS-CoV-2 and MERS spike proteins on the same nanoparticle. Dave Anderson, chief scientific officer at VBI Vaccines, explains that the idea is that by showing the immune system these three spike proteins at the same time, it can help train it to identify and respond to subtle differences between coronavirus strains.
The Duke Human Vaccine Institute is utilising the same method, but rather than including the entire spike proteins from different coronaviruses, they are only including the receptor binding domain (RBD) fragment from each spike protein. “We designed our vaccine to focus the immune system on a site of vulnerability for the virus, which is the receptor binding domain,” says Saunders. “Since the RBD is small, arraying multiple RBDs on a nanoparticle is a straight-forward approach. The goal is to generate immunity to many different subgenuses of viruses so that there will be cross-reactivity with new or unknown coronaviruses.”
But the other strategy is to create a vaccine which contains regions of the viral protein structure which are conserved between all coronavirus strains. This is something which scientists have tried to do for a universal influenza vaccine, but it is thought to be more feasible for coronaviruses because they mutate at a slower rate and are more constrained in the ways that they can evolve.
DIOSynVax, a biotech based in Cambridge, United Kingdom, announced in a press release earlier this month that they are partnering with CEPI to use their computational predictive modelling techniques to identify common structures between all of the SARS coronaviruses which do not mutate, and thus present good vaccine targets.
Stephen Zeichner, an infectious disease specialist at the University of Virginia Medical Center, has created an early stage vaccine using the fusion peptide region – another part of the coronavirus spike protein that aids the virus’s entry into host cells – which so far appears to be highly conserved between all coronaviruses.
So far Zeichner has trialled this version of the vaccine in pigs, where it provided protection against a different coronavirus called porcine epidemic diarrhea virus, which he described as very promising as this virus is from a different family called alphacoronaviruses, while SARS-CoV-2 is a betacoronavirus.
“If a betacoronavirus fusion peptide vaccine designed from SARS-CoV-2 can protect pigs against clinical disease from an alphacoronavirus, then that suggests that an analogous vaccine would enable broad protection against many, many different coronaviruses,” he says.
The road ahead
But while some of the early stage results are promising, researchers are fully aware of the scale of the challenge ahead of them. Although CEPI have declared an aim of having a licensed universal coronavirus vaccine available by 2024-2025, Zeichner says that such timelines are ambitious in the extreme.
“I was incredibly impressed at the speed at which the mRNA coronavirus vaccines were developed for SARS-CoV-2,” he says. “That was faster than just about anybody anticipated. On the other hand, I think a universal coronavirus vaccine is more equivalent to the challenge of developing an HIV vaccine and we're 35 years into that effort without success. We know a lot more now than before, and maybe it will be easier than we think. But I think the route to a universal vaccine is harder than an individual vaccine, so I wouldn’t want to put money on a timeline prediction.”
The major challenge for scientists is essentially designing a vaccine for a future threat which is not even here yet. As such, there are no guidelines on what safety data would be required to license such a vaccine, and how researchers can demonstrate that it truly provides efficacy against all coronaviruses, even those which have not yet jumped to humans.
The teams working on this problem have already devised some ingenious ways of approaching the challenge. VBI Vaccines have taken the genetic sequences of different coronaviruses found in bats and pangolins, from publicly available databases, and inserted them into what virologists call a pseudotype virus – one which has been engineered so it does not have enough genetic material to replicate.
This has allowed them to test the neutralising antibodies that their vaccine produces against these coronaviruses in test tubes, under safe lab conditions. “We have literally just been ordering the sequences, and making synthetic viruses that we can use to test the antibody responses,” says Anderson.
However, some scientists feel that going straight to a universal coronavirus vaccine is likely to be too complex. Instead they say that we should aim for vaccines which are a little more specific. Pamela Bjorkman, a structural biologist at the California Institute of Technology, suggests that pan-coronavirus vaccines which protect against SARS-like betacoronaviruses such as SARS or SARS-CoV-2, or MERS-like betacoronaviruses, may be more realistic.
“I think a vaccine to protect against all coronaviruses is likely impossible since there are so many varieties,” she says. “Perhaps trying to narrow down the scope is advisable.”
But if the mission to develop a universal coronavirus vaccine does succeed, it will be one of the most remarkable feats in the annals of medical science. In January, US chief medical advisor Anthony Fauci urged for greater efforts to be devoted towards this goal, one which scientists feel would be the biological equivalent of the race to develop the first atomic bomb
“The development of an effective universal coronavirus vaccine would be equally groundbreaking, as it would have global applicability and utility,” says Saunders. “Coronaviruses have caused multiple deadly outbreaks, and it is likely that another outbreak will occur. Having a vaccine that prevents death from a future outbreak would be a tremendous achievement in global health.”
He agrees that it will require creativity on a remarkable scale: “The universal coronavirus vaccine will also require ingenuity and perseverance comparable to that needed for the Manhattan project.”