The Skinny on Fat and Covid-19
Researchers at Stanford have found that the virus that causes Covid-19 can infect fat cells, which could help explain why obesity is linked to worse outcomes for those who catch Covid-19.
Obesity is a risk factor for worse outcomes for a variety of medical conditions ranging from cancer to Covid-19. Most experts attribute it simply to underlying low-grade inflammation and added weight that make breathing more difficult.
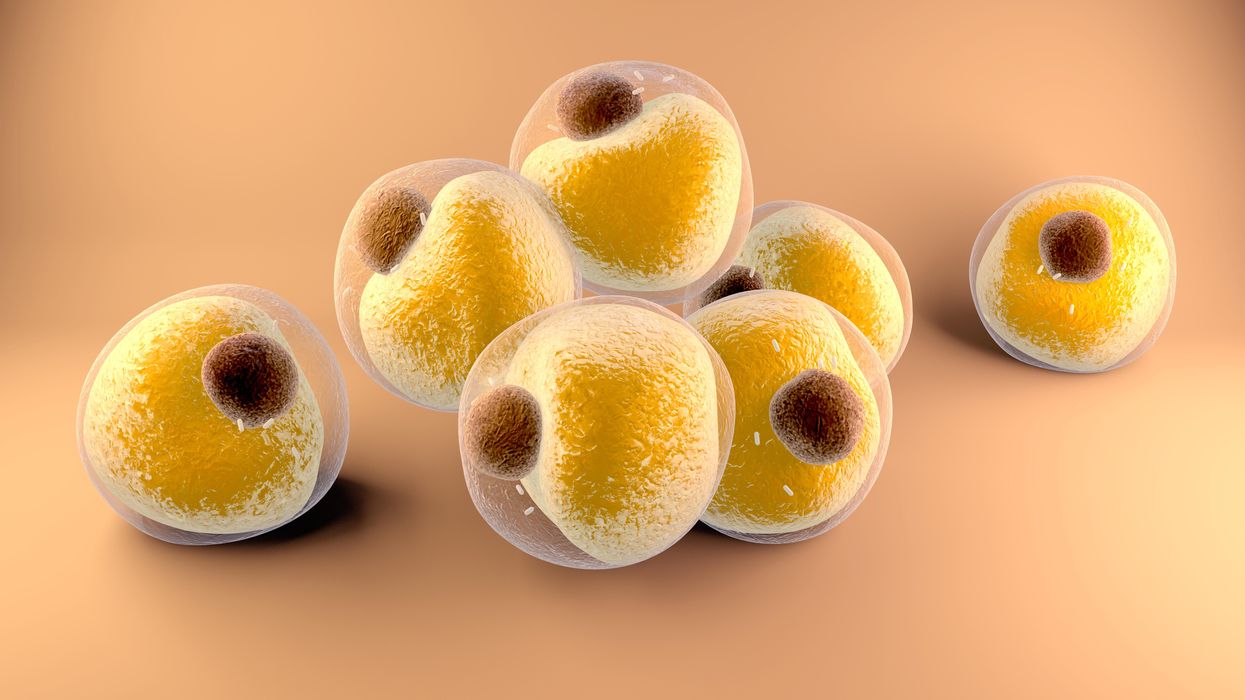
Now researchers have found a more direct reason: SARS-CoV-2, the virus that causes Covid-19, can infect adipocytes, more commonly known as fat cells, and macrophages, immune cells that are part of the broader matrix of cells that support fat tissue. Stanford University researchers Catherine Blish and Tracey McLaughlin are senior authors of the study.
Most of us think of fat as the spare tire that can accumulate around the middle as we age, but fat also is present closer to most internal organs. McLaughlin's research has focused on epicardial fat, “which sits right on top of the heart with no physical barrier at all,” she says. So if that fat got infected and inflamed, it might directly affect the heart.” That could help explain cardiovascular problems associated with Covid-19 infections.
Looking at tissue taken from autopsy, there was evidence of SARS-CoV-2 virus inside the fat cells as well as surrounding inflammation. In fat cells and immune cells harvested from health humans, infection in the laboratory drove "an inflammatory response, particularly in the macrophages…They secreted proteins that are typically seen in a cytokine storm” where the immune response runs amok with potential life-threatening consequences. This suggests to McLaughlin “that there could be a regional and even a systemic inflammatory response following infection in fat.”
It is easy to see how the airborne SARS-CoV-2 virus infects the nose and lungs, but how does it get into fat tissue? That is a mystery and the source of ample speculation.
The macrophages studied by McLaughlin and Blish were spewing out inflammatory proteins, While the the virus within them was replicating, the new viral particles were not able to replicate within those cells. It was a different story in the fat cells. “When [the virus] gets into the fat cells, it not only replicates, it's a productive infection, which means the resulting viral particles can infect another cell,” including microphages, McLaughlin explains. It seems to be a symbiotic tango of the virus between the two cell types that keeps the cycle going.
It is easy to see how the airborne SARS-CoV-2 virus infects the nose and lungs, but how does it get into fat tissue? That is a mystery and the source of ample speculation.
Macrophages are mobile; they engulf and carry invading pathogens to lymphoid tissue in the lymph nodes, tonsils and elsewhere in the body to alert T cells of the immune system to the pathogen. Perhaps some of them also carry the virus through the bloodstream to more distant tissue.
ACE2 receptors are the means by which SARS-CoV-2 latches on to and enters most cells. They are not thought to be common on fat cells, so initially most researchers thought it unlikely they would become infected.
However, while some cell receptors always sit on the surface of the cell, other receptors are expressed on the surface only under certain conditions. Philipp Scherer, a professor of internal medicine and director of the Touchstone Diabetes Center at the University of Texas Southwestern Medical Center, suggests that, in people who have obesity, “There might be higher levels of dysfunctional [fat cells] that facilitate entry of the virus,” either through transiently expressed ACE2 or other receptors. Inflammatory proteins generated by macrophages might contribute to this process.
Another hypothesis is that viral RNA might be smuggled into fat cells as cargo in small bits of material called extracellular vesicles, or EVs, that can travel between cells. Other researchers have shown that when EVs express ACE2 receptors, they can act as decoys for SARS-CoV-2, where the virus binds to them rather than a cell. These scientists are working to create drugs that mimic this decoy effect as an approach to therapy.
Do fat cells play a role in Long Covid? “Fat cells are a great place to hide. You have all the energy you need and fat cells turn over very slowly; they have a half-life of ten years,” says Scherer. Observational studies suggest that acute Covid-19 can trigger the onset of diabetes especially in people who are overweight, and that patients taking medicines to regulate their diabetes “were actually quite protective” against acute Covid-19. Scherer has funding to study the risks and benefits of those drugs in animal models of Long Covid.
McLaughlin says there are two areas of potential concern with fat tissue and Long Covid. One is that this tissue might serve as a “big reservoir where the virus continues to replicate and is sent out” to other parts of the body. The second is that inflammation due to infected fat cells and macrophages can result in fibrosis or scar tissue forming around organs, inhibiting their function. Once scar tissue forms, the tissue damage becomes more difficult to repair.
Current Covid-19 treatments work by stopping the virus from entering cells through the ACE2 receptor, so they likely would have no effect on virus that uses a different mechanism. That means another approach will have to be developed to complement the treatments we already have. So the best advice McLaughlin can offer today is to keep current on vaccinations and boosters and lose weight to reduce the risk associated with obesity.
Podcast: Should Scientific Controversies Be Silenced?
The recent Joe Rogan/Spotify controversy prompts the consideration of tough questions about expertise, trust, gatekeepers, and dissent.
The "Making Sense of Science" podcast features interviews with leading medical and scientific experts about the latest developments and the big ethical and societal questions they raise. This monthly podcast is hosted by journalist Kira Peikoff, founding editor of the award-winning science outlet Leaps.org.
The recent Joe Rogan/Spotify backlash over the misinformation presented in his recent episode on the Covid-19 vaccines raises some difficult and important bioethical questions for society: How can people know which experts to trust? What should big tech gatekeepers do about false claims promoted on their platforms? How should the scientific establishment respond to heterodox viewpoints from experts who disagree with the consensus? When is silencing of dissent merited, and when is it problematic? Journalist Kira Peikoff asks infectious disease physician and pandemic scholar Dr. Amesh Adalja to weigh in.

Dr. Amesh Adalja, Senior Scholar, Johns Hopkins Center for Health Security and an infectious disease physician
Listen to the Episode
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Scientists Are Studying How to Help Dogs Have Longer Lives, in a Bid to Further Our Own
Feeding dogs only once a day is showing health benefits in a large study, scientists report.
The sad eyes. The wagging tail. The frustrated whine. The excited bark. Dogs know how to get their owners to fork over the food more often.
The extra calories dogs get from feeding patterns now used by many Americans may not be good for them from a health and longevity viewpoint. In research from a large study called the Dog Aging Project, canines fed once a day had better scores on cognition tests and lower odds of developing diseases of organs throughout the body: intestinal tract, mouth and teeth, bones and joints, kidneys and bladder, and liver and pancreas.
Fewer than 1 in 10 dog owners fed their furry friends once daily, while nearly three fourths provided two daily meals.
“Most veterinarians have been led to believe that feeding dogs twice a day is optimal, but this is a relatively new idea that has developed over the past few decades with little supportive evidence from a health standpoint,” said Matt Kaeberlein, PhD, Co-Director of the Dog Aging Project, a professor of pathology and Director of the Healthy Aging and Longevity Research Institute at the University of Washington. Kaeberlein studies basic mechanisms of aging to find ways of extending the healthspan, the number of years of life lived free of disease. It’s not enough to extend the lifespan unless declines in biological function and risks of age-related diseases are also studied, he believes, hence the healthspan.
The Dog Aging Project is studying tens of thousands of dogs living with their owners in the real world, not a biology laboratory. The feeding study is the first of several reports now coming from the project based on owners’ annual reports of demographics, physical activity, environment, dog behavior, diet, medications and supplements, and health status. It has been posted on bioRxiv as it goes through peer review.
“All available evidence suggests that most biological mechanisms of aging in dogs will be conserved in humans. It just happens much faster in dogs.”
“The Dog Aging Project is one of the most exciting in the longevity space,” said David A. Sinclair, professor in the Department of Genetics and co-director of the Paul F. Glenn Center for Biology of Aging Research at Harvard Medical School. “Not only is it important to help our companions live longer and healthier, but because they are like people and share the same environment and many of the lifestyles as their owners, they are the perfect model for human longevity interventions.”
The epigenetic clock — and specifically changes in gene expression resulting from methylation of cytosine and guanine in the DNA — provides the critical connection between aging in dogs and people. “All available evidence suggests that most biological mechanisms of aging in dogs will be conserved in humans,” Kaeberlein said. “It just happens much faster in dogs.” These methylation changes, called the “methylomes,” have been associated with rates of aging in dogs, humans, and also mice.
In a 2020 study young dogs matched with young adults and aged dogs matched with older adults showed the greatest similarities in methylomes. In the Cell Systems report, Tina Wang of the University of California, San Diego, and colleagues wrote that the methylome “can be used to quantitatively translate the age-related physiology experienced by one organism (i.e., a model species like dog) to the age at which physiology in a second organism is most similar (i.e., a second model or humans).” This allows rates of aging in one species to be mapped onto aging in another species, providing “a compelling tool in the quest to understand aging and identify interventions for maximizing healthy lifespan.”
In the Dog Aging Project study, 8% of 24,238 owners fed their dogs once daily, the same as the percentage of owners serving three daily meals. Twice-daily feedings were most common (73%), and just over 1 in 10 owners (11%) “free fed” their dogs by just filling up the bowl whenever it was empty — most likely Rover’s favorite option.
“The notion of breakfast, lunch, and dinner for people in the United States is not based on large studies that compared three meals a day to two meals a day, or to four, “ said Kate E. Creevy, chief veterinary officer with the Dog Aging Project and associate professor at Texas A&M University. “It’s more about what we are accustomed to. Similarly, there are not large population studies comparing outcomes of dogs fed once, twice, or three times a day.”
“We do not recommend that people change their dogs’ diets based on this report,” Creevy emphasized. “It’s important to understand the difference between research that finds associations versus research that finds cause and effect.”
To establish cause and effect, the Dog Aging Project will follow their cohort over many years. Then, Creevy said, “We will be able to determine whether the associations we have found with feeding frequency are causes, or effects, or neither.”
While not yet actionable, the feeding findings fit with biology across a variety of animals, Kaeberlein said, including indicators that better health translates into longer healthspans. He said that caloric restriction and perhaps time-restricted eating or intermittent fasting — all ways that some human diets are structured — can have a positive impact on the biology of aging by allowing the gastrointestinal tract to have time each day to rest and repair itself, just as sleep benefits the brain through rest.
Timing of meals is also related to the concept of ketogenesis, Kaeberlein explained. Without access to glucose, animals switch over to a ketogenic state in which back-up systems produce energy through metabolic pathways that generate ketones. Mice go into this state very quickly, after a few hours or an overnight fast, while people shift to ketogenesis more slowly, from a few hours to up to 36 hours for people on typical Western diets, Kaeberlein said.
Dogs are different. They take at least two days to shift to ketogenesis, suggesting they have evolved to need fewer meals that are spaced out rather than the multiple daily meals plus snacks that people prefer.
As this relates to longevity, Kaeberlein said that a couple of studies show that mice who are fed a ketogenic diet have longer lifespans (years of life regardless of health). “For us, the next step is to analyze the composition of the dogs’ diets or the relationship of multiple daily feedings with obesity,” he said. “Maybe not being obese is related to better health.”
To learn more, the Dog Aging Project needs dogs — lots of dogs! Kaeberlein wants at least 100,000 dogs, including small dogs, large dogs, dogs of all ages. Puppies are needed for the researchers to follow across their lifespan. The project has an excellent website where owners can volunteer to participate.
Nutritional strategies are often not built around sound scientific principles, Kaeberlein said. In human nutrition, people have tried all kinds of diets over the years, including some that were completely wrong. Kaeberlein and his colleagues in the Dog Aging Project want to change that, at least for people’s canine companions, and hopefully, as a result, give dogs added years of healthy life and provide clues for human nutrition.
After that, maybe they can do something about those sad eyes and the frustrated whine.

