The Skinny on Fat and Covid-19
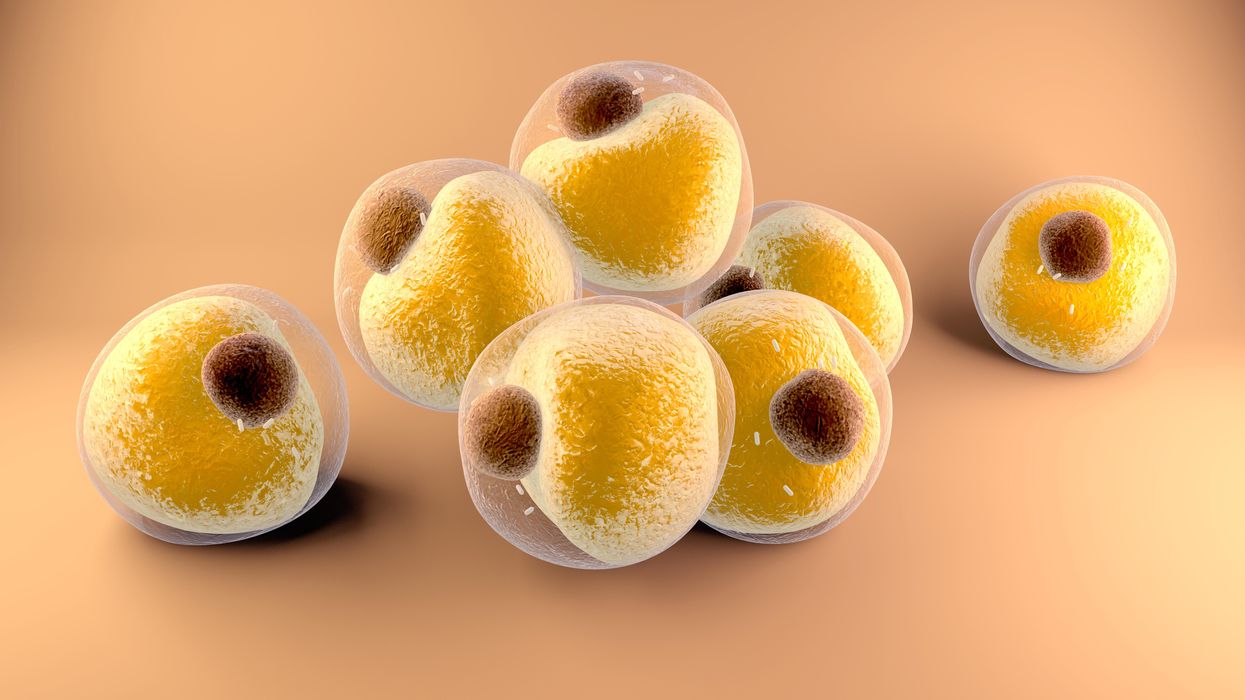
Researchers at Stanford have found that the virus that causes Covid-19 can infect fat cells, which could help explain why obesity is linked to worse outcomes for those who catch Covid-19.
Obesity is a risk factor for worse outcomes for a variety of medical conditions ranging from cancer to Covid-19. Most experts attribute it simply to underlying low-grade inflammation and added weight that make breathing more difficult.
Now researchers have found a more direct reason: SARS-CoV-2, the virus that causes Covid-19, can infect adipocytes, more commonly known as fat cells, and macrophages, immune cells that are part of the broader matrix of cells that support fat tissue. Stanford University researchers Catherine Blish and Tracey McLaughlin are senior authors of the study.
Most of us think of fat as the spare tire that can accumulate around the middle as we age, but fat also is present closer to most internal organs. McLaughlin's research has focused on epicardial fat, “which sits right on top of the heart with no physical barrier at all,” she says. So if that fat got infected and inflamed, it might directly affect the heart.” That could help explain cardiovascular problems associated with Covid-19 infections.
Looking at tissue taken from autopsy, there was evidence of SARS-CoV-2 virus inside the fat cells as well as surrounding inflammation. In fat cells and immune cells harvested from health humans, infection in the laboratory drove "an inflammatory response, particularly in the macrophages…They secreted proteins that are typically seen in a cytokine storm” where the immune response runs amok with potential life-threatening consequences. This suggests to McLaughlin “that there could be a regional and even a systemic inflammatory response following infection in fat.”
It is easy to see how the airborne SARS-CoV-2 virus infects the nose and lungs, but how does it get into fat tissue? That is a mystery and the source of ample speculation.
The macrophages studied by McLaughlin and Blish were spewing out inflammatory proteins, While the the virus within them was replicating, the new viral particles were not able to replicate within those cells. It was a different story in the fat cells. “When [the virus] gets into the fat cells, it not only replicates, it's a productive infection, which means the resulting viral particles can infect another cell,” including microphages, McLaughlin explains. It seems to be a symbiotic tango of the virus between the two cell types that keeps the cycle going.
It is easy to see how the airborne SARS-CoV-2 virus infects the nose and lungs, but how does it get into fat tissue? That is a mystery and the source of ample speculation.
Macrophages are mobile; they engulf and carry invading pathogens to lymphoid tissue in the lymph nodes, tonsils and elsewhere in the body to alert T cells of the immune system to the pathogen. Perhaps some of them also carry the virus through the bloodstream to more distant tissue.
ACE2 receptors are the means by which SARS-CoV-2 latches on to and enters most cells. They are not thought to be common on fat cells, so initially most researchers thought it unlikely they would become infected.
However, while some cell receptors always sit on the surface of the cell, other receptors are expressed on the surface only under certain conditions. Philipp Scherer, a professor of internal medicine and director of the Touchstone Diabetes Center at the University of Texas Southwestern Medical Center, suggests that, in people who have obesity, “There might be higher levels of dysfunctional [fat cells] that facilitate entry of the virus,” either through transiently expressed ACE2 or other receptors. Inflammatory proteins generated by macrophages might contribute to this process.
Another hypothesis is that viral RNA might be smuggled into fat cells as cargo in small bits of material called extracellular vesicles, or EVs, that can travel between cells. Other researchers have shown that when EVs express ACE2 receptors, they can act as decoys for SARS-CoV-2, where the virus binds to them rather than a cell. These scientists are working to create drugs that mimic this decoy effect as an approach to therapy.
Do fat cells play a role in Long Covid? “Fat cells are a great place to hide. You have all the energy you need and fat cells turn over very slowly; they have a half-life of ten years,” says Scherer. Observational studies suggest that acute Covid-19 can trigger the onset of diabetes especially in people who are overweight, and that patients taking medicines to regulate their diabetes “were actually quite protective” against acute Covid-19. Scherer has funding to study the risks and benefits of those drugs in animal models of Long Covid.
McLaughlin says there are two areas of potential concern with fat tissue and Long Covid. One is that this tissue might serve as a “big reservoir where the virus continues to replicate and is sent out” to other parts of the body. The second is that inflammation due to infected fat cells and macrophages can result in fibrosis or scar tissue forming around organs, inhibiting their function. Once scar tissue forms, the tissue damage becomes more difficult to repair.
Current Covid-19 treatments work by stopping the virus from entering cells through the ACE2 receptor, so they likely would have no effect on virus that uses a different mechanism. That means another approach will have to be developed to complement the treatments we already have. So the best advice McLaughlin can offer today is to keep current on vaccinations and boosters and lose weight to reduce the risk associated with obesity.
Will religious people reject organ transplants from pigs?
Scientists are getting better at transplanting pig organs into humans. But religious followers of prohibitions on consuming pork may reject these organs, even if their bodies could accept them.
The first successful recipient of a human heart transplant lived 18 days. The first artificial heart recipient lived just over 100.
Their brief post-transplant lives paved the way toward vastly greater successes. Former Vice President Dick Cheney relied on an artificial heart for nearly two years before receiving a human heart transplant. It still beats in his chest more than a decade later.
Organ transplantation recently reached its next phase with David Bennett. He survived for two months after becoming the first recipient of a pig’s heart genetically modified to function in a human body in February. Known as a xenotransplant, the procedure could pave the way for greatly expanding the use of transplanted vital organs to extend human lives.
Clinical trials would have to be held in the U.S. before xenotransplants become widespread; Bennett’s surgery was authorized under a special Food and Drug Administration program that addresses patients with life-threatening medical conditions.
German researchers plan to perform eight pig-to-human heart transplants as part of a clinical trial beginning in 2024. According to an email sent to Leaps.org by three scholars working on the German project, these procedures will focus on one of the reasons David Bennett did not survive longer: A porcine infection from his new heart.
The transplant team will conduct more sensitive testing of the donor organs, “which in all likelihood will be able to detect even low levels of virus in the xenograft,” note the scientists, Katharina Ebner, Jochen Ostheimer and Jochen Sautermeister. They are confident that the risk of infection with a porcine virus in the future will be significantly lower.
Moreover, hearts are not the only genetically modified organs that are being xenotransplanted. A team of surgeons at the University of Alabama at Birmingham successfully transplanted genetically modified pig kidneys into a brain-dead human recipient in September. The kidneys functioned normally for more than three days before the experiment ended. The UAB team is now moving forward with clinical trials focusing on transplanting pig kidneys into human patients.
Some experts believe the momentum for xenotransplantation is building, particularly given the recent successes. “I think there is a strong likelihood this will go mainstream,” says Brendan Parent of NYU Langone Health.
Douglas Anderson, a surgeon who is part of that kidney xenotransplant team, observes that, “organ shortages have been the major issue facing transplantation since its inception” and that xenotransplantation is a potential solution to that quandary. “It can’t be understated the number of people waiting for a kidney on dialysis, which has a significant mortality rate,” he says. According to the advocacy group Donate Life America, more than 100,000 people in the U.S. alone are waiting for a donated organ, and 85 percent of them need a kidney.
Other experts believe the momentum for xenotransplantation is building, particularly given the recent successes. “I think there is a strong likelihood this will go mainstream,” says Brendan Parent, director of transplant ethics and policy at NYU Langone Health, a New York City-based hospital system. Like the UAB team, surgeons at NYU Langone have had success coaxing modified pig kidneys to work in deceased humans.
“There is a genuinely good chance that within a generation, (xenotransplantation) might become very common in reasonably wealthy countries,” says Michael Reiss, professor of science education at University College in London. In addition to his academic position, Reiss sits on the Nuffield Council on Bioethics, a nonprofit that is one of Britain’s most prominent watchdogs regarding medical and scientific issues. Reiss is also an Anglican priest and has studied xenotransplantation from both a scientific and religious point of view.
Moreover, genetic modifications could one day lead to organs being specifically optimized for their recipients. That could ensure issues like donor rejection and the calculated risk of artificially suppressing recipient immune systems become concerns of the past.
Major bioethical, religious concerns
Despite the promise of xenotransplantation, numerous bioethical issues swirl around the procedure. They could be magnified if xenotransplantation evolves from one-off experiments to a routine medical procedure.
One of the biggest is the millennia-long prohibitions Islam and Judaism have had regarding the consumption of pork. Will followers of these religions assume such rules extend to those taboo materials being inserted into a human body?
“Initially, one’s instinctual reaction is that, oh, crumbs! – how are Jews and Muslims going to react to that?” Reiss says. But in a world where science and secularism are accepted on an everyday basis, he notes it is not a significant issue. Reiss points out that valves from pig hearts have been used in human patients for decades without any issues. He adds that both Islam and Judaism waive religious dietary restrictions if a human life is at risk.
“While nobody's saying an individual patient is to be forced to have these, the very high proportion of people who identify as Jews or Muslims when given this option are content with it,” he says.
Concurring with Reiss is Michael Gusamano, professor of health policy at Lehigh University and director of its Center for Ethics. He is currently performing research on the ethics of xenotransplantation for the National Institutes of Health.
“Leaders from all major religions have commented on this and have indicated that this is not inconsistent with religious doctrine,” Gusamano says in written remarks to Leaps.org. “Having said that, it is plausible to believe that some people will assume that this is inconsistent with the teaching of their religion and may object to…receiving a xenotransplant as part of routine medical care.”
A history of clashes
Despite those assurances, science has long clashed with theology. Although Galileo proved the planets revolved around the sun, the Catholic Church found him guilty of heresy and rewarded his discovery with house arrest for the last decade of his life. A revolt occurred in mid-19th century India after native-born soldiers believed the ammunition supplied by their British occupiers had been lubricated with pork and beef tallow. Given they had to use their mouths to tear open ammunition pouches, this violated both the tenets of Islam and Hinduism. And one of the conspiracy theories hatched as a result of COVID-19 was that the vaccines developed to fight the disease were the “mark of the beast” – a sign of impending Armageddon under evangelical Christian theology.
The German xenotransplant research team has encountered such potential concerns when the procedure is regarded through a religious lens. “The pastors in our research suspected that many recipients might feel disgust and revulsion,” they write. “Even beyond these special religious reservations, cultural scripts about pigs as inferior living beings are also generally widespread and effective in the western world, so that here too possible disgust reactions cannot be ruled out.”
The German researchers add that “Jewish and Muslim hospital pastoral workers believe possible considerable problems in this respect, which must be dealt with psychosocially, religiously, and pastorally prior to a possible transplantation in order to strengthen the acceptance of the received organ by the patients and their relatives.”
Parent, the director at NYU Langone, shares a concern that xenotransplantation could move “too fast,” although much of his worry is focused on zoonotic disease transmission – pig viruses jumping into humans as a result of such procedures.
Another ethical issue
Moreover, the way pigs and other animals are raised for transplants could pose future ethical dilemmas.
Reiss notes that pigs raised for medical procedures have to be grown and kept in what are known as a designated pathogen-free facility, or DPF. Such facilities are kept painstakingly antiseptic so as to minimize the risk of zoonotic transmissions. But given pigs are fond of outdoor activities such as wallowing in mud and sleeping on hay, they lead “stunningly boring lives” that they probably do not enjoy, Reiss observes.
Ethical concerns with using pigs may push transplantation medicine into its next logical phase: Growing functional organs for transplant in a laboratory setting.
“There’s no doubt that these research pigs have gotten much better veterinary care, et cetera, (compared to farmed pigs). But it’s not a great life,” Reiss says. “And although it hasn’t so far dominated the discussion, I think as the years go by, rather as we’ve seen with the use of apes and now monkeys in medical research, more and more theologians will get uncomfortable about us just assuming we can do this with…pigs.”
The German research team raises the same concerns, but has taken a fairly sanguine view on the topic. “The impairments of the species-typical behavior will certainly provoke criticism and perhaps also public protest. But the number of animals affected is very small in relation to slaughter cattle,” the German researchers note. “Moreover, the conditions there and also in several animal experiments are far worse.”
Observers say that may push transplantation medicine into its next logical phase: Growing functional organs for transplant in a laboratory setting. Anderson, the UAB transplant surgeon, believes such an accomplishment remains decades away.
But other experts believe there is a moral imperative that xenotransplantation remain a temporary solution. “I think we have a duty to go in that direction,” Parent says. “We have to go that way, with the xenotransplantation process (as) a steppingstone and research path that will be useful for bioengineered organs.”
The Friday Five: Scientists treated this girl's disease before she was born
In this week's Friday Five, scientists treated this girl's rare diseases in utero. Plus, how to lift weights in half the time, electric shocks help people regain the ability to walk, meditation is found to work as well as medication, and much more.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Here are the promising studies covered in this week's Friday Five:
- Kids treated for diseases before they're born
- How to lift weights in half the time
- Electric shocks help people regain the ability to walk
- Meditation just as good as medication?
- These foods could pump up your motivation

