One of the World’s Most Hated Plants Is Becoming a Public Health Rock Star

A plant in a growth chamber.
The recent Ebola virus outbreak in the Democratic Republic of Congo has refocused attention on the vaccine and treatment prospects for the highly contagious and deadly disease. As of late May, more than 7,500 doses of an experimental vaccine made by Merck Pharmaceuticals had been shipped to the beleaguered African nation, according to a World Health Organization press release.
Research was focused on the production of antibodies and vaccines in a novel manufacturing system: the tobacco plant.
Meanwhile, Ebola treatments were also sent. One of these, ZMapp, was successfully used to treat two American missionaries in Liberia in 2014. Charles Arntzen, who helped develop the treatment, calls that moment the highlight of his career: "It started in a lab as a fanciful idea that needed to be validated. In ten years, it was being used and people went from almost dead to almost recovered."
His initial research was focused on the production of antibodies and vaccines in a novel manufacturing system. That system was the tobacco plant—not the smoking variety, or nicotiana tabacum. But rather, a distant cousin called nicotiana benthamiana, which is native to Australia, where it grows abundantly.
ZMapp is made from the plant, as are other therapeutics and vaccines. Indeed, the once-maligned plant family has turned its image upside down in the public health world, now holding promise to prevent and treat many conditions.
Cheap, easy and plentiful
Research on the tobacco plant's medicinal potential goes back a few decades. In the early 1990s, research on plants as vaccine production platforms was just beginning. "We wanted to make a lower-cost vaccine manufacturing system to be used in developing countries to broaden our manufacturing base in the developing world," said Arntzen, who is the founding director of the Biodesign Center for Immunotherapy, Vaccines and Virotherapy at Arizona State University. "There was and still is a shortage of vaccines in the poorest countries."
"I've got a list of about fifty vaccines that should be made in tobacco."
Initially, research focused on food plants: bananas, tomatoes, and potatoes. While these efforts were successful, they were stymied by the "anti-GMO food establishment," Arntzen said. "I didn't want to spend my time fighting." So, they switched to the tobacco plant.
"I've got a list of about fifty vaccines that should be made in tobacco," said Denis Murphy, professor of biotechnology at the University of South Wales. "We know a lot about how to express genes in tobacco and get it made."
Unlike egg-based vaccines, which require a clean, sterile laboratory to make, and can therefore be an expensive process, Murphy said, tobacco-based vaccines are relatively cheap to make. The process is simple: Three weeks after being planted, the plants are dipped into a liquid containing proteins from the given virus. The plants grow the proteins for another week and then are harvested and chopped up. The green liquid that results is the vaccine, which is purified and then bottled up in precise doses.
"The tobacco plant doesn't seem to mind making all this foreign protein," Murphy added. "The plants will stay alive and look okay, and they will be full of vaccine protein. If you did this with an animal, you'd probably kill it."
Still, there are certain challenges to producing tobacco-based vaccines, particularly in the developing world, said Murphy, who is also a biotech consultant for the Food and Agricultural Organization of the United Nations.
"The purification process of the vaccine protein from leaves is still something for which you need a specialized lab. You couldn't have that in the Congo," he said. Security is another concern. "Someone could steal the plant and grow it themselves as a pirate version."
Even birds could be the culprit for tobacco plant theft. "What if a bird came and started eating the leaves? You might want netting or greenhouse growing. That can be much more problematic in a developing country."
While the ZMapp treatment for Ebola is produced from tobacco, efforts to develop a vaccine this way have not proved fruitful so far. (Merck's Ebola vaccine is made from livestock.) "Our tobacco-based vaccine would require three doses for a full effect, while the vaccine made by Merck may only require a single dose," Arntzen said. "Having to give three doses, over about a month, makes the tobacco-made vaccine much more cumbersome and expensive to deliver." Yet a tobacco-derived vaccine for another newsworthy illness is in the works.
On the frontier of a flu vaccine
Quebec City-based biopharmaceutical company Medicago is using a novel technique to make a flu vaccine with tobacco. This offers several advantages over the current method of developing the vaccine from eggs.
First of all, the production is quicker: five to six weeks, versus four to six months, which means that researchers can wait to identify the circulating flu strain for the upcoming season, rather than guess and risk being wrong.
Also, with tobacco, developers can use something called virus-like particles, instead of the actual flu virus.
"We hope to be on the market by the 2020/21 flu season."
"They have the structure of the flu virus, but not its full genetic code, so the virus doesn't replicate," said Anne Shiraishi, Medicago's communications manager. That's a big deal because the flu is a rapidly mutating virus, and traditional egg-based vaccines encourage those mutations – which wind up making the vaccines less effective.
This problem happens because the flu virus mutates a key protein to better attach to receptors in bird cells, but in humans, this mutation won't trigger an effective immune response, according to a Medicago fact sheet. That's why some people who have been vaccinated still get the flu. Indeed, the 2017 flu season had the lowest vaccine effectiveness record ever for H3N2 at 10 percent in the Southern Hemisphere, and 0 percent effective in the EU and UK in people over age 65. At least theoretically, their tobacco-derived flu vaccine could be far more successful, since no such mutations occur with the virus-like particles.
Last year, Medicago, which is 40 percent owned by cigarette company Philip Morris, began a phase 3 trial of the flu vaccine with 10,000 subjects in five countries: half are getting the vaccine, and half are getting a placebo. "We hope to announce really good results this fall," Shiraishi said. "We hope to be on the market by the 2020/21 flu season."
They're also preparing phase I trials for vaccines for the rotavirus and norovirus, two intractable gastro-intestinal viruses. They hope to roll those trials out in the next year or two.
Meanwhile, other research on antibodies is in their pipeline—all of it using tobacco, Shiraishi said. "We've taken something bad for public health and made it our mini factories."
Jamie Rettinger with his now fiance Amie Purnel-Davis, who helped him through the clinical trial.
Jamie Rettinger was still in his thirties when he first noticed a tiny streak of brown running through the thumbnail of his right hand. It slowly grew wider and the skin underneath began to deteriorate before he went to a local dermatologist in 2013. The doctor thought it was a wart and tried scooping it out, treating the affected area for three years before finally removing the nail bed and sending it off to a pathology lab for analysis.
"I have some bad news for you; what we removed was a five-millimeter melanoma, a cancerous tumor that often spreads," Jamie recalls being told on his return visit. "I'd never heard of cancer coming through a thumbnail," he says. None of his doctors had ever mentioned it either. "I just thought I was being treated for a wart." But nothing was healing and it continued to bleed.
A few months later a surgeon amputated the top half of his thumb. Lymph node biopsy tested negative for spread of the cancer and when the bandages finally came off, Jamie thought his medical issues were resolved.
Melanoma is the deadliest form of skin cancer. About 85,000 people are diagnosed with it each year in the U.S. and more than 8,000 die of the cancer when it spreads to other parts of the body, according to the Centers for Disease Control and Prevention (CDC).
There are two peaks in diagnosis of melanoma; one is in younger women ages 30-40 and often is tied to past use of tanning beds; the second is older men 60+ and is related to outdoor activity from farming to sports. Light-skinned people have a twenty-times greater risk of melanoma than do people with dark skin.
"When I graduated from medical school, in 2005, melanoma was a death sentence" --Diwakar Davar.
Jamie had a follow up PET scan about six months after his surgery. A suspicious spot on his lung led to a biopsy that came back positive for melanoma. The cancer had spread. Treatment with a monoclonal antibody (nivolumab/Opdivo®) didn't prove effective and he was referred to the UPMC Hillman Cancer Center in Pittsburgh, a four-hour drive from his home in western Ohio.
An alternative monoclonal antibody treatment brought on such bad side effects, diarrhea as often as 15 times a day, that it took more than a week of hospitalization to stabilize his condition. The only options left were experimental approaches in clinical trials.
Early research
"When I graduated from medical school, in 2005, melanoma was a death sentence" with a cure rate in the single digits, says Diwakar Davar, 39, an oncologist at UPMC Hillman Cancer Center who specializes in skin cancer. That began to change in 2010 with introduction of the first immunotherapies, monoclonal antibodies, to treat cancer. The antibodies attach to PD-1, a receptor on the surface of T cells of the immune system and on cancer cells. Antibody treatment boosted the melanoma cure rate to about 30 percent. The search was on to understand why some people responded to these drugs and others did not.
At the same time, there was a growing understanding of the role that bacteria in the gut, the gut microbiome, plays in helping to train and maintain the function of the body's various immune cells. Perhaps the bacteria also plays a role in shaping the immune response to cancer therapy.
One clue came from genetically identical mice. Animals ordered from different suppliers sometimes responded differently to the experiments being performed. That difference was traced to different compositions of their gut microbiome; transferring the microbiome from one animal to another in a process known as fecal transplant (FMT) could change their responses to disease or treatment.
When researchers looked at humans, they found that the patients who responded well to immunotherapies had a gut microbiome that looked like healthy normal folks, but patients who didn't respond had missing or reduced strains of bacteria.
Davar and his team knew that FMT had a very successful cure rate in treating the gut dysbiosis of Clostridioides difficile, a persistant intestinal infection, and they wondered if a fecal transplant from a patient who had responded well to cancer immunotherapy treatment might improve the cure rate of patients who did not originally respond to immunotherapies for melanoma.
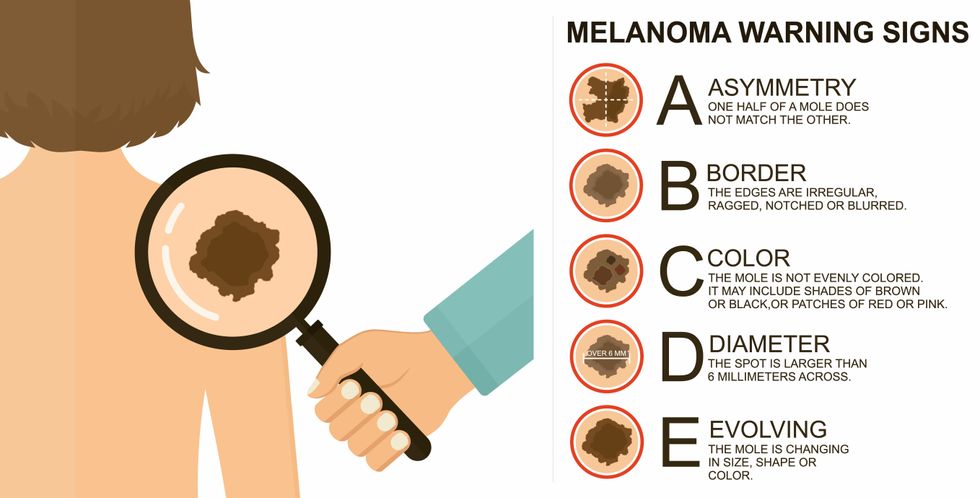
The ABCDE of melanoma detection
Adobe Stock
Clinical trial
"It was pretty weird, I was totally blasted away. Who had thought of this?" Jamie first thought when the hypothesis was explained to him. But Davar's explanation that the procedure might restore some of the beneficial bacterial his gut was lacking, convinced him to try. He quickly signed on in October 2018 to be the first person in the clinical trial.
Fecal donations go through the same safety procedures of screening for and inactivating diseases that are used in processing blood donations to make them safe for transfusion. The procedure itself uses a standard hollow colonoscope designed to screen for colon cancer and remove polyps. The transplant is inserted through the center of the flexible tube.
Most patients are sedated for procedures that use a colonoscope but Jamie doesn't respond to those drugs: "You can't knock me out. I was watching them on the TV going up my own butt. It was kind of unreal at that point," he says. "There were about twelve people in there watching because no one had seen this done before."
A test two weeks after the procedure showed that the FMT had engrafted and the once-missing bacteria were thriving in his gut. More importantly, his body was responding to another monoclonal antibody (pembrolizumab/Keytruda®) and signs of melanoma began to shrink. Every three months he made the four-hour drive from home to Pittsburgh for six rounds of treatment with the antibody drug.
"We were very, very lucky that the first patient had a great response," says Davar. "It allowed us to believe that even though we failed with the next six, we were on the right track. We just needed to tweak the [fecal] cocktail a little better" and enroll patients in the study who had less aggressive tumor growth and were likely to live long enough to complete the extensive rounds of therapy. Six of 15 patients responded positively in the pilot clinical trial that was published in the journal Science.
Davar believes they are beginning to understand the biological mechanisms of why some patients initially do not respond to immunotherapy but later can with a FMT. It is tied to the background level of inflammation produced by the interaction between the microbiome and the immune system. That paper is not yet published.
Surviving cancer
It has been almost a year since the last in his series of cancer treatments and Jamie has no measurable disease. He is cautiously optimistic that his cancer is not simply in remission but is gone for good. "I'm still scared every time I get my scans, because you don't know whether it is going to come back or not. And to realize that it is something that is totally out of my control."
"It was hard for me to regain trust" after being misdiagnosed and mistreated by several doctors he says. But his experience at Hillman helped to restore that trust "because they were interested in me, not just fixing the problem."
He is grateful for the support provided by family and friends over the last eight years. After a pause and a sigh, the ruggedly built 47-year-old says, "If everyone else was dead in my family, I probably wouldn't have been able to do it."
"I never hesitated to ask a question and I never hesitated to get a second opinion." But Jamie acknowledges the experience has made him more aware of the need for regular preventive medical care and a primary care physician. That person might have caught his melanoma at an earlier stage when it was easier to treat.
Davar continues to work on clinical studies to optimize this treatment approach. Perhaps down the road, screening the microbiome will be standard for melanoma and other cancers prior to using immunotherapies, and the FMT will be as simple as swallowing a handful of freeze-dried capsules off the shelf rather than through a colonoscopy. Earlier this year, the Food and Drug Administration approved the first oral fecal microbiota product for C. difficile, hopefully paving the way for more.
An older version of this hit article was first published on May 18, 2021
All organisms can repair damaged tissue, but none do it better than salamanders and newts. A surprising area of science could tell us how they manage this feat - and perhaps even help us develop a similar ability.
All organisms have the capacity to repair or regenerate tissue damage. None can do it better than salamanders or newts, which can regenerate an entire severed limb.
That feat has amazed and delighted man from the dawn of time and led to endless attempts to understand how it happens – and whether we can control it for our own purposes. An exciting new clue toward that understanding has come from a surprising source: research on the decline of cells, called cellular senescence.
Senescence is the last stage in the life of a cell. Whereas some cells simply break up or wither and die off, others transition into a zombie-like state where they can no longer divide. In this liminal phase, the cell still pumps out many different molecules that can affect its neighbors and cause low grade inflammation. Senescence is associated with many of the declining biological functions that characterize aging, such as inflammation and genomic instability.
Oddly enough, newts are one of the few species that do not accumulate senescent cells as they age, according to research over several years by Maximina Yun. A research group leader at the Center for Regenerative Therapies Dresden and the Max Planck Institute of Molecular and Cell Biology and Genetics, in Dresden, Germany, Yun discovered that senescent cells were induced at some stages of regeneration of the salamander limb, “and then, as the regeneration progresses, they disappeared, they were eliminated by the immune system,” she says. “They were present at particular times and then they disappeared.”
Senescent cells added to the edges of the wound helped the healthy muscle cells to “dedifferentiate,” essentially turning back the developmental clock of those cells into more primitive states.
Previous research on senescence in aging had suggested, logically enough, that applying those cells to the stump of a newly severed salamander limb would slow or even stop its regeneration. But Yun stood that idea on its head. She theorized that senescent cells might also play a role in newt limb regeneration, and she tested it by both adding and removing senescent cells from her animals. It turned out she was right, as the newt limbs grew back faster than normal when more senescent cells were included.
Senescent cells added to the edges of the wound helped the healthy muscle cells to “dedifferentiate,” essentially turning back the developmental clock of those cells into more primitive states, which could then be turned into progenitors, a cell type in between stem cells and specialized cells, needed to regrow the muscle tissue of the missing limb. “We think that this ability to dedifferentiate is intrinsically a big part of why salamanders can regenerate all these very complex structures, which other organisms cannot,” she explains.
Yun sees regeneration as a two part problem. First, the cells must be able to sense that their neighbors from the lost limb are not there anymore. Second, they need to be able to produce the intermediary progenitors for regeneration, , to form what is missing. “Molecularly, that must be encoded like a 3D map,” she says, otherwise the new tissue might grow back as a blob, or liver, or fin instead of a limb.
Wound healing
Another recent study, this time at the Mayo Clinic, provides evidence supporting the role of senescent cells in regeneration. Looking closely at molecules that send information between cells in the wound of a mouse, the researchers found that senescent cells appeared near the start of the healing process and then disappeared as healing progressed. In contrast, persistent senescent cells were the hallmark of a chronic wound that did not heal properly. The function and significance of senescence cells depended on both the timing and the context of their environment.
The paper suggests that senescent cells are not all the same. That has become clearer as researchers have been able to identify protein markers on the surface of some senescent cells. The patterns of these proteins differ for some senescent cells compared to others. In biology, such physical differences suggest functional differences, so it is becoming increasingly likely there are subsets of senescent cells with differing functions that have not yet been identified.
There are disagreements within the research community as to whether newts have acquired their regenerative capacity through a unique evolutionary change, or if other animals, including humans, retain this capacity buried somewhere in their genes.
Scientists initially thought that senescent cells couldn’t play a role in regeneration because they could no longer reproduce, says Anthony Atala, a practicing surgeon and bioengineer who leads the Wake Forest Institute for Regenerative Medicine in North Carolina. But Yun’s study points in the other direction. “What this paper shows clearly is that these cells have the potential to be involved in tissue regeneration [in newts]. The question becomes, will these cells be able to do the same in humans.”
As our knowledge of senescent cells increases, Atala thinks we need to embrace a new analogy to help understand them: humans in retirement. They “have acquired a lot of wisdom throughout their whole life and they can help younger people and mentor them to grow to their full potential. We're seeing the same thing with these cells,” he says. They are no longer putting energy into their own reproduction, but the signaling molecules they secrete “can help other cells around them to regenerate.”
There are disagreements within the research community as to whether newts have acquired their regenerative capacity through a unique evolutionary change, or if other animals, including humans, retain this capacity buried somewhere in their genes. If so, it seems that our genes are unable to express this ability, perhaps as part of a tradeoff in acquiring other traits. It is a fertile area of research.
Dedifferentiation is likely to become an important process in the field of regenerative medicine. One extreme example: a lab has been able to turn back the clock and reprogram adult male skin cells into female eggs, a potential milestone in reproductive health. It will be more difficult to control just how far back one wishes to go in the cell's dedifferentiation – part way or all the way back into a stem cell – and then direct it down a different developmental pathway. Yun is optimistic we can learn these tricks from newts.
Senolytics
A growing field of research is using drugs called senolytics to remove senescent cells and slow or even reverse disease of aging.
“Senolytics are great, but senolytics target different types of senescence,” Yun says. “If senescent cells have positive effects in the context of regeneration, of wound healing, then maybe at the beginning of the regeneration process, you may not want to take them out for a little while.”
“If you look at pretty much all biological systems, too little or too much of something can be bad, you have to be in that central zone” and at the proper time, says Atala. “That's true for proteins, sugars, and the drugs that you take. I think the same thing is true for these cells. Why would they be different?”
Our growing understanding that senescence is not a single thing but a variety of things likely means that effective senolytic drugs will not resemble a single sledge hammer but more a carefully manipulated scalpel where some types of senescent cells are removed while others are added. Combinations and timing could be crucial, meaning the difference between regenerating healthy tissue, a scar, or worse.

