Parkinson’s Disease Destroyed My Life. Then I Tried Deep Brain Stimulation.

Anne, Stan, and grandson Louie during vacation in Mexico, 2019. INSET: Anne post-op in 2017.
[Editor's Note: On June 6, 2017, Anne Shabason, an artist, hospice educator, and mother of two from Bolton, Ontario, a small town about 30 miles outside of Toronto, underwent Deep Brain Stimulation (DBS) to treat her Parkinson's disease. The FDA approved DBS for Parkinson's disease in 2002. Although it's shown to be safe and effective, agreeing to invasive brain surgery is no easy decision, even when you have your family and one of North America's premier neurosurgeons at your side.
Here, with support from Stan, her husband of the past 40 years, Anne talks about her life before Parkinson's, what the disease took away, and what she got back because of DBS. As told to writer Heather R. Johnson.]
I was an artist.
I worked in mixed media, Papier-mâché, and collage, inspired by dreams, birds, mystery. I had gallery shows and participated in studio tours.
Educated in thanatology, I worked in hospice care as a volunteer and education director for Hospice Caledon, an organization that supports people facing life-limiting illness and grief.
I trained volunteers who helped people through their transition.
Parkinson's disease changed all that.
My hands and my head were not coordinating, so it was impossible to do my art.
It started as a twitch in my leg. During a hospice workshop, my right leg started vibrating in a way I hadn't experienced before. I told a friend, "This can't be good."
Over the next year, my right foot vibrated more and more. I could not sleep well. In my dreams people lurked in corners, in dark places, and behind castle doors. I knew they were there and couldn't avoid the ambush. I shrieked and woke everyone in the house.
An anxiety attack—something I had also never experienced before—came next.
During a class I was teaching, my mouth got so dry, I couldn't speak. I stood in front of the class for three or four minutes, unable to continue. I pushed through and finished the class. That's when I realized this was more than jiggling legs.
That's when I went to see a doctor.
A Diagnosis
My first doctor, when I suggested it might be Parkinson's, didn't believe me. She sent me to a neurologist who told me I had to meditate more and calm myself.
A friend from hospice told me to phone the Toronto Western Hospital Movement Disorders Clinic. In January 2010, I was diagnosed with Parkinson's disease.
The doctor, a fellow, got all my stats and asked a lot of questions. He was so excited he knew what it was, he exclaimed, "You've got Parkinson's!" like it was the best thing ever. I must say, that wasn't the best news, but at least I finally had a diagnosis.
I could choose whether to take medication or not. The doctor said, "If Parkinson's is compromising your lifestyle, you should consider taking levodopa."
"Well I can't run my classes, I can't do my art, so it's compromising me," I said. And my health was going downhill. The shaking—my whole body moved—sleeping was horrible. Two to four hours max a night was usual. I had terrible anxiety and panic attacks and had to quit work.
So I started taking levodopa. It's taken in a four-hour cycle, but the medication didn't last the full time. I developed dyskenisia, a side effect of the medication that made me experience uncontrolled, involuntary movements. I was edgy, irritable, and focused on my watch like a drug addict. I'd lie on the couch, feel crummy and tired, and wait.
The medication cycle restricted where I could go. Fearing the "off" period, I avoided interaction with lifelong friends, which increased my feeling of social isolation. They would come over and cook with me and read to me sometimes, and that was fine, as long as it was during an "on" period.
There was incontinence, constipation, and fatigue.
I lost fine motor skills, like writing. And painting. My hands and my head were not coordinating, so it was impossible to do my art.
It was a terrible time.
The worst symptoms—what pushed me to consider DBS—were the symptoms no one could see. The anxiety and depression were so bad, the sleeplessness, not eating.
I projected a lot of my discomforts onto Stan. I reacted so badly to him. I actually separated from him briefly on two separate occasions and lived in a separate space—a self-imposed isolation. There wasn't anything he could do to help me really except sit back and watch.
I tried alternative therapies—a naturopath, an osteopath, a reflexologist and a Chinese medicine practitioner—but nothing seemed to help.
I felt like I was dying. Certain parts of my life were being taken away from me. I was a perfectionist, and I felt imperfect. It was a horrible feeling, to not be in control of myself.
The DBS Decision
I was familiar with DBS, a procedure that involves a neurosurgeon drilling small holes into your skull and implanting electrical leads deep in your brain to modify neural activity, reducing involuntary movements.
But I was convinced I'd never do it. I was brought up in a family that believed 'doctors make you sick and hospitals kill you.'
I worried the room wouldn't be sterile. Someone's cutting into your brain, you don't know what's going to happen. They're putting things in your body. I didn't want to risk possible infection.
And my doctor said he couldn't promise he would actually do the operation. It might be a fellow, but he'd be in the background in case anything went wrong. I wasn't comfortable with that arrangement.
When filmmakers Taryn Southern and Elena Gaby decided to make a documentary about people whose lives were changed by cutting-edge brain implants--and I agreed to participate—my doctor said he would for sure do the operation. They couldn't risk anything happening on the operating table on camera, so most of my fears went away.
My family supported the decision. My mother had trigeminal neuralgia, which is a very painful facial condition. She also had a stroke and what we now believe to be Parkinson's. My father, a retired dentist, managed her care and didn't give her the opportunity to see a specialist.
I felt them running the knife across my scalp, and drilling two holes in my head, but only as pressure, not pain.
When we were talking about DBS, my son, Joseph, said, "How can you not do this, for the sake of your family? Because if you don't, you'll end up like Grandma, who, for the last few years of her life, just lay on a couch because she didn't get any kind of outside help. If you even have a chance to improve your life or give yourself five extra years, why wouldn't you do that, for our sake? Are we not worth that?"
That talk really affected me, and I realized I had to try. Even though it was difficult, I had to be brave for my family.
Surgery, Recovery, and Tweaking
You have to be awake for part of the procedure—I was awake enough that my subconscious could hear, because they had to know how far to insert the electrodes. DBS targets the troublemaking areas of the brain. There's a one millimeter difference between success and failure.
I felt them running the knife across my scalp, and drilling two holes in my head, but only as pressure, not pain.
Once they were inside, they asked me to move parts of my body to see whether the right neurons were activated.
They put me to sleep to put a battery-powered neurostimulator in my chest. A wire that runs behind my ear and down my neck connects the electrodes in my brain to the battery pack. The neurostimulator creates electric pulses 24 hours a day.
I was moving around almost immediately after surgery. Recovery from the stitches took a few weeks, but everything else took a lot longer.
I couldn't read. My motor skills were still impaired, and my brain and my hands weren't yet linked up. I needed the device to be programmed and tweaked. Until that happened, I needed help.
The depression and anxiety, though, went away almost immediately. From that perspective, it was like I never had Parkinson's. I was so happy.
When they calibrated the electrodes, they adjusted how much electrical current goes to any one of four contact points on the left and right sides of the brain. If they increased it too much, a leg would start shaking, a foot would start cramping, or my tongue would feel thicker. It took a while to get it calibrated correctly to control the symptoms.
First it was five sessions in five weeks, then once a month, then every three months. Now I visit every six months. As the disease progresses, they have the ability to keep making adjustments. (DBS controls the symptoms, but it doesn't cure the disease.)
Once they got the calibration right, my motor skills improved. I could walk without shuffling. My muscles weren't stiff and aching, and the dyskinesia disappeared. But if I turn off the device, my symptoms return almost immediately.
Some days I have more fatigue than others, and sometimes my brain doesn't click. And my voice got softer – that's a common side effect of this operation. But I'm doing so much better than before.
I have a quality of life I didn't have before. Before COVID-19 hit, Stan and I traveled, went to concerts, movies, galleries, and spent time with our growing family.
I cut back the levodopa from seven-and-a-half pills a day to two-and-a-half. I often forget to take my medication until I realize I'm feeling tired or anxious.
Best of all, my motivation and creative ability have clicked in.
I am an artist—again.
I'm painting every day. It's what is keeping me sane. It's my saving grace.
I'm not perfect. But I am Anne. Again.
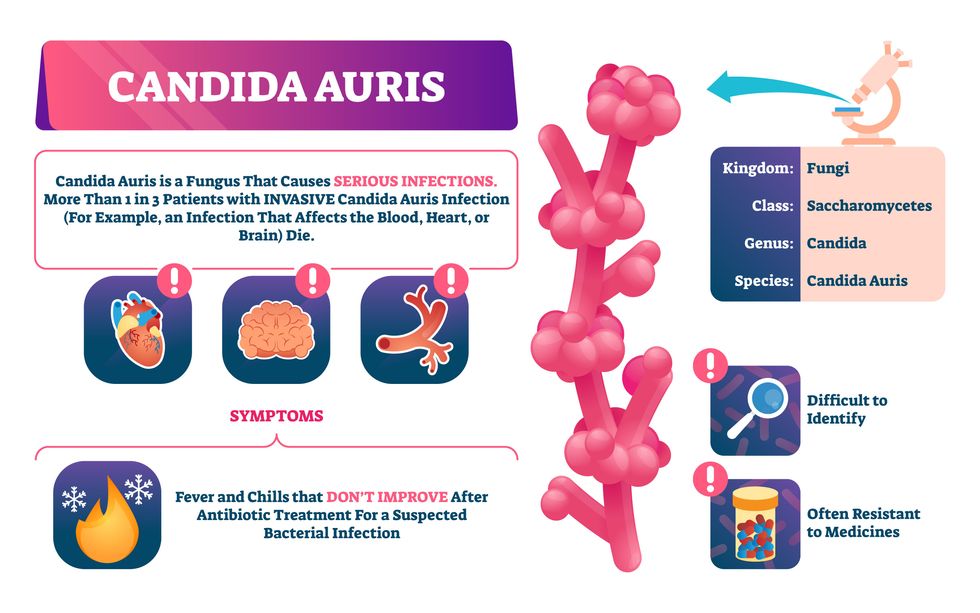
Doctors worry that fungal pathogens may cause the next pandemic.
Bacterial antibiotic resistance has been a concern in the medical field for several years. Now a new, similar threat is arising: drug-resistant fungal infections. The Centers for Disease Control and Prevention considers antifungal and antimicrobial resistance to be among the world’s greatest public health challenges.
One particular type of fungal infection caused by Candida auris is escalating rapidly throughout the world. And to make matters worse, C. auris is becoming increasingly resistant to current antifungal medications, which means that if you develop a C. auris infection, the drugs your doctor prescribes may not work. “We’re effectively out of medicines,” says Thomas Walsh, founding director of the Center for Innovative Therapeutics and Diagnostics, a translational research center dedicated to solving the antimicrobial resistance problem. Walsh spoke about the challenges at a Demy-Colton Virtual Salon, one in a series of interactive discussions among life science thought leaders.
Although C. auris typically doesn’t sicken healthy people, it afflicts immunocompromised hospital patients and may cause severe infections that can lead to sepsis, a life-threatening condition in which the overwhelmed immune system begins to attack the body’s own organs. Between 30 and 60 percent of patients who contract a C. auris infection die from it, according to the CDC. People who are undergoing stem cell transplants, have catheters or have taken antifungal or antibiotic medicines are at highest risk. “We’re coming to a perfect storm of increasing resistance rates, increasing numbers of immunosuppressed patients worldwide and a bug that is adapting to higher temperatures as the climate changes,” says Prabhavathi Fernandes, chair of the National BioDefense Science Board.
Most Candida species aren’t well-adapted to our body temperatures so they aren’t a threat. C. auris, however, thrives at human body temperatures.
Although medical professionals aren’t concerned at this point about C. auris evolving to affect healthy people, they worry that its presence in hospitals can turn routine surgeries into life-threatening calamities. “It’s coming,” says Fernandes. “It’s just a matter of time.”
An emerging global threat
“Fungi are found in the environment,” explains Fernandes, so Candida spores can easily wind up on people’s skin. In hospitals, they can be transferred from contact with healthcare workers or contaminated surfaces. Most Candida species aren’t well-adapted to our body temperatures so they aren’t a threat. C. auris, however, thrives at human body temperatures. It can enter the body during medical treatments that break the skin—and cause an infection. Overall, fungal infections cost some $48 billion in the U.S. each year. And infection rates are increasing because, in an ironic twist, advanced medical therapies are enabling severely ill patients to live longer and, therefore, be exposed to this pathogen.
The first-ever case of a C. auris infection was reported in Japan in 2009, although an analysis of Candida samples dated the earliest strain to a 1996 sample from South Korea. Since then, five separate varieties – called clades, which are similar to strains among bacteria – developed independently in different geographies: South Asia, East Asia, South Africa, South America and, recently, Iran. So far, C. auris infections have been reported in 35 countries.
In the U.S., the first infection was reported in 2016, and the CDC started tracking it nationally two years later. During that time, 5,654 cases have been reported to the CDC, which only tracks U.S. data.
What’s more notable than the number of cases is their rate of increase. In 2016, new cases increased by 175 percent and, on average, they have approximately doubled every year. From 2016 through 2022, the number of infections jumped from 63 to 2,377, a roughly 37-fold increase.
“This reminds me of what we saw with epidemics from 2013 through 2020… with Ebola, Zika and the COVID-19 pandemic,” says Robin Robinson, CEO of Spriovas and founding director of the Biomedical Advanced Research and Development Authority (BARDA), which is part of the U.S. Department of Health and Human Services. These epidemics started with a hockey stick trajectory, Robinson says—a gradual growth leading to a sharp spike, just like the shape of a hockey stick.
Another challenge is that right now medics don’t have rapid diagnostic tests for fungal infections. Currently, patients are often misdiagnosed because C. auris resembles several other easily treated fungi. Or they are diagnosed long after the infection begins and is harder to treat.
The problem is that existing diagnostics tests can only identify C. auris once it reaches the bloodstream. Yet, because this pathogen infects bodily tissues first, it should be possible to catch it much earlier before it becomes life-threatening. “We have to diagnose it before it reaches the bloodstream,” Walsh says.
The most alarming fact is that some Candida infections no longer respond to standard therapeutics.
“We need to focus on rapid diagnostic tests that do not rely on a positive blood culture,” says John Sperzel, president and CEO of T2 Biosystems, a company specializing in diagnostics solutions. Blood cultures typically take two to three days for the concentration of Candida to become large enough to detect. The company’s novel test detects about 90 percent of Candida species within three to five hours—thanks to its ability to spot minute quantities of the pathogen in blood samples instead of waiting for them to incubate and proliferate.
Unlike other Candida species C. auris thrives at human body temperatures
Adobe Stock
Tackling the resistance challenge
The most alarming fact is that some Candida infections no longer respond to standard therapeutics. The number of cases that stopped responding to echinocandin, the first-line therapy for most Candida infections, tripled in 2020, according to a study by the CDC.
Now, each of the first four clades shows varying levels of resistance to all three commonly prescribed classes of antifungal medications, such as azoles, echinocandins, and polyenes. For example, 97 percent of infections from C. auris Clade I are resistant to fluconazole, 54 percent to voriconazole and 30 percent of amphotericin. Nearly half are resistant to multiple antifungal drugs. Even with Clade II fungi, which has the least resistance of all the clades, 11 to 14 percent have become resistant to fluconazole.
Anti-fungal therapies typically target specific chemical compounds present on fungi’s cell membranes, but not on human cells—otherwise the medicine would cause damage to our own tissues. Fluconazole and other azole antifungals target a compound called ergosterol, preventing the fungal cells from replicating. Over the years, however, C. auris evolved to resist it, so existing fungal medications don’t work as well anymore.
A newer class of drugs called echinocandins targets a different part of the fungal cell. “The echinocandins – like caspofungin – inhibit (a part of the fungi) involved in making glucan, which is an essential component of the fungal cell wall and is not found in human cells,” Fernandes says. New antifungal treatments are needed, she adds, but there are only a few magic bullets that will hit just the fungus and not the human cells.
Research to fight infections also has been challenged by a lack of government support. That is changing now that BARDA is requesting proposals to develop novel antifungals. “The scope includes C. auris, as well as antifungals following a radiological/nuclear emergency, says BARDA spokesperson Elleen Kane.
The remaining challenge is the number of patients available to participate in clinical trials. Large numbers are needed, but the available patients are quite sick and often die before trials can be completed. Consequently, few biopharmaceutical companies are developing new treatments for C. auris.
ClinicalTrials.gov reports only two drugs in development for invasive C. auris infections—those than can spread throughout the body rather than localize in one particular area, like throat or vaginal infections: ibrexafungerp by Scynexis, Inc., fosmanogepix, by Pfizer.
Scynexis’ ibrexafungerp appears active against C. auris and other emerging, drug-resistant pathogens. The FDA recently approved it as a therapy for vaginal yeast infections and it is undergoing Phase III clinical trials against invasive candidiasis in an attempt to keep the infection from spreading.
“Ibreafungerp is structurally different from other echinocandins,” Fernandes says, because it targets a different part of the fungus. “We’re lucky it has activity against C. auris.”
Pfizer’s fosmanogepix is in Phase II clinical trials for patients with invasive fungal infections caused by multiple Candida species. Results are showing significantly better survival rates for people taking fosmanogepix.
Although C. auris does pose a serious threat to healthcare worldwide, scientists try to stay optimistic—because they recognized the problem early enough, they might have solutions in place before the perfect storm hits. “There is a bit of hope,” says Robinson. “BARDA has finally been able to fund the development of new antifungal agents and, hopefully, this year we can get several new classes of antifungals into development.”
New elevators could lift up our access to space
A space elevator would be cheaper and cleaner than using rockets
Story by Big Think
When people first started exploring space in the 1960s, it cost upwards of $80,000 (adjusted for inflation) to put a single pound of payload into low-Earth orbit.
A major reason for this high cost was the need to build a new, expensive rocket for every launch. That really started to change when SpaceX began making cheap, reusable rockets, and today, the company is ferrying customer payloads to LEO at a price of just $1,300 per pound.
This is making space accessible to scientists, startups, and tourists who never could have afforded it previously, but the cheapest way to reach orbit might not be a rocket at all — it could be an elevator.
The space elevator
The seeds for a space elevator were first planted by Russian scientist Konstantin Tsiolkovsky in 1895, who, after visiting the 1,000-foot (305 m) Eiffel Tower, published a paper theorizing about the construction of a structure 22,000 miles (35,400 km) high.
This would provide access to geostationary orbit, an altitude where objects appear to remain fixed above Earth’s surface, but Tsiolkovsky conceded that no material could support the weight of such a tower.
We could then send electrically powered “climber” vehicles up and down the tether to deliver payloads to any Earth orbit.
In 1959, soon after Sputnik, Russian engineer Yuri N. Artsutanov proposed a way around this issue: instead of building a space elevator from the ground up, start at the top. More specifically, he suggested placing a satellite in geostationary orbit and dropping a tether from it down to Earth’s equator. As the tether descended, the satellite would ascend. Once attached to Earth’s surface, the tether would be kept taut, thanks to a combination of gravitational and centrifugal forces.
We could then send electrically powered “climber” vehicles up and down the tether to deliver payloads to any Earth orbit. According to physicist Bradley Edwards, who researched the concept for NASA about 20 years ago, it’d cost $10 billion and take 15 years to build a space elevator, but once operational, the cost of sending a payload to any Earth orbit could be as low as $100 per pound.
“Once you reduce the cost to almost a Fed-Ex kind of level, it opens the doors to lots of people, lots of countries, and lots of companies to get involved in space,” Edwards told Space.com in 2005.
In addition to the economic advantages, a space elevator would also be cleaner than using rockets — there’d be no burning of fuel, no harmful greenhouse emissions — and the new transport system wouldn’t contribute to the problem of space junk to the same degree that expendable rockets do.
So, why don’t we have one yet?
Tether troubles
Edwards wrote in his report for NASA that all of the technology needed to build a space elevator already existed except the material needed to build the tether, which needs to be light but also strong enough to withstand all the huge forces acting upon it.
The good news, according to the report, was that the perfect material — ultra-strong, ultra-tiny “nanotubes” of carbon — would be available in just two years.
“[S]teel is not strong enough, neither is Kevlar, carbon fiber, spider silk, or any other material other than carbon nanotubes,” wrote Edwards. “Fortunately for us, carbon nanotube research is extremely hot right now, and it is progressing quickly to commercial production.”Unfortunately, he misjudged how hard it would be to synthesize carbon nanotubes — to date, no one has been able to grow one longer than 21 inches (53 cm).
Further research into the material revealed that it tends to fray under extreme stress, too, meaning even if we could manufacture carbon nanotubes at the lengths needed, they’d be at risk of snapping, not only destroying the space elevator, but threatening lives on Earth.
Looking ahead
Carbon nanotubes might have been the early frontrunner as the tether material for space elevators, but there are other options, including graphene, an essentially two-dimensional form of carbon that is already easier to scale up than nanotubes (though still not easy).
Contrary to Edwards’ report, Johns Hopkins University researchers Sean Sun and Dan Popescu say Kevlar fibers could work — we would just need to constantly repair the tether, the same way the human body constantly repairs its tendons.
“Using sensors and artificially intelligent software, it would be possible to model the whole tether mathematically so as to predict when, where, and how the fibers would break,” the researchers wrote in Aeon in 2018.
“When they did, speedy robotic climbers patrolling up and down the tether would replace them, adjusting the rate of maintenance and repair as needed — mimicking the sensitivity of biological processes,” they continued.Astronomers from the University of Cambridge and Columbia University also think Kevlar could work for a space elevator — if we built it from the moon, rather than Earth.
They call their concept the Spaceline, and the idea is that a tether attached to the moon’s surface could extend toward Earth’s geostationary orbit, held taut by the pull of our planet’s gravity. We could then use rockets to deliver payloads — and potentially people — to solar-powered climber robots positioned at the end of this 200,000+ mile long tether. The bots could then travel up the line to the moon’s surface.
This wouldn’t eliminate the need for rockets to get into Earth’s orbit, but it would be a cheaper way to get to the moon. The forces acting on a lunar space elevator wouldn’t be as strong as one extending from Earth’s surface, either, according to the researchers, opening up more options for tether materials.
“[T]he necessary strength of the material is much lower than an Earth-based elevator — and thus it could be built from fibers that are already mass-produced … and relatively affordable,” they wrote in a paper shared on the preprint server arXiv.
After riding up the Earth-based space elevator, a capsule would fly to a space station attached to the tether of the moon-based one.
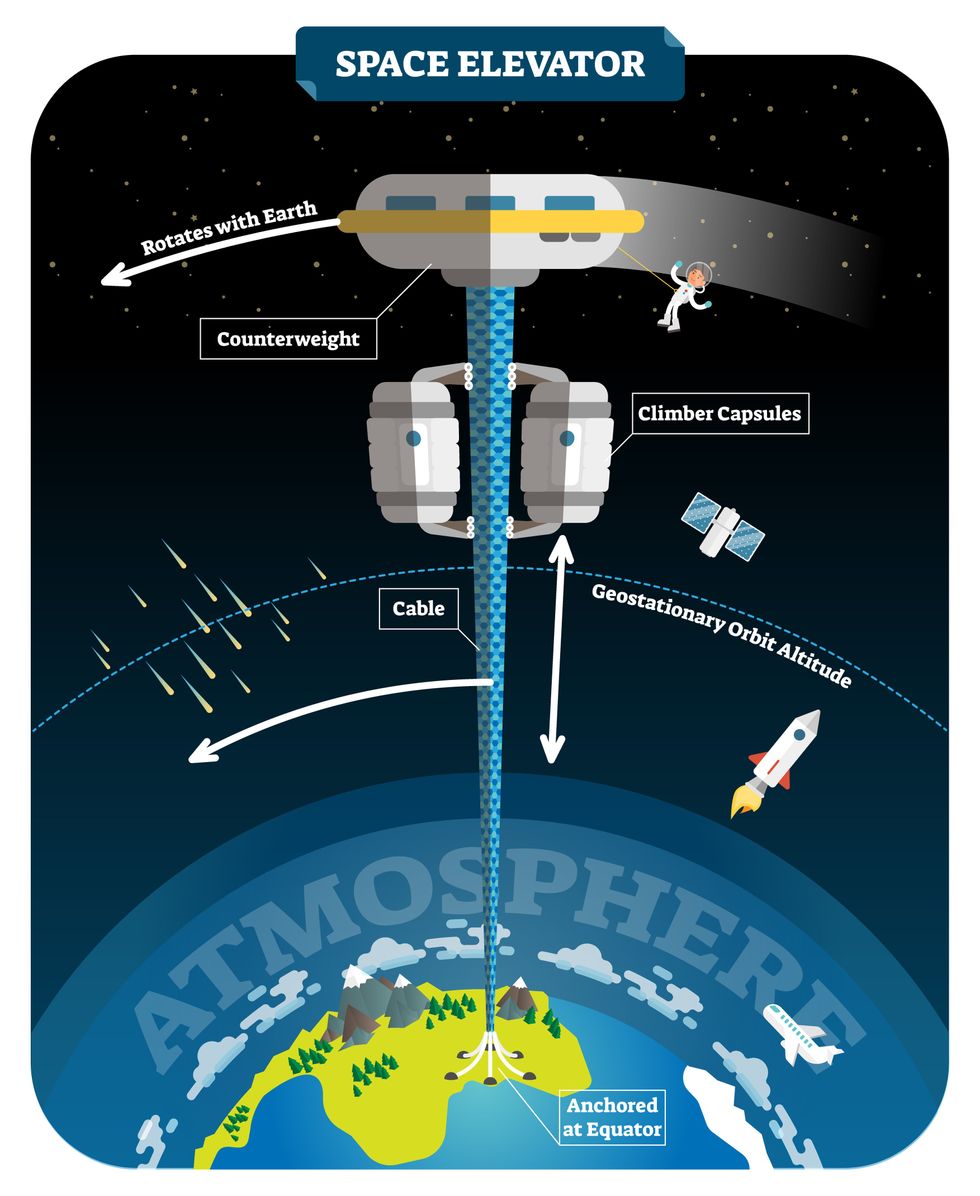
Electrically powered climber capsules could go up down the tether to deliver payloads to any Earth orbit.
Adobe Stock
Some Chinese researchers, meanwhile, aren’t giving up on the idea of using carbon nanotubes for a space elevator — in 2018, a team from Tsinghua University revealed that they’d developed nanotubes that they say are strong enough for a tether.
The researchers are still working on the issue of scaling up production, but in 2021, state-owned news outlet Xinhua released a video depicting an in-development concept, called “Sky Ladder,” that would consist of space elevators above Earth and the moon.
After riding up the Earth-based space elevator, a capsule would fly to a space station attached to the tether of the moon-based one. If the project could be pulled off — a huge if — China predicts Sky Ladder could cut the cost of sending people and goods to the moon by 96 percent.
The bottom line
In the 120 years since Tsiolkovsky looked at the Eiffel Tower and thought way bigger, tremendous progress has been made developing materials with the properties needed for a space elevator. At this point, it seems likely we could one day have a material that can be manufactured at the scale needed for a tether — but by the time that happens, the need for a space elevator may have evaporated.
Several aerospace companies are making progress with their own reusable rockets, and as those join the market with SpaceX, competition could cause launch prices to fall further.
California startup SpinLaunch, meanwhile, is developing a massive centrifuge to fling payloads into space, where much smaller rockets can propel them into orbit. If the company succeeds (another one of those big ifs), it says the system would slash the amount of fuel needed to reach orbit by 70 percent.
Even if SpinLaunch doesn’t get off the ground, several groups are developing environmentally friendly rocket fuels that produce far fewer (or no) harmful emissions. More work is needed to efficiently scale up their production, but overcoming that hurdle will likely be far easier than building a 22,000-mile (35,400-km) elevator to space.
This article originally appeared on Big Think, home of the brightest minds and biggest ideas of all time.