Her Incredible Sense of Smell Helped Scientists Develop the First Parkinson's Test

Joy Milne's unusual sense of smell led Dr. Tilo Kunath, a neurobiologist at the Centre for Regenerative Medicine at the University of Edinburgh, and a host of other scientists, to develop a new diagnostic test for Parkinson's.
Forty years ago, Joy Milne, a nurse from Perth, Scotland, noticed a musky odor coming from her husband, Les. At first, Milne thought the smell was a result of bad hygiene and badgered her husband to take longer showers. But when the smell persisted, Milne learned to live with it, not wanting to hurt her husband's feelings.
Twelve years after she first noticed the "woodsy" smell, Les was diagnosed at the age of 44 with Parkinson's Disease, a neurodegenerative condition characterized by lack of dopamine production and loss of movement. Parkinson's Disease currently affects more than 10 million people worldwide.
Milne spent the next several years believing the strange smell was exclusive to her husband. But to her surprise, at a local support group meeting in 2012, she caught the familiar scent once again, hanging over the group like a cloud. Stunned, Milne started to wonder if the smell was the result of Parkinson's Disease itself.
Milne's discovery led her to Dr. Tilo Kunath, a neurobiologist at the Centre for Regenerative Medicine at the University of Edinburgh. Together, Milne, Kunath, and a host of other scientists would use Milne's unusual sense of smell to develop a new diagnostic test, now in development and poised to revolutionize the treatment of Parkinson's Disease.
"Joy was in the audience during a talk I was giving on my work, which has to do with Parkinson's and stem cell biology," Kunath says. "During the patient engagement portion of the talk, she asked me if Parkinson's had a smell to it." Confused, Kunath said he had never heard of this – but for months after his talk he continued to turn the question over in his mind.
Kunath knew from his research that the skin's microbiome changes during different disease processes, releasing metabolites that can give off odors. In the medical literature, diseases like melanoma and Type 2 diabetes have been known to carry a specific scent – but no such connection had been made with Parkinson's. If people could smell Parkinson's, he thought, then it stood to reason that those metabolites could be isolated, identified, and used to potentially diagnose Parkinson's by their presence alone.
First, Kunath and his colleagues decided to test Milne's sense of smell. "I got in touch with Joy again and we designed a protocol to test her sense of smell without her having to be around patients," says Kunath, which could have affected the validity of the test. In his spare time, Kunath collected t-shirt samples from people diagnosed with Parkinson's and from others without the diagnosis and gave them to Milne to smell. In 100 percent of the samples, Milne was able to detect whether a person had Parkinson's based on smell alone. Amazingly, Milne was even able to detect the "Parkinson's scent" in a shirt from the control group – someone who did not have a Parkinson's diagnosis, but would go on to be diagnosed nine months later.
From the initial study, the team discovered that Parkinson's did have a smell, that Milne – inexplicably – could detect it, and that she could detect it long before diagnosis like she had with her husband, Les. But the experiments revealed other things that the team hadn't been expecting.
"One surprising thing we learned from that experiment was that the odor was always located in the back of the shirt – never in the armpit, where we expected the smell to be," Kunath says. "I had a chance meeting with a dermatologist and he said the smell was due to the patient's sebum, which are greasy secretions that are really dense on your upper back. We have sweat glands, instead of sebum, in our armpits." Patients with Parkinson's are also known to have increased sebum production.
With the knowledge that a patient's sebum was the source of the unusual smell, researchers could go on to investigate exactly what metabolites were in the sebum and in what amounts. Kunath, along with his associate, Dr. Perdita Barran, collected and analyzed sebum samples from 64 participants across the United Kingdom. Once the samples were collected, Barran and others analyzed it using a method called gas chromatography mass spectrometry, or GS-MC, which separated, weighed and helped identify the individual compounds present in each sebum sample.
Barran's team can now correctly identify Parkinson's in nine out of 10 patients – a much quicker and more accurate way to diagnose than what clinicians do now.
"The compounds we've identified in the sebum are not unique to people with Parkinson's, but they are differently expressed," says Barran, a professor of mass spectrometry at the University of Manchester. "So this test we're developing now is not a black-and-white, do-you-have-something kind of test, but rather how much of these compounds do you have compared to other people and other compounds." The team identified over a dozen compounds that were present in the sebum of Parkinson's patients in much larger amounts than the control group.
Using only the GC-MS and a sebum swab test, Barran's team can now correctly identify Parkinson's in nine out of 10 patients – a much quicker and more accurate way to diagnose than what clinicians do now.
"At the moment, a clinical diagnosis is based on the patient's physical symptoms," Barran says, and determining whether a patient has Parkinson's is often a long and drawn-out process of elimination. "Doctors might say that a group of symptoms looks like Parkinson's, but there are other reasons people might have those symptoms, and it might take another year before they're certain," Barran says. "Some of those symptoms are just signs of aging, and other symptoms like tremor are present in recovering alcoholics or people with other kinds of dementia." People under the age of 40 with Parkinson's symptoms, who present with stiff arms, are often misdiagnosed with carpal tunnel syndrome, she adds.
Additionally, by the time physical symptoms are present, Parkinson's patients have already lost a substantial amount of dopamine receptors – about sixty percent -- in the brain's basal ganglia. Getting a diagnosis before physical symptoms appear would mean earlier interventions that could prevent dopamine loss and preserve regular movement, Barran says.
"Early diagnosis is good if it means there's a chance of early intervention," says Barran. "It stops the process of dopamine loss, which means that motor symptoms potentially will not happen, or the onset of symptoms will be substantially delayed." Barran's team is in the processing of streamlining the sebum test so that definitive results will be ready in just two minutes.
"What we're doing right now will be a very inexpensive test, a rapid-screen test, and that will encourage people to self-sample and test at home," says Barran. In addition to diagnosing Parkinson's, she says, this test could also be potentially useful to determine if medications were at a therapeutic dose in people who have the disease, since the odor is strongest in people whose symptoms are least controlled by medication.
"When symptoms are under control, the odor is lower," Barran says. "Potentially this would allow patients and clinicians to see whether their symptoms are being managed properly with medication, or perhaps if they're being overmedicated." Hypothetically, patients could also use the test to determine if interventions like diet and exercise are effective at keeping Parkinson's controlled.
"We hope within the next two to five years we will have a test available."
Barran is now running another clinical trial – one that determines whether they can diagnose at an earlier stage and whether they can identify a difference in sebum samples between different forms of Parkinson's or diseases that have Parkinson's-like symptoms, such as Lewy Body Dementia.
"Within the next one to two years, we hope to be running a trial in the Manchester area for those people who do not have motor symptoms but are at risk for developing dementia due to symptoms like loss of smell and sleep difficulty," Barran had said in 2019. "If we can establish that, we can roll out a test that determines if you have Parkinson's or not with those first pre-motor symptoms, and then at what stage. We hope within the next two to five years we will have a test available."
In a 2022 study, published in the American Chemical Society, researchers used mass spectrometry to analyze sebum from skin swabs for the presence of the specific molecules. They found that some specific molecules are present only in people who have Parkinson’s. Now they hope that the same method can be used in regular diagnostic labs. The test, many years in the making, is inching its way to the clinic.
"We would likely first give this test to people who are at risk due to a genetic predisposition, or who are at risk based on prodomal symptoms, like people who suffer from a REM sleep disorder who have a 50 to 70 percent chance of developing Parkinson's within a ten year period," Barran says. "Those would be people who would benefit from early therapeutic intervention. For the normal population, it isn't beneficial at the moment to know until we have therapeutic interventions that can be useful."
Milne's husband, Les, passed away from complications of Parkinson's Disease in 2015. But thanks to him and the dedication of his wife, Joy, science may have found a way to someday prolong the lives of others with this devastating disease. Sometimes she can smell people who have Parkinson’s while in the supermarket or walking down the street but has been told by medical ethicists she cannot tell them, Milne said in an interview with the Guardian. But once the test becomes available in the clinics, it will do the job for her.
[Ed. Note: A older version of this hit article originally ran on September 3, 2019.]
Coronavirus Risk Calculators: What You Need to Know
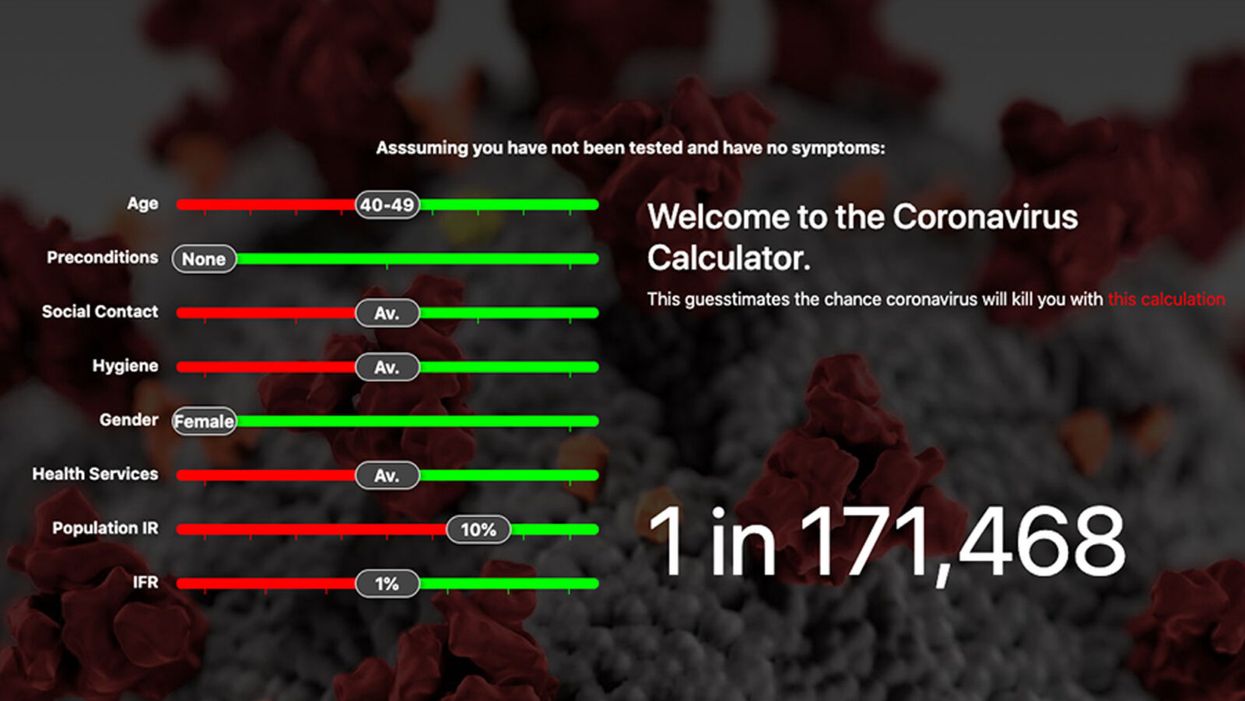
A screenshot of one coronavirus risk calculator.
People in my family seem to develop every ailment in the world, including feline distemper and Dutch elm disease, so I naturally put fingers to keyboard when I discovered that COVID-19 risk calculators now exist.
"It's best to look at your risk band. This will give you a more useful insight into your personal risk."
But the results – based on my answers to questions -- are bewildering.
A British risk calculator developed by the Nexoid software company declared I have a 5 percent, or 1 in 20, chance of developing COVID-19 and less than 1 percent risk of dying if I get it. Um, great, I think? Meanwhile, 19 and Me, a risk calculator created by data scientists, says my risk of infection is 0.01 percent per week, or 1 in 10,000, and it gave me a risk score of 44 out of 100.
Confused? Join the club. But it's actually possible to interpret numbers like these and put them to use. Here are five tips about using coronavirus risk calculators:
1. Make Sure the Calculator Is Designed For You
Not every COVID-19 risk calculator is designed to be used by the general public. Cleveland Clinic's risk calculator, for example, is only a tool for medical professionals, not sick people or the "worried well," said Dr. Lara Jehi, Cleveland Clinic's chief research information officer.
Unfortunately, the risk calculator's web page fails to explicitly identify its target audience. But there are hints that it's not for lay people such as its references to "platelets" and "chlorides."
The 19 and Me or the Nexoid risk calculators, in contrast, are both designed for use by everyone, as is a risk calculator developed by Emory University.
2. Take a Look at the Calculator's Privacy Policy
COVID-19 risk calculators ask for a lot of personal information. The Nexoid calculator, for example, wanted to know my age, weight, drug and alcohol history, pre-existing conditions, blood type and more. It even asked me about the prescription drugs I take.
It's wise to check the privacy policy and be cautious about providing an email address or other personal information. Nexoid's policy says it provides the information it gathers to researchers but it doesn't release IP addresses, which can reveal your location in certain circumstances.
John-Arne Skolbekken, a professor and risk specialist at Norwegian University of Science and Technology, entered his own data in the Nexoid calculator after being contacted by LeapsMag for comment. He noted that the calculator, among other things, asks for information about use of recreational drugs that could be illegal in some places. "I have given away some of my personal data to a company that I can hope will not misuse them," he said. "Let's hope they are trustworthy."
The 19 and Me calculator, by contrast, doesn't gather any data from users, said Cindy Hu, data scientist at Mathematica, which created it. "As soon as the window is closed, that data is gone and not captured."
The Emory University risk calculator, meanwhile, has a long privacy policy that states "the information we collect during your assessment will not be correlated with contact information if you provide it." However, it says personal information can be shared with third parties.
3. Keep an Eye on Time Horizons
Let's say a risk calculator says you have a 1 percent risk of infection. That's fairly low if we're talking about this year as a whole, but it's quite worrisome if the risk percentage refers to today and jumps by 1 percent each day going forward. That's why it's helpful to know exactly what the numbers mean in terms of time.
Unfortunately, this information isn't always readily available. You may have to dig around for it or contact a risk calculator's developers for more information. The 19 and Me calculator's risk percentages refer to this current week based on your behavior this week, Hu said. The Nexoid calculator, by contrast, has an "infinite timeline" that assumes no vaccine is developed, said Jonathon Grantham, the company's managing director. But your results will vary over time since the calculator's developers adjust it to reflect new data.
When you use a risk calculator, focus on this question: "How does your risk compare to the risk of an 'average' person?"
4. Focus on the Big Picture
The Nexoid calculator gave me numbers of 5 percent (getting COVID-19) and 99.309 percent (surviving it). It even provided betting odds for gambling types: The odds are in favor of me not getting infected (19-to-1) and not dying if I get infected (144-to-1).
However, Grantham told me that these numbers "are not the whole story." Instead, he said, "it's best to look at your risk band. This will give you a more useful insight into your personal risk." Risk bands refer to a segmentation of people into five categories, from lowest to highest risk, according to how a person's result sits relative to the whole dataset.
The Nexoid calculator says I'm in the "lowest risk band" for getting COVID-19, and a "high risk band" for dying of it if I get it. That suggests I'd better stay in the lowest-risk category because my pre-existing risk factors could spell trouble for my survival if I get infected.
Michael J. Pencina, a professor and biostatistician at Duke University School of Medicine, agreed that focusing on your general risk level is better than focusing on numbers. When you use a risk calculator, he said, focus on this question: "How does your risk compare to the risk of an 'average' person?"
The 19 and Me calculator, meanwhile, put my risk at 44 out of 100. Hu said that a score of 50 represents the typical person's risk of developing serious consequences from another disease – the flu.
5. Remember to Take Action
Hu, who helped develop the 19 and Me risk calculator, said it's best to use it to "understand the relative impact of different behaviors." As she noted, the calculator is designed to allow users to plug in different answers about their behavior and immediately see how their risk levels change.
This information can help us figure out if we should change the way we approach the world by, say, washing our hands more or avoiding more personal encounters.
"Estimation of risk is only one part of prevention," Pencina said. "The other is risk factors and our ability to reduce them." In other words, odds, percentages and risk bands can be revealing, but it's what we do to change them that matters.
Pseudoscience Is Rampant: How Not to Fall for It
A metaphorical rendering of scientific truth gone awry.
Whom to believe?
The relentless and often unpredictable coronavirus (SARS-CoV-2) has, among its many quirky terrors, dredged up once again the issue that will not die: science versus pseudoscience.
How does one learn to spot the con without getting a Ph.D. and spending years in a laboratory?
The scientists, experts who would be the first to admit they are not infallible, are now in danger of being drowned out by the growing chorus of pseudoscientists, conspiracy theorists, and just plain troublemakers that seem to be as symptomatic of the virus as fever and weakness.
How is the average citizen to filter this cacophony of information and misinformation posing as science alongside real science? While all that noise makes it difficult to separate the real stuff from the fakes, there is at least one positive aspect to it all.
A famous aphorism by one Charles Caleb Colton, a popular 19th-century English cleric and writer, says that "imitation is the sincerest form of flattery."
The frauds and the paranoid conspiracy mongers who would perpetrate false science on a susceptible public are at least recognizing the value of science—they imitate it. They imitate the ways in which science works and make claims as if they were scientists, because even they recognize the power of a scientific approach. They are inadvertently showing us how much we value science. Unfortunately they are just shabby counterfeits.
Separating real science from pseudoscience is not a new problem. Philosophers, politicians, scientists, and others have been worrying about this perhaps since science as we know it, a science based entirely on experiment and not opinion, arrived in the 1600s. The original charter of the British Royal Society, the first organized scientific society, stated that at their formal meetings there would be no discussion of politics, religion, or perpetual motion machines.
The first two of those for the obvious purpose of keeping the peace. But the third is interesting because at that time perpetual motion machines were one of the main offerings of the imitators, the bogus scientists who were sure that you could find ways around the universal laws of energy and make a buck on it. The motto adopted by the society was, and remains, Nullius in verba, Latin for "take nobody's word for it." Kind of an early version of Missouri's venerable state motto: "Show me."
You might think that telling phony science from the real thing wouldn't be so difficult, but events, historical and current, tell a very different story—often with tragic outcomes. Just one terrible example is the estimated 350,000 additional HIV deaths in South Africa directly caused by the now-infamous conspiracy theories of their own elected President no less (sound familiar?). It's surprisingly easy to dress up phony science as the real thing by simply adopting, or appearing to adopt, the trappings of science.
Thus, the anti-vaccine movement claims to be based on suspicion of authority, beginning with medical authority in this case, stemming from the fraudulent data published by the now-disgraced Andrew Wakefield, an English gastroenterologist. And it's true that much of science is based on suspicion of authority. Science got its start when the likes of Galileo and Copernicus claimed that the Church, the State, even Aristotle, could no longer be trusted as authoritative sources of knowledge.
But Galileo and those who followed him produced alternative explanations, and those alternatives were based on data that arose independently from many sources and generated a great deal of debate and, most importantly, could be tested by experiments that could prove them wrong. The anti-vaccine movement imitates science, still citing the discredited Wakefield report, but really offers nothing but suspicion—and that is paranoia, not science.
Similarly, there are those who try to cloak their nefarious motives in the trappings of science by claiming that they are taking the scientific posture of doubt. Science after all depends on doubt—every scientist doubts every finding they make. Every scientist knows that they can't possibly foresee all possible instances or situations in which they could be proven wrong, no matter how strong their data. Einstein was doubted for two decades, and cosmologists are still searching for experimental proofs of relativity. Science indeed progresses by doubt. In science revision is a victory.
But the imitators merely use doubt to suggest that science is not dependable and should not be used for informing policy or altering our behavior. They claim to be taking the legitimate scientific stance of doubt. Of course, they don't doubt everything, only what is problematic for their individual enterprises. They don't doubt the value of blood pressure medicine to control their hypertension. But they should, because every medicine has side effects and we don't completely understand how blood pressure is regulated and whether there may not be still better ways of controlling it.
But we use the pills we have because the science is sound even when it is not completely settled. Ask a hypertensive oil executive who would like you to believe that climate science should be ignored because there are too many uncertainties in the data, if he is willing to forgo his blood pressure medicine—because it, too, has its share of uncertainties and unwanted side effects.
The apparent success of pseudoscience is not due to gullibility on the part of the public. The problem is that science is recognized as valuable and that the imitators are unfortunately good at what they do. They take a scientific pose to gain your confidence and then distort the facts to their own purposes. How does one learn to spot the con without getting a Ph.D. and spending years in a laboratory?
"If someone claims to have the ultimate answer or that they know something for certain, the only thing for sure is that they are trying to fool you."
What can be done to make the distinction clearer? Several solutions have been tried—and seem to have failed. Radio and television shows about the latest scientific breakthroughs are a noble attempt to give the public a taste of good science, but they do nothing to help you distinguish between them and the pseudoscience being purveyed on the neighboring channel and its "scientific investigations" of haunted houses.
Similarly, attempts to inculcate what are called "scientific habits of mind" are of little practical help. These habits of mind are not so easy to adopt. They invariably require some amount of statistics and probability and much of that is counterintuitive—one of the great values of science is to help us to counter our normal biases and expectations by showing that the actual measurements may not bear them out.
Additionally, there is math—no matter how much you try to hide it, much of the language of science is math (Galileo said that). And half the audience is gone with each equation (Stephen Hawking said that). It's hard to imagine a successful program of making a non-scientifically trained public interested in adopting the rigors of scientific habits of mind. Indeed, I suspect there are some people, artists for example, who would be rightfully suspicious of changing their thinking to being habitually scientific. Many scientists are frustrated by the public's inability to think like a scientist, but in fact it is neither easy nor always desirable to do so. And it is certainly not practical.
There is a more intuitive and simpler way to tell the difference between the real thing and the cheap knock-off. In fact, it is not so much intuitive as it is counterintuitive, so it takes a little bit of mental work. But the good thing is it works almost all the time by following a simple, if as I say, counterintuitive, rule.
True science, you see, is mostly concerned with the unknown and the uncertain. If someone claims to have the ultimate answer or that they know something for certain, the only thing for sure is that they are trying to fool you. Mystery and uncertainty may not strike you right off as desirable or strong traits, but that is precisely where one finds the creative solutions that science has historically arrived at. Yes, science accumulates factual knowledge, but it is at its best when it generates new and better questions. Uncertainty is not a place of worry, but of opportunity. Progress lives at the border of the unknown.
How much would it take to alter the public perception of science to appreciate unknowns and uncertainties along with facts and conclusions? Less than you might think. In fact, we make decisions based on uncertainty every day—what to wear in case of 60 percent chance of rain—so it should not be so difficult to extend that to science, in spite of what you were taught in school about all the hard facts in those giant textbooks.
You can believe science that says there is clear evidence that takes us this far… and then we have to speculate a bit and it could go one of two or three ways—or maybe even some way we don't see yet. But like your blood pressure medicine, the stuff we know is reliable even if incomplete. It will lower your blood pressure, no matter that better treatments with fewer side effects may await us in the future.
Unsettled science is not unsound science. The honesty and humility of someone who is willing to tell you that they don't have all the answers, but they do have some thoughtful questions to pursue, are easy to distinguish from the charlatans who have ready answers or claim that nothing should be done until we are an impossible 100-percent sure.
Imitation may be the sincerest form of flattery.
The problem, as we all know, is that flattery will get you nowhere.
[Editor's Note: This article was originally published on June 8th, 2020 as part of a standalone magazine called GOOD10: The Pandemic Issue. Produced as a partnership among LeapsMag, The Aspen Institute, and GOOD, the magazine is available for free online.]