New tech for prison reform spreads to 11 states
The U.S. has the highest incarceration rate in the world, costing $182 billion per year, partly because its antiquated data systems often fail to identify people who should be released. A tech nonprofit is trying to change that.
A new non-profit called Recidiviz is using data technology to reduce the size of the U.S. criminal justice system. The bi-coastal company (SF and NYC) is currently working with 11 states to improve their systems and, so far, has helped remove nearly 69,000 people — ones left floundering in jail or on parole when they should have been released.
“The root cause is fragmentation,” says Clementine Jacoby, 31, a software engineer who worked at Google before co-founding Recidiviz in 2019. In the 1970s and 80s, the U.S. built a series of disconnected data systems, and this patchwork is still being used by criminal justice authorities today. It requires parole officers to manually calculate release dates, leading to errors in many cases. “[They] have done everything they need to do to earn their release, but they're still stuck in the system,” Jacoby says.
Recidiviz has built a platform that connects the different databases, with the goal of identifying people who are already qualified for release but remain behind bars or on supervision. “Think of Recidiviz like Google Maps,” says Jacoby, who worked on Maps when she was at the tech giant. Google Maps takes in data from different sources – satellite images, street maps, local business data — and organizes it into one easy view. “Recidiviz does something similar with criminal justice data,” Jacoby explains, “making it easy to identify people eligible to come home or to move to less intensive levels of supervision.”
People like Jacoby’s uncle. His experience with incarceration is what inspired her passion for criminal justice reform in the first place.
The problems are vast
The U.S. has the highest incarceration rate in the world — 2 million people according to the watchdog group, Prison Policy Initiative — at a cost of $182 billion a year. The numbers could be a lot lower if not for an array of problems including inaccurate sentencing calculations, flawed algorithms and parole violations laws.
Sentencing miscalculations
To determine eligibility for release, the current system requires corrections officers to check 21 different requirements spread across five different databases for each of the 90 to 100 people under their supervision. These manual calculations are time prohibitive, says Jacoby, and fall victim to human error.
In addition, Recidiviz found that policies aimed at helping to reduce the prison population don’t always work correctly. A key example is time off for good behavior laws that allow inmates to earn one day off for every 30 days of good behavior. Some states' data systems are built to calculate time off as one day per month of good behavior, rather than per day. Over the course of a decade-long sentence, Jacoby says these miscalculations can lead to a huge discrepancy in the calculated release data and the actual release date.
Algorithms
Commercial algorithm-based software systems for risk assessment continue to be widely used in the criminal justice system, even though a 2018 study published in Science Advances exposed their limitations. After the study went viral, it took three years for the Justice Department to issue a report on their own flawed algorithms used to reduce the federal prison population as part of the 2018 First Step Act. The program, it was determined, overestimated the risk of putting inmates of color into early-release programs.
Despite its name, Recidiviz does not build these types of algorithms for predicting recidivism, or whether someone will commit another crime after being released from prison. Rather, Jacoby says the company’s "descriptive analytics” approach is specifically intended to weed out incarceration inequalities and avoid algorithmic pitfalls.
Parole violation laws
Research shows that 350,000 people a year — about a quarter of the total prison population — are sent back not because they’ve committed another crime, but because they’ve broken a specific rule of their probation. “Things that wouldn't send you or I to prison, but would send someone on parole,” such as crossing county lines or being in the presence of alcohol when they shouldn’t be, are inflating the prison population, says Jacoby.
It’s personal for the co-founder and CEO
“I grew up with an uncle who went into the prison system,” Jacoby says. At 19, he was sentenced to ten years in prison for a non-violent crime. A few months after being released from jail, he was sent back for a non-violent parole violation.
“For my family, the fact that one in four prison admissions are driven not by a crime but by someone who's broken a rule on probation and parole was really profound because that happened to my uncle,” Jacoby says. The experience led her to begin studying criminal justice in high school, then college. She continued her dive into how the criminal justice system works as part of her Passion Project while at Google, a program that allows employees to spend 20 percent of their time on pro-bono work. Two colleagues whose family members had also been stuck in the system joined her.
As part of the project, Jacoby interviewed hundreds of people involved in the criminal justice system. “Those on the right, those on the left, agreed that bad data was slowing down reform,” she says. Their research brought them to North Dakota where they began to understand the root of the problem. The corrections department is making “huge, consequential decisions every day [without] … the data,” Jacoby says. In a new video by Recidiviz not yet released, Jacoby recounts her exchange with the state’s director of corrections who told her, “‘It’s not that we have the data and we just don’t know how to make it public; we don’t have the information you think we have.'"
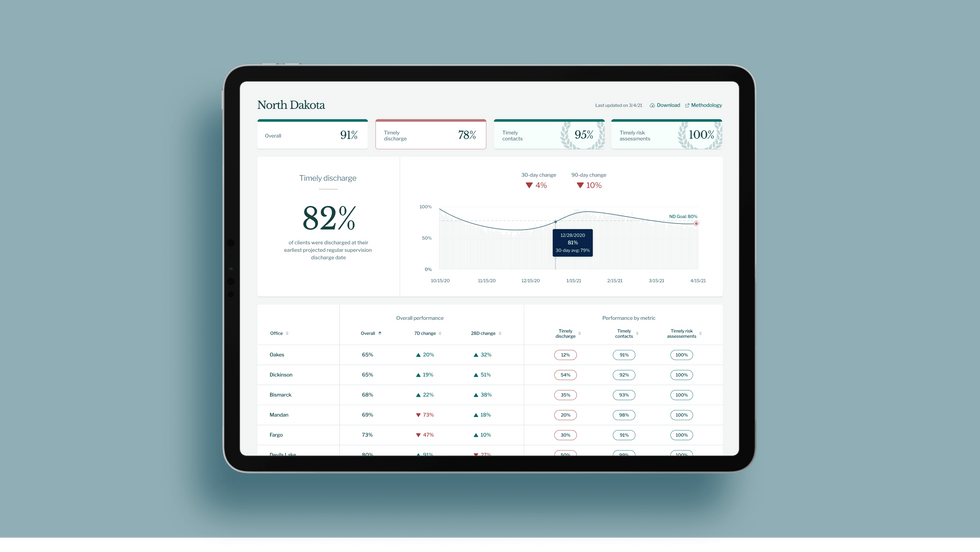
A mock-up (with fake data) of the types of dashboards and insights that Recidiviz provides to state governments.
Recidiviz
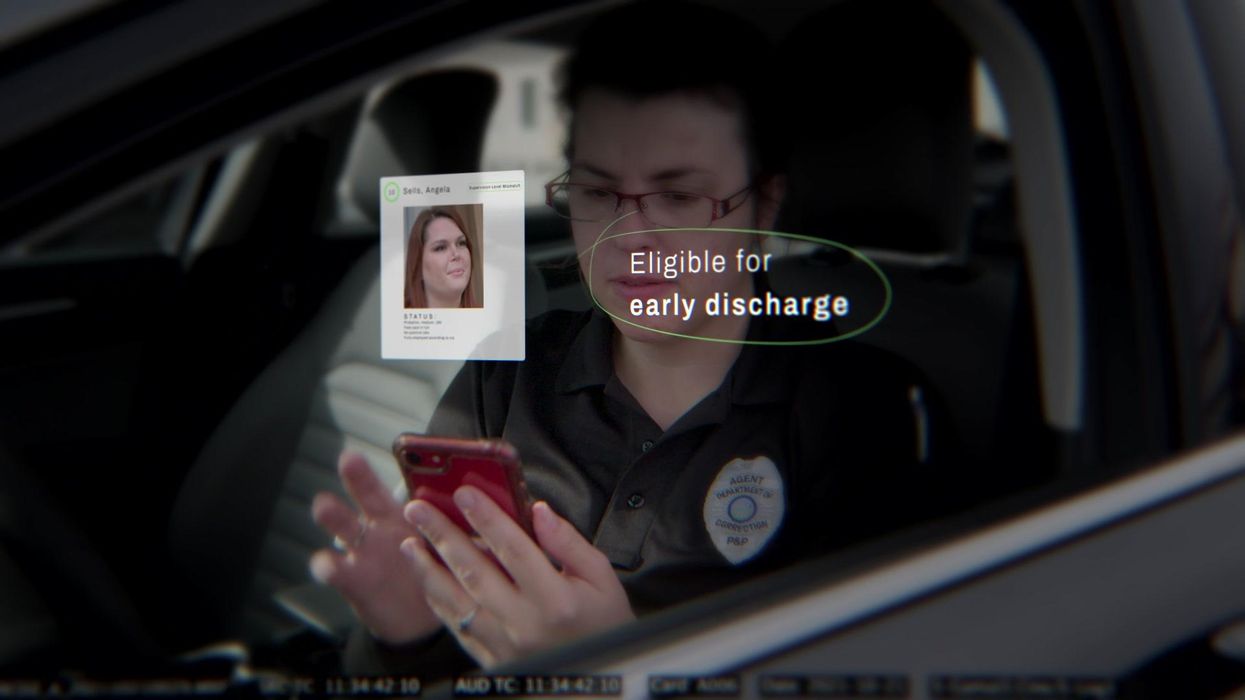
As a software engineer, Jacoby says the comment made no sense to her — until she witnessed it first-hand. “We spent a lot of time driving around in cars with corrections directors and parole officers watching them use these incredibly taxing, frankly terrible, old data systems,” Jacoby says.
As they weeded through thousands of files — some computerized, some on paper — they unearthed the consequences of bad data: Hundreds of people in prison well past their release date and thousands more whose release from parole was delayed because of minor paperwork issues. They found individuals stuck in parole because they hadn’t checked one last item off their eligibility list — like simply failing to provide their parole officer with a paystub. And, even when parolees advocated for themselves, the archaic system made it difficult for their parole officers to confirm their eligibility, so they remained in the system. Jacoby and her team also unpacked specific policies that drive racial disparities — such as fines and fees.
The Solution
It’s more than a trivial technical challenge to bring the incomplete, fragmented data onto a 21st century data platform. It takes months for Recidiviz to sift through a state’s information systems to connect databases “with the goal of tracking a person all the way through their journey and find out what’s working for 18- to 25-year-old men, what’s working for new mothers,” explains Jacoby in the video.
TED Talk: How bad data traps people in the U.S. justice system

TED Fellow Clementine Jacoby's TED Talk went live on Jan. 13. It describes how we can fix bad data in the criminal justice system, "bringing thousands of people home, reducing costs and improving public safety along the way."
Clementine Jacoby • TED2022
Ojmarrh Mitchell, an associate professor in the School of Criminology and Criminal Justice at Arizona State University, who is not involved with the company, says what Recidiviz is doing is “remarkable.” His perspective goes beyond academic analysis. In his pre-academic years, Mitchell was a probation officer, working within the framework of the “well known, but invisible” information sharing issues that plague criminal justice departments. The flexibility of Recidiviz’s approach is what makes it especially innovative, he says. “They identify the specific gaps in each jurisdiction and tailor a solution for that jurisdiction.”
On the downside, the process used by Recidiviz is “a bit opaque,” Mitchell says, with few details available on how Recidiviz designs its tools and tracks outcomes. By sharing more information about how its actions lead to progress in a given jurisdiction, Recidiviz could help reformers in other places figure out which programs have the best potential to work well.
The eleven states in which Recidiviz is working include California, Colorado, Maine, Michigan, Missouri, Pennsylvania and Tennessee. And a pilot program launched last year in Idaho, if scaled nationally, with could reduce the number of people in the criminal justice system by a quarter of a million people, Jacoby says. As part of the pilot, rather than relying on manual calculations, Recidiviz is equipping leaders and the probation officers with actionable information with a few clicks of an app that Recidiviz built.
Mitchell is disappointed that there’s even the need for Recidiviz. “This is a problem that government agencies have a responsibility to address,” he says. “But they haven’t.” For one company to come along and fill such a large gap is “remarkable.”
Questions remain about new drug for hot flashes
In May, a new drug, Fezolinetant, was approved by the FDA to treat hot flashes associated with menopause.
Vascomotor symptoms (VMS) is the medical term for hot flashes associated with menopause. You are going to hear a lot more about it because a company has a new drug to sell. Here is what you need to know.
Menopause marks the end of a woman’s reproductive capacity. Normal hormonal production associated with that monthly cycle becomes erratic and finally ceases. For some women the transition can be relatively brief with only modest symptoms, while for others the body's “thermostat” in the brain is disrupted and they experience hot flashes and other symptoms that can disrupt daily activity. Lifestyle modification and drugs such as hormone therapy can provide some relief, but women at risk for cancer are advised not to use them and other women choose not to do so.
Fezolinetant, sold by Astellas Pharma Inc. under the product name Veozah™, was approved by the Food and Drug Administration (FDA) on May 12 to treat hot flashes associated with menopause. It is the first in a new class of drugs called neurokinin 3 receptor antagonists, which block specific neurons in the brain “thermostat” that trigger VMS. It does not appear to affect other symptoms of menopause. As with many drugs targeting a brain cell receptor, it must be taken continuously for a few days to build up a good therapeutic response, rather than working as a rescue product such as an asthma inhaler to immediately treat that condition.
Hot flashes vary greatly and naturally get better or resolve completely with time. That contributes to a placebo effect and makes it more difficult to judge the outcome of any intervention. Early this year, a meta analysis of 17 studies of drug trials for hot flashes found an unusually large placebo response in those types of studies; the placebo groups had an average of 5.44 fewer hot flashes and a 36 percent reduction in their severity.
In studies of fezolinetant, the drug recently approved by the FDA, the placebo benefit was strong and persistent. The drug group bested the placebo response to a statistically significant degree but, “If people have gone from 11 hot flashes a day to eight or seven in the placebo group and down to a couple fewer ones in the drug groups, how meaningful is that? Having six hot flashes a day is still pretty unpleasant,” says Diana Zuckerman, president of the National Center for Health Research (NCHR), a health oriented think tank.
“Is a reduction compared to placebo of 2-3 hot flashes per day, in a population of women experiencing 10-11 moderate to severe hot flashes daily, enough relief to be clinically meaningful?” Andrea LaCroix asked a commentary published in Nature Medicine. She is an epidemiologist at the University of California San Diego and a leader of the MsFlash network that has conducted a handful of NIH-funded studies on menopause.
Questions Remain
LaCroix and others have raised questions about how Astellas, the company that makes the new drug, handled missing data from patients who dropped out of the clinical trials. “The lack of detailed information about important parameters such as adherence and missing data raises concerns that the reported benefits of fezolinetant very likely overestimate those that will be observed in clinical practice," LaCroix wrote.
In response to this concern, Anna Criddle, director of global portfolio communications at Astellas, wrote in an email to Leaps.org: “…a full analysis of data, including adherence data and any impact of missing data, was submitted for assessment by [the FDA].”
The company ran the studies at more than 300 sites around the world. Curiously, none appear to have been at academic medical centers, which are known for higher quality research. Zuckerman says, "When somebody is paid to do a study, if they want to get paid to do another study by the same company, they will try to make sure that the results are the results that the company wants.”
Criddle said that Astellas picked the sites “that would allow us to reach a diverse population of women, including race and ethnicity.”
A trial of a lower dose of the drug was conducted in Asia. In March 2022, Astellas issued a press release saying it had failed to prove effectiveness. No further data has been released. Astellas still plans to submit the data, according to Criddle. Results from clinical trials funded by the U.S. goverment must be reported on clinicaltrials.gov within one year of the study's completion - a deadline that, in this case, has expired.
The measurement scale for hot flashes used in the studies, mild-moderate-severe, also came in for criticism. “It is really not good scale, there probably isn’t a broad enough range of things going on or descriptors,” says David Rind. He is chief medical officer of the Institute for Clinical and Economic Review (ICER), a nonprofit authority on new drugs. It conducted a thorough review and analysis of fezolinestant using then existing data gathered from conference abstracts, posters and presentations and included a public stakeholder meeting in December. A 252-page report was published in January, finding “considerable uncertainty about the comparative net health benefits of fezolinetant” versus hormone therapy.
Questions surrounding some of these issues might have been answered if the FDA had chosen to hold a public advisory committee meeting on fezolinetant, which it regularly does for first in class medicines. But the agency decided such a meeting was unnecessary.
Cost
There was little surprise when Astellas announced a list price for fezolinetant of $550 a month ($6000 annually) and a program of patient assistance to ease out of pocket expenses. The company had already incurred large expenses.
In 2017 Astellas purchased the company that originally developed fezolinetant for $534 million plus several hundred million in potential royalties. The drug company ran a "disease awareness” ad, Heat on the Street, hat aired during the Super Bowl in February, where 30 second ads cost about $7 million. Industry analysts have projected sales to be $1.9 billion by 2028.
ICER’s pre-approval evaluation said fezolinetant might "be considered cost-effective if priced around $2,000 annually. ... [It]will depend upon its price and whether it is considered an alternative to MHT [menopause hormone treatment] for all women or whether it will primarily be used by women who cannot or will not take MHT."
Criddle wrote that Astellas set the price based on the novelty of the science, the quality of evidence for the drug and its uniqueness compared to the rest of the market. She noted that an individual’s payment will depend on how much their insurance company decides to cover. “[W]e expect insurance coverage to increase over the course of the year and to achieve widespread coverage in the U.S. over time.”
Leaps.org wrote to and followed up with nine of the largest health insurers/providers asking basic questions about their coverage of fezolinetant. Only two responded. Jennifer Martin, the deputy chief consultant for pharmacy benefits management at the Department of Veterans Affairs, said the agency “covers all drugs from the date that they are launched.” Decisions on whether it will be included in the drug formulary and what if any copays might be required are under review.
“[Fezolinetant] will go through our standard P&T Committee [patient and treatment] review process in the next few months, including a review of available efficacy data, safety data, clinical practice guidelines, and comparison with other agents used for vasomotor symptoms of menopause," said Phil Blando, executive director of corporate communications for CVS Health.
Other insurers likely are going through a similar process to decide issues such as limiting coverage to women who are advised not to use hormones, how much copay will be required, and whether women will be required to first try other options or obtain approvals before getting a prescription.
Rind wants to see a few years of use before he prescribes fezolinetant broadly, and believes most doctors share his view. Nor will they be eager to fill out the additional paperwork required for women to participate in the Astellas patient assistance program, he added.
Safety
Astellas is marketing its drug by pointing out risks of hormone therapy, such as a recent paper in The BMJ, which noted that women who took hormones for even a short period of time had a 24 percent increased risk of dementia. While the percentage was scary, the combined number of women both on and off hormones who developed dementia was small. And it is unclear whether hormones are causing dementia or if more severe hot flashes are a marker for higher risk of developing dementia. This information is emerging only after 80 years of hundreds of millions of women using hormones.
In contrast, the label for fezolinetant prohibits “concomitant use with CYP1A2 inhibitors” and requires testing for liver and kidney function prior to initiating the drug and every three months thereafter. There is no human or animal data on use in a geriatric population, defined as 65 or older, a group that is likely to use the drug. Only a few thousand women have ever taken fezolinetant and most have used it for just a few months.
Options
A woman seeking relief from symptoms of menopause would like to see how fezolintant compares with other available treatment options. But Astellas did not conduct such a study and Andrea LaCroix says it is unlikely that anyone ever will.
ICER has come the closest, with a side-by-side analysis of evidence-based treatments and found that fezolinetant performed quite similarly and modestly as the others in providing relief from hot flashes. Some treatments also help with other symptoms of menopause, which fezolinetant does not.
There are many coping strategies that women can adopt to deal with hot flashes; one of the most common is dressing in layers (such as a sleeveless blouse with a sweater) that can be added or subtracted as conditions require. Avoiding caffeine, hot liquids, and spicy foods is another common strategy. “I stopped drinking hot caffeinated drinks…for several years, and you get out of the habit of drinking them,” says Zuckerman.
LaCroix curates those options at My Meno Plan, which includes a search function where you can enter your symptoms and identify which treatments might work best for you. It also links to published research papers. She says the goal is to empower women with information to make informed decisions about menopause.
A company in England has made a test that picks out the compounds from breath that reveal if people have liver disease.
Every year, around two million people worldwide die of liver disease. While some people inherit the disease, it’s most commonly caused by hepatitis, obesity and alcoholism. These underlying conditions kill liver cells, causing scar tissue to form until eventually the liver cannot function properly. Since 1979, deaths due to liver disease have increased by 400 percent.
The sooner the disease is detected, the more effective treatment can be. But once symptoms appear, the liver is already damaged. Around 50 percent of cases are diagnosed only after the disease has reached the final stages, when treatment is largely ineffective.
To address this problem, Owlstone Medical, a biotech company in England, has developed a breath test that can detect liver disease earlier than conventional approaches. Human breath contains volatile organic compounds (VOCs) that change in the first stages of liver disease. Owlstone’s breath test can reliably collect, store and detect VOCs, while picking out the specific compounds that reveal liver disease.
“There’s a need to screen more broadly for people with early-stage liver disease,” says Owlstone’s CEO Billy Boyle. “Equally important is having a test that's non-invasive, cost effective and can be deployed in a primary care setting.”
The standard tool for detection is a biopsy. It is invasive and expensive, making it impractical to use for people who aren't yet symptomatic. Meanwhile, blood tests are less invasive, but they can be inaccurate and can’t discriminate between different stages of the disease.
In the past, breath tests have not been widely used because of the difficulties of reliably collecting and storing breath. But Owlstone’s technology could help change that.
The team is testing patients in the early stages of advanced liver disease, or cirrhosis, to identify and detect these biomarkers. In an initial study, Owlstone’s breathalyzer was able to pick out patients who had early cirrhosis with 83 percent sensitivity.
Boyle’s work is personally motivated. His wife died of colorectal cancer after she was diagnosed with a progressed form of the disease. “That was a big impetus for me to see if this technology could work in early detection,” he says. “As a company, Owlstone is interested in early detection across a range of diseases because we think that's a way to save lives and a way to save costs.”
How it works
In the past, breath tests have not been widely used because of the difficulties of reliably collecting and storing breath. But Owlstone’s technology could help change that.
Study participants breathe into a mouthpiece attached to a breath sampler developed by Owlstone. It has cartridges are designed and optimized to collect gases. The sampler specifically targets VOCs, extracting them from atmospheric gases in breath, to ensure that even low levels of these compounds are captured.
The sampler can store compounds stably before they are assessed through a method called mass spectrometry, in which compounds are converted into charged atoms, before electromagnetic fields filter and identify even the tiniest amounts of charged atoms according to their weight and charge.
The top four compounds in our breath
In an initial study, Owlstone captured VOCs in breath to see which ones could help them tell the difference between people with and without liver disease. They tested the breath of 46 patients with liver disease - most of them in the earlier stages of cirrhosis - and 42 healthy people. Using this data, they were able to create a diagnostic model. Individually, compounds like 2-Pentanone and limonene performed well as markers for liver disease. Owlstone achieved even better performance by examining the levels of the top four compounds together, distinguishing between liver disease cases and controls with 95 percent accuracy.
“It was a good proof of principle since it looks like there are breath biomarkers that can discriminate between diseases,” Boyle says. “That was a bit of a stepping stone for us to say, taking those identified, let’s try and dose with specific concentrations of probes. It's part of building the evidence and steering the clinical trials to get to liver disease sensitivity.”
Sabine Szunerits, a professor of chemistry in Institute of Electronics at the University of Lille, sees the potential of Owlstone’s technology.
“Breath analysis is showing real promise as a clinical diagnostic tool,” says Szunerits, who has no ties with the company. “Owlstone Medical’s technology is extremely effective in collecting small volatile organic biomarkers in the breath. In combination with pattern recognition it can give an answer on liver disease severity. I see it as a very promising way to give patients novel chances to be cured.”
Improving the breath sampling process
Challenges remain. With more than one thousand VOCs found in the breath, it can be difficult to identify markers for liver disease that are consistent across many patients.
Julian Gardner is a professor of electrical engineering at Warwick University who researches electronic sensing devices. “Everyone’s breath has different levels of VOCs and different ones according to gender, diet, age etc,” Gardner says. “It is indeed very challenging to selectively detect the biomarkers in the breath for liver disease.”
So Owlstone is putting chemicals in the body that they know interact differently with patients with liver disease, and then using the breath sampler to measure these specific VOCs. The chemicals they administer are called Exogenous Volatile Organic Compound) probes, or EVOCs.
Most recently, they used limonene as an EVOC probe, testing 29 patients with early cirrhosis and 29 controls. They gave the limonene to subjects at specific doses to measure how its concentrations change in breath. The aim was to try and see what was happening in their livers.
“They are proposing to use drugs to enhance the signal as they are concerned about the sensitivity and selectivity of their method,” Gardner says. “The approach of EVOC probes is probably necessary as you can then eliminate the person-to-person variation that will be considerable in the soup of VOCs in our breath.”
Through these probes, Owlstone could identify patients with liver disease with 83 percent sensitivity. By targeting what they knew was a disease mechanism, they were able to amplify the signal. The company is starting a larger clinical trial, and the plan is to eventually use a panel of EVOC probes to make sure they can see diverging VOCs more clearly.
“I think the approach of using probes to amplify the VOC signal will ultimately increase the specificity of any VOC breath tests, and improve their practical usability,” says Roger Yazbek, who leads the South Australian Breath Analysis Research (SABAR) laboratory in Flinders University. “Whilst the findings are interesting, it still is only a small cohort of patients in one location.”
The future of breath diagnosis
Owlstone wants to partner with pharmaceutical companies looking to learn if their drugs have an effect on liver disease. They’ve also developed a microchip, a miniaturized version of mass spectrometry instruments, that can be used with the breathalyzer. It is less sensitive but will enable faster detection.
Boyle says the company's mission is for their tests to save 100,000 lives. "There are lots of risks and lots of challenges. I think there's an opportunity to really establish breath as a new diagnostic class.”

