Rehabilitating psychedelic drugs: Another key to treating severe mental health disorders

A recent review paper found evidence that using psychedelics such as MDMA can help with treating a variety of common mental illnesses, but experts fear that research might easily be shut down in the future.
Lori Tipton's life was a cascade of trauma that even a soap opera would not dare inflict upon a character: a mentally unstable family; a brother who died of a drug overdose; the shocking discovery of the bodies of two persons her mother had killed before turning the gun on herself; the devastation of Hurricane Katrina that savaged her hometown of New Orleans; being raped by someone she trusted; and having an abortion. She suffered from severe PTSD.
“My life was filled with anxiety and hypervigilance,” she says. “I was constantly afraid and had mood swings, panic attacks, insomnia, intrusive thoughts and suicidal ideation. I tried to take my life more than once.” She was fortunate to be able to access multiple mental health services, “And while at times some of these modalities would relieve the symptoms, nothing really lasted and nothing really address the core trauma.”
Then in 2018 Tipton enrolled in a clinical trial that combined intense sessions of psychotherapy with limited use of Methylenedioxymethamphetamine, or MDMA, a drug classified as a psychedelic and commonly known as ecstasy or Molly. The regimen was arduous; 1-2 hour preparation sessions, three sessions where MDMA was used, which lasted 6-8 hours, and lengthy sessions afterward to process and integrate the experiences. Two therapists were with her every moment of the three-month program that totaled more than 40 hours.
“It was clear to me that [the therapists] weren't going to heal me, that I was going to have to do the work for myself, but that they were there to completely support my process,” she says. “But the effects of MDMA were really undeniable for me. I felt embodied in a way that I hadn't in years. PTSD had robbed me of the ability to feel safe in my own body.”
Tipton doesn’t think the therapy completely cured her PTSD. “But when I completed the trial in 2018, I no longer qualified for the diagnosis, and I still don't qualify for the diagnosis today,” she told an April workshop on psychedelics as mental health treatment by the National Academies of Sciences, Engineering and Medicine, or NASEM.
A Champion
Rick Doblin has been a catalyst behind much of the contemporary research into psychedelics. Prior to the DEA clamp down, the Boston psychotherapist had seen that MDMA and other psychedelics could benefit some of his patients where other measures had failed. He immediately organized efforts to question the drug rescheduling but to little avail. In 1986, he created the nonprofit Multidisciplinary Association for Psychedelic Studies (MAPS), which slowly laid the scientific foundation for clinical trials, including the one that Tipton joined, using psychedelics to treat mental health conditions.
Now, only slowly, have researchers been able to explore the power of these drugs to treat a broad spectrum of severely debilitating mental health conditions, including trauma, depression, and PTSD, where other available treatments proved inadequate.
“Psychedelic psychotherapy is an attempt to go after the root causes of the problems with just a relatively few administrations, as contrasted to most of the psychiatric drugs used today that are mostly just reducing symptoms and are meant to be taken on a daily basis,” Doblin said in a 2019 TED Talk. Most of these drugs can have broad effect but “some are probably more effective than others for certain conditions,” he added in a recent interview with Leaps.org. Comparative head-to-head studies of psychedelic therapies simply have not been conducted.
Their mechanisms of action are poorly understood and can vary between drugs, but it is generally believed that psychedelics change the activity of neurons so that the brain processes information differently, says Katrin Preller, a neuropsychologist at the University of Zurich. A recent important study in Nature Medicine by Richard Daws and colleagues used functional magnetic resonance imaging (fMRI) of the brain and found that “functional networks became more functionally interconnected and flexible after psilocybin treatment…implying that psilocybin's antidepressant action may depend on a global increase in brain network integration.”
Rosalind Watts, a clinical investigator at the Imperial College in London, believes there is “an overestimation of the importance of the drug and an underestimation of the importance of the [therapeutic] context” in psychedelic research. “It is unethical to provide the drug without the other,” she says. Doblin notes that “psychotherapy outcomes research demonstrates that the therapeutic alliance between the therapist and the patients is the single most predictive factor of outcomes. [It is] trust and the sense of safety, the willingness to go into difficult spaces” that makes clinical breakthroughs possible with the drug.
Excitement and Challenges
Recurrent themes expressed at the NASEM workshop were exciting glimpses of the potential for psychedelics to treat mental health conditions combined with the challenges of realizing those potentials. A recent review paper found evidence that using psychedelics can help with treating a variety of common mental illnesses, but the paper could identify only 14 clinical trials of classic psychedelics published since 1991. Much of the reason is that the drugs are not patentable and so the pharmaceutical industry has no interest in investing in expensive clinical trials to bring them to market. MAPS has raised about $135 million over its 36-year history to conduct such research, says Doblin, the vast majority of it from individual donors and none from foundations.
The workshop participants’ views also were colored by the history of drug crackdowns and a fear that research might easily be shut down in the future. There was great concern that use of psychedelics should be confined to clinical trials with high safety and ethical standards, instead of doctors and patients experimenting on their own. “We need to get it right this time,” says Charles Grob, a psychiatrist at the UCLA School of Medicine. But restricting access to psychedelics will become even more difficult now that Oregon and several cities have acted to decriminalize possession and use of many of these drugs.
The experience with ketamine also troubled Grob. He is hoping to “mitigate the rush of rapid commercialization” that occurred with that drug. Ketamine technically is not a psychedelic though it does share some of their potentially euphoric properties. In 2019, soon after the FDA approved a form of ketamine with a limited label indication to treat depression, for profit clinics sprang up promoting off label use of the drug for psychiatric conditions where there was little clinical evidence of efficacy. He fears the same thing will happen when true psychedelics are made available.
If these therapies are approved, access to them is likely to be a problem. The drugs themselves are cheap but the accompanying therapy is not, and there is a shortage of trained psychotherapists. Mental health services often are not adequately covered by health insurance, while the poor and people of color suffer additional burdens of inadequate access. Doblin is committed to health care equity by training additional providers and by investigating whether some of the preparatory and integration sessions might be handled in a group setting. He says it is important that the legal aspects of psychedelics also be addressed so that patients “don't have to go underground” in order to receive this care.
Donna Shirley pictured at her home in Tulsa, with a model of the Sojourner rover she was in charge of that explored Mars.
When NASA's Perseverance rover landed successfully on Mars on February 18, 2021, calling it "one giant leap for mankind" – as Neil Armstrong said when he set foot on the moon in 1969 – would have been inaccurate. This year actually marked the fifth time the U.S. space agency has put a remote-controlled robotic exploration vehicle on the Red Planet. And it was a female engineer named Donna Shirley who broke new ground for women in science as the manager of both the Mars Exploration Program and the 30-person team that built Sojourner, the first rover to land on Mars on July 4, 1997.
For Shirley, the Mars Pathfinder mission was the climax of her 32-year career at NASA's Jet Propulsion Laboratory (JPL) in Pasadena, California. The Oklahoma-born scientist, who earned her Master's degree in aerospace engineering from the University of Southern California, saw her profile skyrocket with media appearances from CNN to the New York Times, and her autobiography Managing Martians came out in 1998. Now 79 and living in a Tulsa retirement community, she still embraces her status as a female pioneer.
"Periodically, I'll hear somebody say they got into the space program because of me, and that makes me feel really good," Shirley told Leaps.org. "I look at the mission control area, and there are a lot of women in there. I'm quite pleased I was able to break the glass ceiling."
Her $25-million, 25-pound microrover – powered by solar energy and designed to get rock samples and test soil chemistry for evidence of life – was named after Sojourner Truth, a 19th-century Black abolitionist and women's rights activist. Unlike Mars Pathfinder, Shirley didn't have to travel more than 131 million miles to reach her goal, but her path to scientific fame as a woman sometimes resembled an asteroid field.
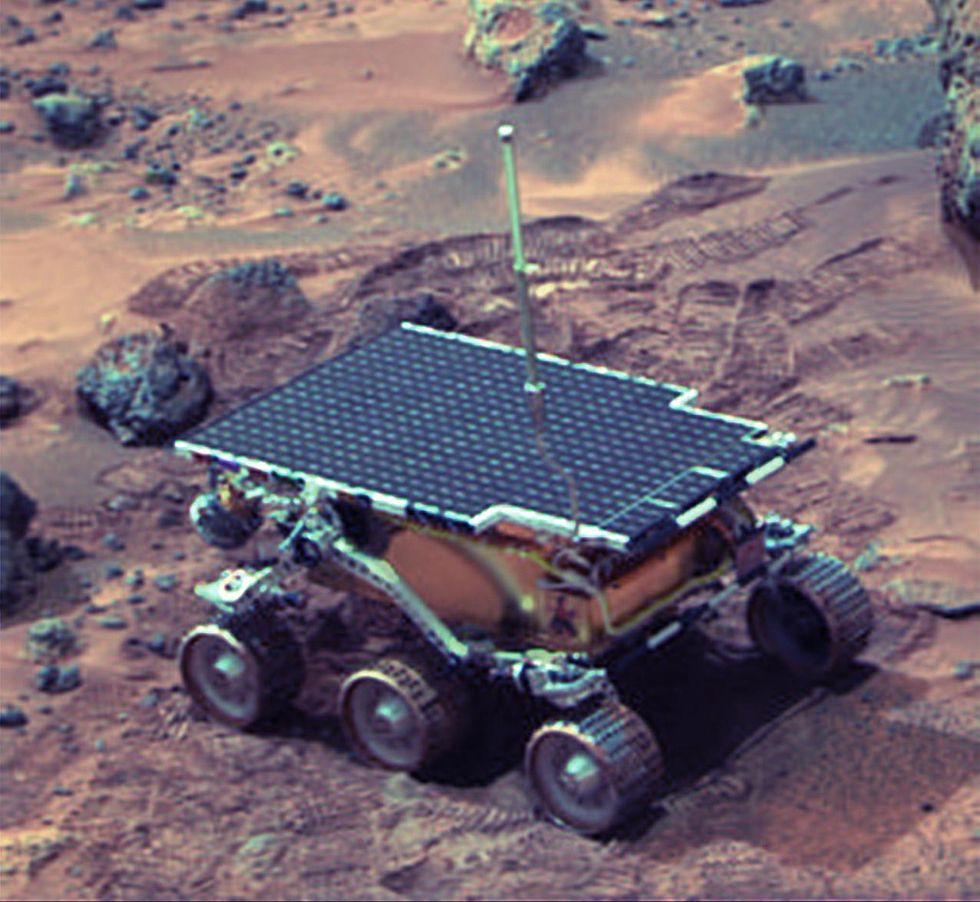 The Sojourner Rover in 1997 on Mars.NASA/JPL
The Sojourner Rover in 1997 on Mars.NASA/JPLAs a high-IQ tomboy growing up in Wynnewood, Oklahoma (pop. 2,300), Shirley yearned to escape. She decided to become an engineer at age 10 and took flying lessons at 15. Her extraterrestrial aspirations were fueled by Ray Bradbury's The Martian Chronicles and Arthur C. Clarke's The Sands of Mars. Yet when she entered the University of Oklahoma (OU) in 1958, her freshman academic advisor initially told her: "Girls can't be engineers." She ignored him.
Years later, Shirley would combat such archaic thinking, succeeding at JPL with her creative, collaborative management style. "If you look at the literature, you'll find that teams that are either led by or heavily involved with women do better than strictly male teams," she noted.
However, her career trajectory stalled at OU. Burned out by her course load and distracted by a broken engagement to marry a fellow student, she switched her major to professional writing. After graduation, she applied her aeronautical background as a McDonnell Aircraft technical writer, but her boss, she says, harassed her and she faced gender-based hostility from male co-workers.
Returning to OU, Shirley finished off her engineering degree and became a JPL aerodynamist in 1966 after answering an ad in the St. Louis Post-Dispatch. At first, she was the only female engineer among the research center's 2,000-odd engineers. She wore many hats, from designing planetary atmospheric entry vehicles to picking the launch date of November 4, 1973 for Mariner 10's mission to Venus and Mercury.
By the mid-1980's, she was managing teams that focused on robotics and Mars, delivering creative solutions when NASA budget cuts loomed. In 1989, the same year the Sojourner microrover concept was born, President George H.W. Bush announced his Space Exploration Initiative, including plans for a human mission to Mars by 2019.
That target, of course, wasn't attained, despite huge advances in technology and our understanding of the Martian environment. Today, Shirley believes humans could land on Mars by 2030. She became the founding director of the Science Fiction Museum and Hall of Fame in Seattle in 2004 after leaving NASA, and to this day, she enjoys checking out pop culture portrayals of Mars landings – even if they're not always accurate.
After the novel The Martian was published in 2011, which later was adapted into the hit film starring Matt Damon, Shirley phoned author Andy Weir: "You've got a major mistake in here. It says there's a storm that tries to blow the rocket over. But actually, the Mars atmosphere is so thin, it would never blow a rocket over!"
Fearlessly speaking her mind and seeking the stars helped Donna Shirley make history. However, a 2019 Washington Post story noted: "Women make up only about a third of NASA's workforce. They comprise just 28 percent of senior executive leadership positions and are only 16 percent of senior scientific employees." Whether it's traveling to Mars or trending toward gender equality, we've still got a long way to go.
Announcing March Event: "COVID Vaccines and the Return to Life: Part 1"
Leading medical and scientific experts will discuss the latest developments around the COVID-19 vaccines at our March 11th event.
EVENT INFORMATION
DATE:
Thursday, March 11th, 2021 at 12:30pm - 1:45pm EST
On the one-year anniversary of the global declaration of the pandemic, this virtual event will convene leading scientific and medical experts to discuss the most pressing questions around the COVID-19 vaccines. Planned topics include the effect of the new circulating variants on the vaccines, what we know so far about transmission dynamics post-vaccination, how individuals can behave post-vaccination, the myths of "good" and "bad" vaccines as more alternatives come on board, and more. A public Q&A will follow the expert discussion.
CONTACT:
kira@goodinc.com
LOCATION:
Zoom webinar
SPEAKERS:

Dr. Paul Offit speaking at Communicating Vaccine Science.
commons.wikimedia.orgDr. Paul Offit, M.D., is the director of the Vaccine Education Center and an attending physician in infectious diseases at the Children's Hospital of Philadelphia. He is a co-inventor of the rotavirus vaccine for infants, and he has lent his expertise to the advisory committees that review data on new vaccines for the CDC and FDA.

Dr. Monica Gandhi
UCSF Health
Dr. Monica Gandhi, M.D., MPH, is Professor of Medicine and Associate Division Chief (Clinical Operations/ Education) of the Division of HIV, Infectious Diseases, and Global Medicine at UCSF/ San Francisco General Hospital.

Dr. Onyema Ogbuagu, MBBCh, FACP, FIDSA
Yale Medicine
Dr. Onyema Ogbuagu, MBBCh, is an infectious disease physician at Yale Medicine who treats COVID-19 patients and leads Yale's clinical studies around COVID-19. He ran Yale's trial of the Pfizer/BioNTech vaccine.

Dr. Eric Topol
Dr. Topol's Twitter
Dr. Eric Topol, M.D., is a cardiologist, scientist, professor of molecular medicine, and the director and founder of Scripps Research Translational Institute. He has led clinical trials in over 40 countries with over 200,000 patients and pioneered the development of many routinely used medications.
REGISTER NOW
This event is the first of a four-part series co-hosted by LeapsMag, the Aspen Institute Science & Society Program, and the Sabin–Aspen Vaccine Science & Policy Group, with generous support from the Gordon and Betty Moore Foundation and the Howard Hughes Medical Institute.

Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.