Regrowing Amputated Limbs Is Getting Closer to Medical Reality

Kirstie Ennis, an Afghanistan veteran who survived a helicopter crash but lost a limb, pictured in May 2021 at Two Rivers Park in Colorado.
In June 2012, Kirstie Ennis was six months into her second deployment to Afghanistan and recently promoted to sergeant. The helicopter gunner and seven others were three hours into a routine mission of combat resupplies and troop transport when their CH-53D helicopter went down hard.
Miraculously, all eight people onboard survived, but Ennis' injuries were many and severe. She had a torn rotator cuff, torn labrum, crushed cervical discs, facial fractures, deep lacerations and traumatic brain injury. Despite a severely fractured ankle, doctors managed to save her foot, for a while at least.
In November 2015, after three years of constant pain and too many surgeries to count, Ennis relented. She elected to undergo a lower leg amputation but only after she completed the 1,000-mile, 72-day Walking with the Wounded journey across the UK.
On Veteran's Day of that year, on the other side of the country, orthopedic surgeon Cato Laurencin announced a moonshot challenge he was setting out to achieve on behalf of wounded warriors like Ennis: the Hartford Engineering A Limb (HEAL) Project.
Laurencin, who is a University of Connecticut professor of chemical, materials and biomedical engineering, teamed up with experts in tissue bioengineering and regenerative medicine from Harvard, Columbia, UC Irvine and SASTRA University in India. Laurencin and his colleagues at the Connecticut Convergence Institute for Translation in Regenerative Engineering made a bold commitment to regenerate an entire limb within 15 years – by the year 2030.
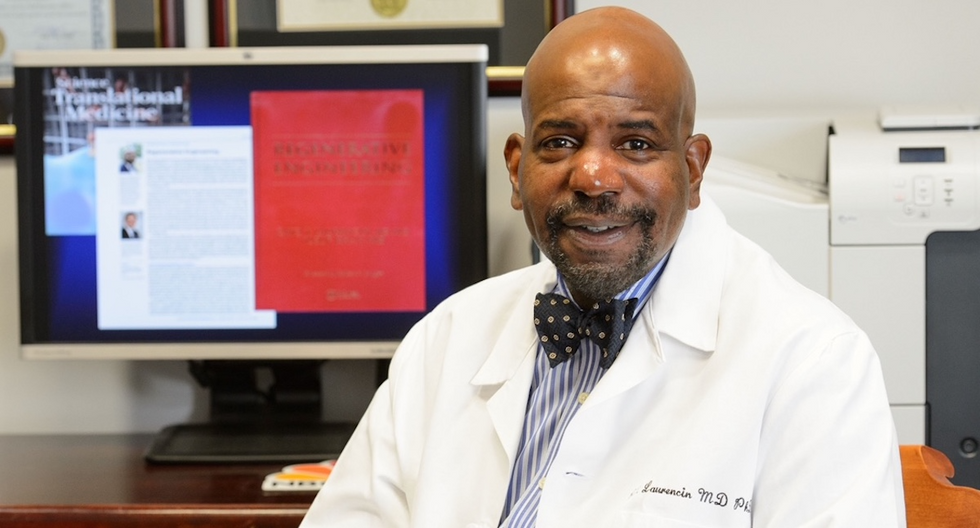
Dr. Cato Laurencin pictured in his office at UConn.
Photo Credit: UConn
Regenerative Engineering -- A Whole New Field
Limb regeneration in humans has been a medical and scientific fascination for decades, with little to show for the effort. However, Laurencin believes that if we are to reach the next level of 21st century medical advances, this puzzle must be solved.
An estimated 185,000 people undergo upper or lower limb amputation every year. Despite the significant advances in electromechanical prosthetics, these individuals still lack the ability to perform complex functions such as sensation for tactile input, normal gait and movement feedback. As far as Laurencin is concerned, the only clinical answer that makes sense is to regenerate a whole functional limb.
Laurencin feels other regeneration efforts were hampered by their siloed research methods with chemists, surgeons, engineers all working separately. Success, he argues, requires a paradigm shift to a trans-disciplinary approach that brings together cutting-edge technologies from disparate fields such as biology, material sciences, physical, chemical and engineering sciences.
As the only surgeon ever inducted into the academies of Science, Medicine and Innovation, Laurencin is uniquely suited for the challenge. He is regarded as the founder of Regenerative Engineering, defined as the convergence of advanced materials sciences, stem cell sciences, physics, developmental biology and clinical translation for the regeneration of complex tissues and organ systems.
But none of this is achievable without early clinician participation across scientific fields to develop new technologies and a deeper understanding of how to harness the body's innate regenerative capabilities. "When I perform a surgical procedure or something is torn or needs to be repaired, I count on the body being involved in regenerating tissue," he says. "So, understanding how the body works to regenerate itself and harnessing that ability is an important factor for the regeneration process."
The Birth of the Vision
Laurencin's passion for regeneration began when he was a sports medicine fellow at Cornell University Medical Center in the early 1990s. There he saw a significant number of injuries to the anterior cruciate ligament (ACL), the major ligament that stabilizes the knee. He believed he could develop a better way to address those injuries using biomaterials to regenerate the ligament. He sketched out a preliminary drawing on a napkin one night over dinner. He has spent the next 30 years regenerating tissues, including the patented L-C ligament.
As chair of Orthopaedic Surgery at the University of Virginia during the peak of the wars in Iraq and Afghanistan, Laurencin treated military personnel who survived because of improved helmets, body armor and battlefield medicine but were left with more devastating injuries, including traumatic brain injuries and limb loss.
"I was so honored to care for them and I so admired their steadfast courage that I became determined to do something big for them," says Laurencin.
When he tells people about his plans to regrow a limb, he gets a lot of eye rolls, which he finds amusing but not discouraging. Growing bone cells was relatively new when he was first focused on regenerating bone in 1987 at MIT; in 2007 he was well on his way to regenerating ligaments at UVA when many still doubted that ligaments could even be reconstructed. He and his team have already regenerated torn rotator cuff tendons and ACL ligaments using a nano-textured fabric seeded with stem cells.
Even as a finalist for the $4 million NIH Pioneer Award for high-risk/high-reward research, he faced a skeptical scientific audience in 2014. "They said, 'Well what do you plan to do?' I said 'I plan to regenerate a whole limb in people.' There was a lot of incredulousness. They stared at me and asked a lot of questions. About three days later, I received probably the best score I've ever gotten on an NIH grant."
In the Thick of the Science
Humans are born with regenerative abilities--two-year-olds have regrown fingertips--but lose that ability with age. Salamanders are the only vertebrates that can regenerate lost body parts as adults; axolotl, the rare Mexican salamander, can grow extra limbs.
The axolotl is important as a model organism because it is a four-footed vertebrate with a similar body plan to humans. Mapping the axolotl genome in 2018 enhanced scientists' genetic understanding of their evolution, development, and regeneration. Being easy to breed in captivity allowed the HEAL team to closely study these amphibians and discover a new cell type they believe may shed light on how to mimic the process in humans.
"Whenever limb regeneration takes place in the salamander, there is a huge amount of something called heparan sulfate around that area," explains Laurencin. "We thought, 'What if this heparan sulfate is the key ingredient to allowing regeneration to take place?' We found these groups of cells that were interspersed in tissues during the time of regeneration that seemed to have connections to each other that expressed this heparan sulfate."
Called GRID (Groups that are Regenerative, Interspersed and Dendritic), these cells were also recently discovered in mice. While GRID cells don't regenerate as well in mice as in salamanders, finding them in mammals was significant.
"If they're found in mice. we might be able to find these in humans in some form," Laurencin says. "We think maybe it will help us figure out regeneration or we can create cells that mimic what grid cells do and create an artificial grid cell."
What Comes Next?
Laurencin and his team have individually engineered and made every single tissue in the lower limb, including bone, cartilage, ligament, skin, nerve, blood vessels. Regenerating joints and joint tissue is the next big mile marker, which Laurencin sees as essential to regenerating a limb that functions and performs in the way he envisions.
"Using stem cells and amnion tissue, we can regenerate joints that are damaged, and have severe arthritis," he says. "We're making progress on all fronts, and making discoveries we believe are going to be helping people along the way."
That focus and advancement is vital to Ennis. After laboring over the decision to have her leg amputated below the knee, she contracted MRSA two weeks post-surgery. In less than a month, she went from a below-the-knee-amputee to a through-the-knee amputee to an above-the-knee amputee.
"A below-the-knee amputation is night-and-day from above-the-knee," she said. "You have to relearn everything. You're basically a toddler."

Kirstie Ennis pictured in July 2020.
Photo Credit: Ennis' Instagram
The clock is ticking on the timeline Laurencin set for himself. Nine years might seem like forever if you're doing time but it might appear fleeting when you're trying to create something that's never been done before. But Laurencin isn't worried. He's convinced time is on his side.
"Every week, I receive an email or a call from someone, maybe a mother whose child has lost a finger or I'm in communication with a disabled American veteran who wants to know how the progress is going. That energizes me to continue to work hard to try to create these sorts of solutions because we're talking about people and their lives."
He devotes about 60 hours a week to the project and the roughly 100 students, faculty and staff who make up the HEAL team at the Convergence Institute seem acutely aware of what's at stake and appear equally dedicated.
"We're in the thick of the science in terms of making this happen," says Laurencin. "We've moved from making the impossible possible to making the possible a reality. That's what science is all about."
In this week's Friday Five, breathing this way may cut down on anxiety, a fasting regimen that could make you sick, this type of job makes men more virile, 3D printed hearts could save your life, and the role of metformin in preventing dementia.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Here are the promising studies covered in this week's Friday Five, featuring interviews with Dr. David Spiegel, associate chair of psychiatry and behavioral sciences at Stanford, and Dr. Filip Swirski, professor of medicine and cardiology at the Icahn School of Medicine at Mount Sinai.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Here are the promising studies covered in this week's Friday Five, featuring interviews with Dr. David Spiegel, associate chair of psychiatry and behavioral sciences at Stanford, and Dr. Filip Swirski, professor of medicine and cardiology at the Icahn School of Medicine at Mount Sinai.
- Breathing this way cuts down on anxiety*
- Could your fasting regimen make you sick?
- This type of job makes men more virile
- 3D printed hearts could save your life
- Yet another potential benefit of metformin
* This video with Dr. Andrew Huberman of Stanford shows exactly how to do the breathing practice.
This podcast originally aired on March 3, 2023.
Breakthrough drones deliver breast milk in rural Uruguay
A drone hovers over Tacuarembó hospital in Uruguay, carrying its precious cargo: breast milk intended for children in remote parts of the country.
Until three months ago, nurse Leopoldina Castelli used to send bottles of breast milk to nourish babies in the remote areas of Tacuarembó, in northern Uruguay, by way of ambulances or military trucks. That is, if the vehicles were available and the roads were passable, which wasn’t always the case. Now, five days per week, she stands by a runway at the hospital, located in Tacuarembó’s capital, watching a drone take off and disappear from view, carrying the milk to clinics that serve the babies’ families.
The drones can fly as far as 62 miles. Long distances and rough roads are no obstacles. The babies, whose mothers struggle to produce sufficient milk and cannot afford formula, now receive ample supplies for healthy growth. “Today we provided nourishment to a significantly larger number of children, and this is something that deeply moves me,” Castelli says.
About two decades ago, the Tacuarembó hospital established its own milk bank, supported by donations from mothers across Tacuarembó. Over the years, the bank has provided milk to infants immediately after birth. It's helped drive a “significant and sustained” decrease in infant mortality, says the hospital director, Ciro Ferreira.
But these children need breast milk throughout their first six months, if not longer, to prevent malnutrition and other illnesses that are prevalent in rural Tacuarembó. Ground transport isn't quick or reliable enough to meet this goal. It can take several hours, during which the milk may spoil due to a lack of refrigeration.
The battery-powered drones have been the difference-maker. The project to develop them, financed by the UNICEF Innovation Fund, is the first of its kind in Latin America. To Castelli, it's nothing short of a revolution. Tacuarembó Hospital, along with three rural clinics in the most impoverished part of Uruguay, are its leaders.
"This marks the first occasion when the public health system has been directly impacted [by our technology]," says Sebastián Macías, the CEO and co-founder of Cielum, an engineer at the University Republic, which collaborated on the technology with a Uruguayan company called Cielum and a Swiss company, Rigitech.
The drone can achieve a top speed of up to 68 miles per hour, is capable of flying in light rain, and can withstand winds of up to 30 miles per hour at a maximum altitude of 120 meters.
"We have succeeded in embracing the mothers from rural areas who were previously slipping through the cracks of the system," says Ferreira, the hospital director. He envisions an expansion of the service so it can improve health for children in other rural areas.

Nurses load the drone for breast milk delivery.
Sebastián Macías - Cielum
The star aircraft
The drone, which costs approximately $70,000, was specifically designed for the transportation of biological materials. Constructed from carbon fiber, it's three meters wide, two meters long and weighs 42 pounds when fully loaded. Additionally, it is equipped with a ballistic parachute to ensure a safe descent in case the technology fails in midair. Furthermore, it can achieve a top speed of 68 miles per hour, fly in light rain, and withstand winds of 30 miles per hour at a height of 120 meters.
Inside, the drones feature three refrigerated compartments that maintain a stable temperature and adhere to the United Nations’ standards for transporting perishable products. These compartments accommodate four gallons or 6.5 pounds of cargo. According to Macías, that's more than sufficient to carry a week’s worth of milk for one infant on just two flights, or 3.3 pounds of blood samples collected in a rural clinic.
“From an energy perspective, it serves as an efficient mode of transportation and helps reduce the carbon emissions associated with using an ambulance,” said Macías. Plus, the ambulance can remain available in the town.
Macías, who has led software development for the drone, and three other technicians have been trained to operate it. They ensure that the drone stays on course, monitor weather conditions and implement emergency changes when needed. The software displays the in-flight positions of the drones in relation to other aircraft. All agricultural planes in the region receive notification about the drone's flight path, departure and arrival times, and current location.
The future: doubling the drone's reach
Forty-five days after its inaugural flight, the drone is now making five flights per week. It serves two routes: 34 miles to Curtina and 31 miles to Tambores. The drone reaches Curtina in 50 minutes while ambulances take double that time, partly due to the subpar road conditions. Pueblo Ansina, located 40 miles from the state capital, will soon be introduced as the third destination.
Overall, the drone’s schedule is expected to become much busier, with plans to accomplish 20 weekly flights by the end of October and over 30 in 2024. Given the drone’s speed, Macías is contemplating using it to transport cancer medications as well.
“When it comes to using drones to save lives, for us, the sky is not the limit," says Ciro Ferreira, Tacuarembó hospital director.
In future trips to clinics in San Gregorio de Polanco and Caraguatá, the drone will be pushed to the limit. At these locations, a battery change will be necessary, but it's worth it. The route will cover up to 10 rural Tacuarembó clinics plus one hospital outside Tacuarembó, in Rivera, close to the border with Brazil. Currently, because of a shortage of ambulances, the delivery of pasteurized breast milk to Rivera only occurs every 15 days.
“The expansion to Rivera will include 100,000 more inhabitants, doubling the healthcare reach,” said Ferreira, the director of the Tacuarembó Hospital. In itself, Ferreira's hospital serves the medical needs of 500,000 people as one of the largest in Uruguay's interior.
Alejandro Del Estal, an aeronautical engineer at Rigitech, traveled from Europe to Tacuarembó to oversee the construction of the vertiports – the defined areas that can support drones’ take-off and landing – and the first flights. He pointed out that once the flight network between hospitals and rural polyclinics is complete in Uruguay, it will rank among the five most extensive drone routes in the world for any activity, including healthcare and commercial uses.
Cielum is already working on the long-term sustainability of the project. The aim is to have more drones operating in other rural regions in the western and northern parts of the country. The company has received inquiries from Argentina and Colombia, but, as Macías pointed out, they are exercising caution when making commitments. Expansion will depend on the development of each country’s regulations for airspace use.
For Ferreira, the advantages in Uruguay are evident: "This approach enables us to bridge the geographical gap, enhance healthcare accessibility, and reduce the time required for diagnosing and treating rural inhabitants, all without the necessity of them traveling to the hospital,” he says. "When it comes to using drones to save lives, for us, the sky is not the limit."