Researchers Are Experimenting With Magic Mushrooms' Fascinating Ability to Improve Mental Health Disorders

Magic mushrooms, in conjunction with a psychotherapist's treatment, may be helpful in treating addiction, depression, anxiety, and other mental health ailments.
Mental illness is a dark undercurrent in the lives of tens of millions of Americans. According to the World Health Organization, about 450 million people worldwide have a mental health disorder, which cut across all demographics, cultures, and socioeconomic classes.
One area of research seems to herald the first major breakthrough in decades — hallucinogen-assisted psychotherapy.
The U.S. National Institute on Mental Health estimates that severely debilitating mental health disorders cost the U.S. more than $300 billion per year, and that's not even counting the human toll of broken lives, devastated families, and a health care system stretched to the limit.
However, one area of research seems to herald the first major breakthrough in decades — hallucinogen-assisted psychotherapy. Drugs like psilocybin (obtained from "magic mushrooms"), LSD, and MDMA (known as the club drug, ecstasy) are being tested in combination with talk therapy for a variety of mental illnesses. These drugs, administered by a psychotherapist in a safe and controlled environment, are showing extraordinary results that other conventional treatments would take years to accomplish.
But the therapy will likely continue to face an uphill legal battle before it achieves FDA approval. It is up against not only current drug laws (all psychedelics remain illegal on the federal level) and strict FDA regulations, but a powerful status quo that has institutionalized fear of any drug used for recreational purposes.
How We Got Here
According to researchers Sean Belouin and Jack Henningfield, the use of psychedelic drugs has a long and winding history. It's believed that hallucinogenic substances have been used in healing ceremonies and religious rituals for thousands of years. Indigenous people in the U.S., Mexico, and Central and South America still use distillations from the peyote cactus and other hallucinogens in their religious ceremonies. And psilocybin mushrooms, also capable of causing hallucinations, grow throughout the world and are thought to have been used for millennia.
But psychedelic drugs didn't receive much research until 1943, when LSD's psychoactive effects were discovered by chemist Albert Hoffman. Hoffman tested the compound he had discovered years earlier on himself and found that the drug had profound mind-altering effects. He made the drug available to psychiatrists who were interested in testing it out as an adjunct to talk therapy. There were no truly effective drugs at the time for mental illnesses, and psychiatrists early on saw the possibility of psychedelics providing a kind of emotional catharsis that might represent therapeutic breakthroughs for many mental conditions.
During the 1950s and early 1960s, psychedelic drugs saw an increase in use within psychology, according to a 2018 article in Neuropharmacology. During this time, research on LSD and other hallucinogens was the subject of over 1,000 scientific papers, six international conferences, and several dozen books. LSD was widely prescribed to psychiatric patients, and by 1958, Hoffman had identified psilocybin as the hallucinogenic in "magic mushrooms," which was also administered. By 1965 some type of hallucinogenic had been given to more than 40,000 patients.
Then came a sea change. Psychedelic drugs caught the public's attention and there was widespread experimentation. The association with Hippie counterculture alarmed many and led to a legal and cultural backlash that stigmatized psychedelics for decades to come. In the mid-1960s, psychedelics were designated Schedule 1 drugs in the U.S., meaning they were seen as having "no accepted medical use and a high potential of abuse." Schedule 1 also implied that the drugs were more dangerous than cocaine, methamphetamine, Vicodin, and oxycodone, a perception that was far from proven but became an institutionalized part of drug enforcement. Medical use ceased and research dwindled down to close to zero.
For years, research into hallucinogenic-assisted therapy was basically dormant, until the 1990s when interest started to revive. In the 2000s, the first modern clinical trials of psilocybin were done by Francisco Moreno at the University of Arizona and Matthew Johnson at Johns Hopkins. Scientists in the 2010s, including Robin Carhart-Harris, started studying the use of psychedelics in the treatment of major depressive disorder (MDD).
In small trials with these patients, results showed significant and long-term improvement (for at least six months) after only two episodes of psilocybin-assisted therapy. In several studies, the guided experience of administering one of the psychedelic drugs along with psychotherapy seemed to result in marked improvement in a variety of disorders, including depression, anxiety, PTSD, and addiction.
The drugs allowed patients to experience a radical reframing of reality, helping them to become "unstuck" from the anxious and negative tape loops that played in their heads. According to Michael Pollan, an American author and professor of journalism who wrote the book, "How to Change Your Mind: What the New Science of Psychedelics Teaches Us About Consciousness, Dying, Addiction, Depression and Transcendence," psychedelics allow patients to see their lives through a kind of wide angle, where boundaries vanish and they're able to experience "consciousness without self." This perspective is usually accompanied by profound feelings of oneness with the universe.
Pollan likens the effect to a fresh blanketing of snow over the deep ruts of unproductive thinking, which characterize depression and other mental disorders. Once the new snow has fallen, the ruts disappear and a new path can be chosen. Relief from symptoms comes immediately, and in numerous studies, is sustained for months.
In spite of growing evidence for the safety and efficacy of psychedelic-assisted psychotherapy, the practice has major hurdles to cross on its quest for FDA approval.
Some of the most influential studies have focused on testing the use of psilocybin to treat end-of-life anxiety in patients diagnosed with a terminal illness. In 2016, Stephen Ross and colleagues tested a single dose of psilocybin on 29 subjects with end-of-life anxiety due to a terminal cancer diagnosis. A control group received a niacin pill. The researchers reported that of the 29 receiving psilocybin, all of the patients had "immediate, substantial, and sustained clinical benefits," even after six months.
In spite of growing evidence for the safety and efficacy of psychedelic-assisted psychotherapy, the practice has major hurdles to cross on its quest for FDA approval. The National Institutes of Health is not currently supporting any clinical trials and the research relies on private sources of funding, often with small research organizations that cannot afford the high cost of clinical trials.
Given the controversial nature of the drugs, researchers in psychedelic-assisted therapies may be cautious about publicity. Leapsmag reached out to several leaders in the field but none agreed to an interview.
Looking Ahead
Still, interest is building in the combination of psychedelic drugs and psychotherapy for treatment-resistant mental illnesses. Two months ago, Johns Hopkins University launched a new psychedelic research center with an infusion of $17 million from private investors. The center will focus on psychedelic-assisted therapies for opioid addiction, Alzheimer's disease, PTSD and major depression, to name just a few. Currently, of 51 cancer patients enrolled in a Hopkins study, more than half reported a decrease in depression and anxiety after receiving therapy with psilocybin. Two thirds even claimed that the experience was one of the most meaningful of their lives.
It is not unheard of for Schedule 1 drugs to make their way into medical use if they're shown to provide a bonafide improvement in a medical condition through well-designed clinical trials. MDMA, for example, has been designated a Breakthrough Therapy by the FDA as part of an Investigational New Drug Application. The FDA has agreed to a special protocol assessment that could speed up phase three clinical trials. The next step is for the data to be submitted to the FDA for an in-depth regulatory review. If the FDA agrees, MDMA-assisted therapy could be legalized.
Will the positive buzz around psychedelics persuade the NIH to provide the millions of dollars needed to push the field forward?
Robin Carhart-Harris believes the first drug that will receive FDA clearance is psilocybin, which he speculates could become legal in the next five to ten years. However, the field of psychedelic-assisted therapy needs more and larger clinical trials, preferably with the support of the NIH.
As Rucker and colleagues noted, the scientific literature bends toward the theme that the drugs are not necessarily therapeutic in and of themselves. It's the use of hallucinogens within a "psychologically supportive context" with a trained expert that's helpful. It's currently unknown how many users of recreational drugs are self-medicating for depression, anxiety, or other mental illnesses. But without the guidance of a knowledgeable psychotherapist, those who are self-medicating may not be helping themselves at all.
Will the positive buzz around psychedelics persuade the NIH to provide the millions of dollars needed to push the field forward? Given the changing climate in public opinion around these drugs and the need for breakthroughs in mental health therapies, it's possible that in the foreseeable future, this bold new therapy will become part of the mental health arsenal.
A robot server, controlled remotely by a disabled worker, delivers drinks to patrons at the DAWN cafe in Tokyo.
A sleek, four-foot tall white robot glides across a cafe storefront in Tokyo’s Nihonbashi district, holding a two-tiered serving tray full of tea sandwiches and pastries. The cafe’s patrons smile and say thanks as they take the tray—but it’s not the robot they’re thanking. Instead, the patrons are talking to the person controlling the robot—a restaurant employee who operates the avatar from the comfort of their home.
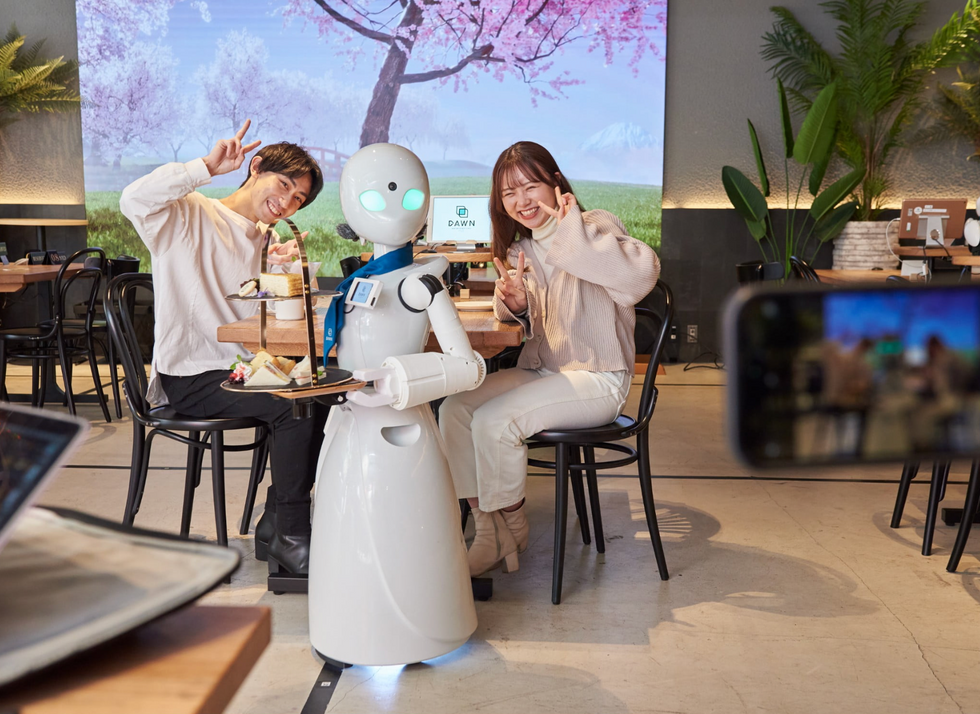
It’s a typical scene at DAWN, short for Diverse Avatar Working Network—a cafe that launched in Tokyo six years ago as an experimental pop-up and quickly became an overnight success. Today, the cafe is a permanent fixture in Nihonbashi, staffing roughly 60 remote workers who control the robots remotely and communicate to customers via a built-in microphone.
More than just a creative idea, however, DAWN is being hailed as a life-changing opportunity. The workers who control the robots remotely (known as “pilots”) all have disabilities that limit their ability to move around freely and travel outside their homes. Worldwide, an estimated 16 percent of the global population lives with a significant disability—and according to the World Health Organization, these disabilities give rise to other problems, such as exclusion from education, unemployment, and poverty.
These are all problems that Kentaro Yoshifuji, founder and CEO of Ory Laboratory, which supplies the robot servers at DAWN, is looking to correct. Yoshifuji, who was bedridden for several years in high school due to an undisclosed health problem, launched the company to help enable people who are house-bound or bedridden to more fully participate in society, as well as end the loneliness, isolation, and feelings of worthlessness that can sometimes go hand-in-hand with being disabled.
“It’s heartbreaking to think that [people with disabilities] feel they are a burden to society, or that they fear their families suffer by caring for them,” said Yoshifuji in an interview in 2020. “We are dedicating ourselves to providing workable, technology-based solutions. That is our purpose.”

Shota, Kuwahara, a DAWN employee with muscular dystrophy, agrees. "There are many difficulties in my daily life, but I believe my life has a purpose and is not being wasted," he says. "Being useful, able to help other people, even feeling needed by others, is so motivational."
A woman receives a mammogram, which can detect the presence of tumors in a patient's breast.
When a patient is diagnosed with early-stage breast cancer, having surgery to remove the tumor is considered the standard of care. But what happens when a patient can’t have surgery?
Whether it’s due to high blood pressure, advanced age, heart issues, or other reasons, some breast cancer patients don’t qualify for a lumpectomy—one of the most common treatment options for early-stage breast cancer. A lumpectomy surgically removes the tumor while keeping the patient’s breast intact, while a mastectomy removes the entire breast and nearby lymph nodes.
Fortunately, a new technique called cryoablation is now available for breast cancer patients who either aren’t candidates for surgery or don’t feel comfortable undergoing a surgical procedure. With cryoablation, doctors use an ultrasound or CT scan to locate any tumors inside the patient’s breast. They then insert small, needle-like probes into the patient's breast which create an “ice ball” that surrounds the tumor and kills the cancer cells.
Cryoablation has been used for decades to treat cancers of the kidneys and liver—but only in the past few years have doctors been able to use the procedure to treat breast cancer patients. And while clinical trials have shown that cryoablation works for tumors smaller than 1.5 centimeters, a recent clinical trial at Memorial Sloan Kettering Cancer Center in New York has shown that it can work for larger tumors, too.
In this study, doctors performed cryoablation on patients whose tumors were, on average, 2.5 centimeters. The cryoablation procedure lasted for about 30 minutes, and patients were able to go home on the same day following treatment. Doctors then followed up with the patients after 16 months. In the follow-up, doctors found the recurrence rate for tumors after using cryoablation was only 10 percent.
For patients who don’t qualify for surgery, radiation and hormonal therapy is typically used to treat tumors. However, said Yolanda Brice, M.D., an interventional radiologist at Memorial Sloan Kettering Cancer Center, “when treated with only radiation and hormonal therapy, the tumors will eventually return.” Cryotherapy, Brice said, could be a more effective way to treat cancer for patients who can’t have surgery.
“The fact that we only saw a 10 percent recurrence rate in our study is incredibly promising,” she said.

