We Should Resist Making “Synthetic Embryos” Too Realistic

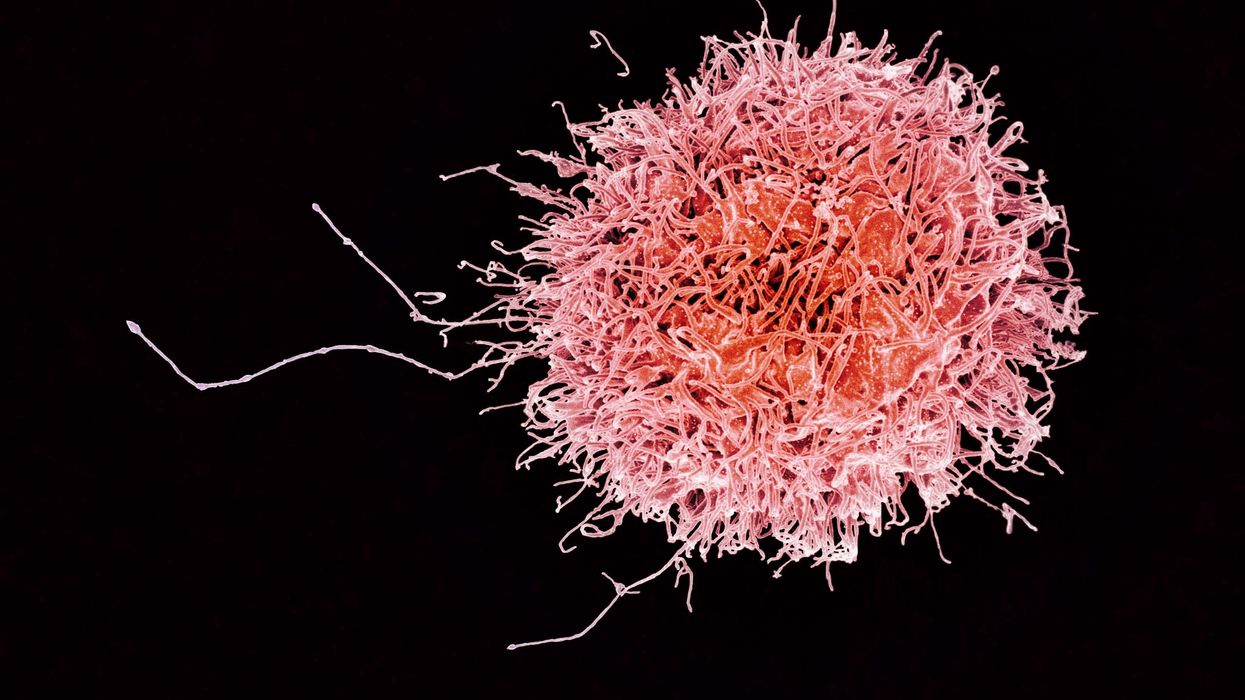
A rendering of emerging medical technology.
Ethics needs context. So does science – specifically, science that aims to create bioengineered models of early human embryo development in a dish (hereafter synthetic embryos). Even the term "synthetic embryos" begs for an explanation. What are these? And why would anyone want to create them?
"This knowledge may help scientists understand how certain birth defects are formed and why miscarriages often occur."
First the research context. Synthetic embryos are stem cell-derived simulations of human post-implantation embryos that are designed to mimic a stage of early development called gastrulation. That's the stage—around 14-15 days after fertilization – when embryos begin to form a very primitive body plan (basic dorsal-ventral and anterior-posterior axes, and distinct cell lineages). Researchers are starting to create synthetic embryos in the lab – albeit imperfect and incomplete versions – to learn how gastrulation might unfold in real human embryos embedded unseen in the womb. This knowledge may help scientists understand how certain birth defects are formed and why miscarriages often occur soon after implantation. As such, synthetic embryos are meant to be models of human embryo development, not themselves actually embryos. But will synthetic embryos ever get to the point where they are practically the same thing as "natural" human embryos? That is my concern and why I think researchers should avoid creating synthetic embryos capable of doing everything natural embryos can do.
It may not be too difficult to prevent this slide from synthetic to real. Synthetic embryos must be created using sophisticated 3D culture systems that mimic the complex architecture of human embryos. These complex culture systems also have to incorporate precise microinjection systems to chemically trigger the symmetry-breaking events involved in early body plan formation. In short, synthetic embryos need a heavy dose of engineering to get their biological processes going and to help keep them going. And like most engineered entities, designs can be built into the system early to serve well-considered goals – in our case, the goal of not wanting to create synthetic embryos that are too realistic.
"If one wants to study how car engines work, one can model an engine without also modeling the wheels, transmission, and every other car part together."
A good example of this point is found a report published in Nature Communications where scientists created a human stem cell-based 3D model that faithfully recapitulates the biological events around post-implantation amniotic sac development. Importantly, however, the embryo model they developed lacked several key structures and therefore – despite its partial resemblance to an early human embryo – did not have complete human form and potential. While fulfilling their model's aim of revealing a previously inaccessible early developmental event, the team intentionally did not recreate the entire post-implantation human embryo because they did not want to provoke any ethical concerns, as the lead author told me personally. Besides, creating a complete synthetic embryo was not necessary or scientifically justified for the research question they were pursuing. This example goes to show that researchers can create a synthetic embryo to model specific developmental events they want to study without modeling every aspect of a developing embryo. Likewise – to use a somewhat imprecise but instructive analogy – if one wants to study how car engines work, one can model an engine without also modeling the wheels, transmission, and every other car part together.

A representative "synthetic embryo," which in some ways resembles a post-implantation embryo around 14 days after fertilization.
(Courtesy of Yue Shao)
But why should researchers resist creating complete synthetic embryos? To answer this, we need some policy context. Currently there is an embryo research rule in place – a law in many nations, in others a culturally accepted agreement – that intact human embryos must not be grown for research in the lab for longer than 14 consecutive days after fertilization or the formation of the primitive streak (a faint embryonic band that signals the start of gastrulation). This is commonly referred to as the 14-day rule. It was established in the UK decades ago to carve out a space for meritorious human embryo research while simultaneously assuring the public that researchers won't go too far in cultivating embryos to later developmental stages before destroying them at the end of their studies. Many citizens accepting of pre-implantation stage human embryo research would not have tolerated post-implantation stage embryo use. The 14-day rule was a line in the sand, drawn to protect the advancement of embryo research, which otherwise might have been stifled without this clear stopping point. To date, the 14-day rule has not been revoked anywhere in the world, although new research in extended natural embryo cultivation is starting to put some pressure on it.
"Perhaps the day will come when scientists don't have to apply for research funding under such a dark cloud of anti-science sentiment."
Why does this policy context matter? The creation of complete synthetic embryos could raise serious questions (some of them legal) about whether the 14-day rule applies to these lab entities. Although they can be constructed in far fewer than 14 days, they would, at least in theory, be capable of recapitulating all of a natural embryo's developmental events at the gastrulation stage, thus possibly violating the spirit of the 14-day rule. Embryo research laws and policies worldwide are not ready yet to tackle this issue. Furthermore, professional guidelines issued by the International Society for Stem Cell Research prohibit the culture of any "organized embryo-like cellular structures with human organismal potential" to be cultured past the formation of the primitive streak. Thus, researchers should wait until there is greater clarity on this point, or until the 14-day rule is revised through proper policy-making channels to explicitly exclude complete synthetic embryos from its reach.
I should be clear that I am not basing my recommendations on any anti-embryo-research position per se, or on any metaphysical position regarding the positive moral status of synthetic embryos. Rather, I am concerned about the potential backlash that research on complete synthetic embryos might bring to embryo research in general. I began this essay by saying that ethics needs context. The ethics of synthetic embryo research needs to be considered within the context of today's fraught political environment. Perhaps the day will come when scientists don't have to apply for research funding under such a dark cloud of anti-science sentiment. Until then, however, it is my hope that scientists can fulfill their research aims by working on an array of different but each purposefully incomplete synthetic embryo models to generate, in the aggregate of their published work, a unified portrait of human development such that biologically complete synthetic embryo models will not be necessary.
Editor's Note: Read a different viewpoint here written by a leading New York fertility doctor/researcher.
Dr. May Edward Chinn, Kizzmekia Corbett, PhD., and Alice Ball, among others, have been behind some of the most important scientific work of the last century.
If you look back on the last century of scientific achievements, you might notice that most of the scientists we celebrate are overwhelmingly white, while scientists of color take a backseat. Since the Nobel Prize was introduced in 1901, for example, no black scientists have landed this prestigious award.
The work of black women scientists has gone unrecognized in particular. Their work uncredited and often stolen, black women have nevertheless contributed to some of the most important advancements of the last 100 years, from the polio vaccine to GPS.
Here are five black women who have changed science forever.
Dr. May Edward Chinn
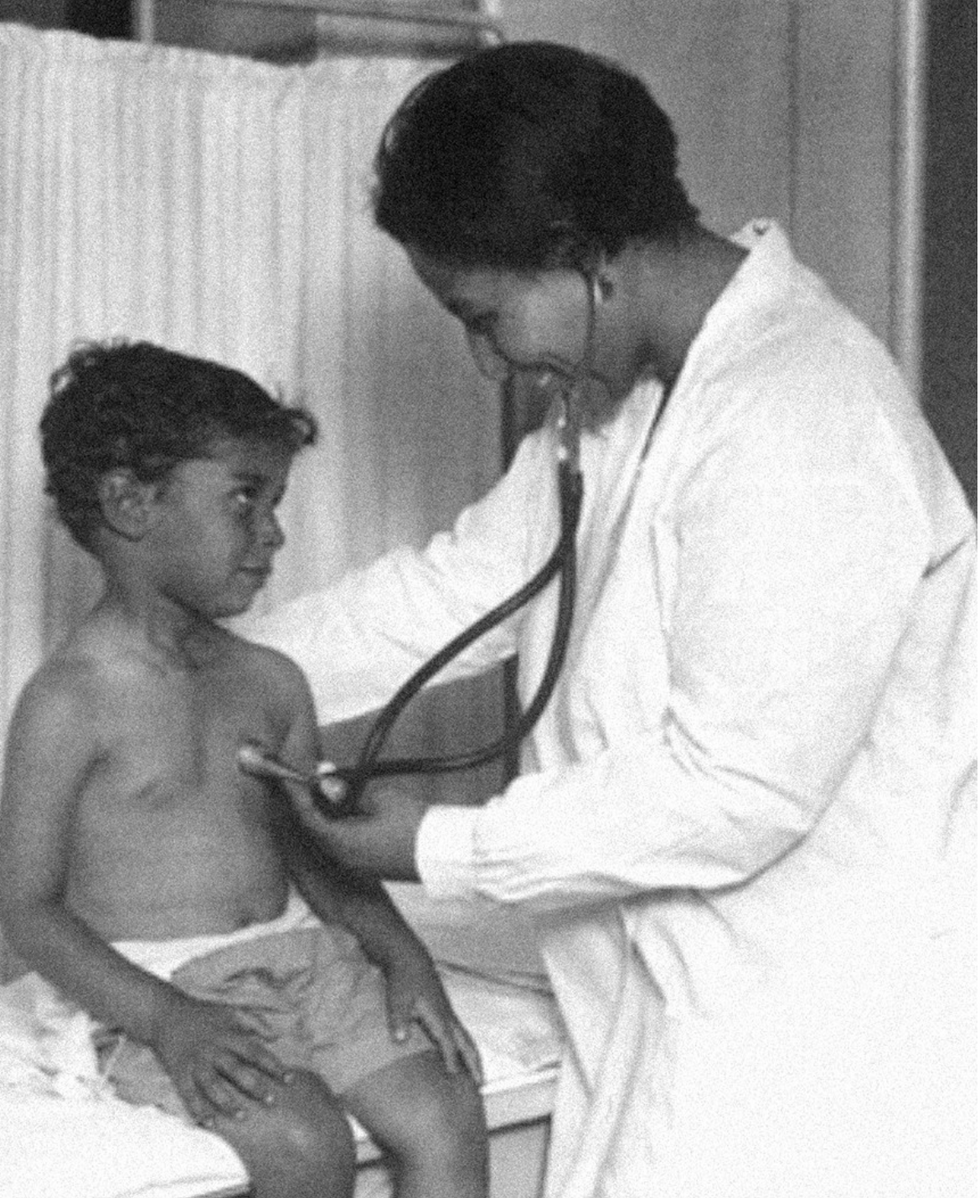
Dr. May Edward Chinn practicing medicine in Harlem
George B. Davis, PhD.
Chinn was born to poor parents in New York City just before the start of the 20th century. Although she showed great promise as a pianist, playing with the legendary musician Paul Robeson throughout the 1920s, she decided to study medicine instead. Chinn, like other black doctors of the time, were barred from studying or practicing in New York hospitals. So Chinn formed a private practice and made house calls, sometimes operating in patients’ living rooms, using an ironing board as a makeshift operating table.
Chinn worked among the city’s poor, and in doing this, started to notice her patients had late-stage cancers that often had gone undetected or untreated for years. To learn more about cancer and its prevention, Chinn begged information off white doctors who were willing to share with her, and even accompanied her patients to other clinic appointments in the city, claiming to be the family physician. Chinn took this information and integrated it into her own practice, creating guidelines for early cancer detection that were revolutionary at the time—for instance, checking patient health histories, checking family histories, performing routine pap smears, and screening patients for cancer even before they showed symptoms. For years, Chinn was the only black female doctor working in Harlem, and she continued to work closely with the poor and advocate for early cancer screenings until she retired at age 81.
Alice Ball

Pictorial Press Ltd/Alamy
Alice Ball was a chemist best known for her groundbreaking work on the development of the “Ball Method,” the first successful treatment for those suffering from leprosy during the early 20th century.
In 1916, while she was an undergraduate student at the University of Hawaii, Ball studied the effects of Chaulmoogra oil in treating leprosy. This oil was a well-established therapy in Asian countries, but it had such a foul taste and led to such unpleasant side effects that many patients refused to take it.
So Ball developed a method to isolate and extract the active compounds from Chaulmoogra oil to create an injectable medicine. This marked a significant breakthrough in leprosy treatment and became the standard of care for several decades afterward.
Unfortunately, Ball died before she could publish her results, and credit for this discovery was given to another scientist. One of her colleagues, however, was able to properly credit her in a publication in 1922.
Henrietta Lacks

onathan Newton/The Washington Post/Getty
The person who arguably contributed the most to scientific research in the last century, surprisingly, wasn’t even a scientist. Henrietta Lacks was a tobacco farmer and mother of five children who lived in Maryland during the 1940s. In 1951, Lacks visited Johns Hopkins Hospital where doctors found a cancerous tumor on her cervix. Before treating the tumor, the doctor who examined Lacks clipped two small samples of tissue from Lacks’ cervix without her knowledge or consent—something unthinkable today thanks to informed consent practices, but commonplace back then.
As Lacks underwent treatment for her cancer, her tissue samples made their way to the desk of George Otto Gey, a cancer researcher at Johns Hopkins. He noticed that unlike the other cell cultures that came into his lab, Lacks’ cells grew and multiplied instead of dying out. Lacks’ cells were “immortal,” meaning that because of a genetic defect, they were able to reproduce indefinitely as long as certain conditions were kept stable inside the lab.
Gey started shipping Lacks’ cells to other researchers across the globe, and scientists were thrilled to have an unlimited amount of sturdy human cells with which to experiment. Long after Lacks died of cervical cancer in 1951, her cells continued to multiply and scientists continued to use them to develop cancer treatments, to learn more about HIV/AIDS, to pioneer fertility treatments like in vitro fertilization, and to develop the polio vaccine. To this day, Lacks’ cells have saved an estimated 10 million lives, and her family is beginning to get the compensation and recognition that Henrietta deserved.
Dr. Gladys West

Andre West
Gladys West was a mathematician who helped invent something nearly everyone uses today. West started her career in the 1950s at the Naval Surface Warfare Center Dahlgren Division in Virginia, and took data from satellites to create a mathematical model of the Earth’s shape and gravitational field. This important work would lay the groundwork for the technology that would later become the Global Positioning System, or GPS. West’s work was not widely recognized until she was honored by the US Air Force in 2018.
Dr. Kizzmekia "Kizzy" Corbett

TIME Magazine
At just 35 years old, immunologist Kizzmekia “Kizzy” Corbett has already made history. A viral immunologist by training, Corbett studied coronaviruses at the National Institutes of Health (NIH) and researched possible vaccines for coronaviruses such as SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome).
At the start of the COVID pandemic, Corbett and her team at the NIH partnered with pharmaceutical giant Moderna to develop an mRNA-based vaccine against the virus. Corbett’s previous work with mRNA and coronaviruses was vital in developing the vaccine, which became one of the first to be authorized for emergency use in the United States. The vaccine, along with others, is responsible for saving an estimated 14 million lives.On today’s episode of Making Sense of Science, I’m honored to be joined by Dr. Paul Song, a physician, oncologist, progressive activist and biotech chief medical officer. Through his company, NKGen Biotech, Dr. Song is leveraging the power of patients’ own immune systems by supercharging the body’s natural killer cells to make new treatments for Alzheimer’s and cancer.
Whereas other treatments for Alzheimer’s focus directly on reducing the build-up of proteins in the brain such as amyloid and tau in patients will mild cognitive impairment, NKGen is seeking to help patients that much of the rest of the medical community has written off as hopeless cases, those with late stage Alzheimer’s. And in small studies, NKGen has shown remarkable results, even improvement in the symptoms of people with these very progressed forms of Alzheimer’s, above and beyond slowing down the disease.
In the realm of cancer, Dr. Song is similarly setting his sights on another group of patients for whom treatment options are few and far between: people with solid tumors. Whereas some gradual progress has been made in treating blood cancers such as certain leukemias in past few decades, solid tumors have been even more of a challenge. But Dr. Song’s approach of using natural killer cells to treat solid tumors is promising. You may have heard of CAR-T, which uses genetic engineering to introduce cells into the body that have a particular function to help treat a disease. NKGen focuses on other means to enhance the 40 plus receptors of natural killer cells, making them more receptive and sensitive to picking out cancer cells.
Paul Y. Song, MD is currently CEO and Vice Chairman of NKGen Biotech. Dr. Song’s last clinical role was Asst. Professor at the Samuel Oschin Cancer Center at Cedars Sinai Medical Center.
Dr. Song served as the very first visiting fellow on healthcare policy in the California Department of Insurance in 2013. He is currently on the advisory board of the Pritzker School of Molecular Engineering at the University of Chicago and a board member of Mercy Corps, The Center for Health and Democracy, and Gideon’s Promise.
Dr. Song graduated with honors from the University of Chicago and received his MD from George Washington University. He completed his residency in radiation oncology at the University of Chicago where he served as Chief Resident and did a brachytherapy fellowship at the Institute Gustave Roussy in Villejuif, France. He was also awarded an ASTRO research fellowship in 1995 for his research in radiation inducible gene therapy.
With Dr. Song’s leadership, NKGen Biotech’s work on natural killer cells represents cutting-edge science leading to key findings and important pieces of the puzzle for treating two of humanity’s most intractable diseases.
Show links
- Paul Song LinkedIn
- NKGen Biotech on Twitter - @NKGenBiotech
- NKGen Website: https://nkgenbiotech.com/
- NKGen appoints Paul Song
- Patient Story: https://pix11.com/news/local-news/long-island/promising-new-treatment-for-advanced-alzheimers-patients/
- FDA Clearance: https://nkgenbiotech.com/nkgen-biotech-receives-ind-clearance-from-fda-for-snk02-allogeneic-natural-killer-cell-therapy-for-solid-tumors/Q3 earnings data: https://www.nasdaq.com/press-release/nkgen-biotech-inc.-reports-third-quarter-2023-financial-results-and-business