Paralyzed By Polio, This British Tea Broker Changed the Course Of Medical History Forever
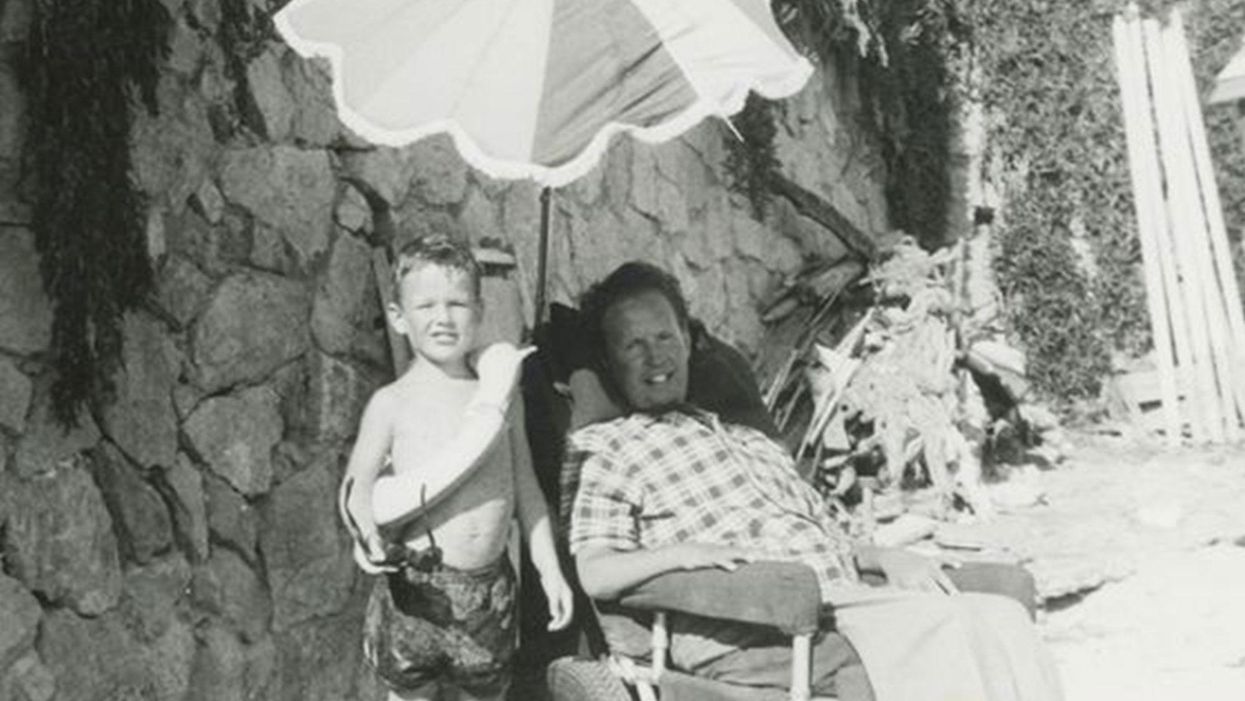
Robin Cavendish in his special wheelchair with his son Jonathan in the 1960s.
In December 1958, on a vacation with his wife in Kenya, a 28-year-old British tea broker named Robin Cavendish became suddenly ill. Neither he nor his wife Diana knew it at the time, but Robin's illness would change the course of medical history forever.
Robin was rushed to a nearby hospital in Kenya where the medical staff delivered the crushing news: Robin had contracted polio, and the paralysis creeping up his body was almost certainly permanent. The doctors placed Robin on a ventilator through a tracheotomy in his neck, as the paralysis from his polio infection had rendered him unable to breathe on his own – and going off the average life expectancy at the time, they gave him only three months to live. Robin and Diana (who was pregnant at the time with their first child, Jonathan) flew back to England so he could be admitted to a hospital. They mentally prepared to wait out Robin's final days.
But Robin did something unexpected when he returned to the UK – just one of many things that would astonish doctors over the next several years: He survived. Diana gave birth to Jonathan in February 1959 and continued to visit Robin regularly in the hospital with the baby. Despite doctors warning that he would soon succumb to his illness, Robin kept living.
After a year in the hospital, Diana suggested something radical: She wanted Robin to leave the hospital and live at home in South Oxfordshire for as long as he possibly could, with her as his nurse. At the time, this suggestion was unheard of. People like Robin who depended on machinery to keep them breathing had only ever lived inside hospital walls, as the prevailing belief was that the machinery needed to keep them alive was too complicated for laypeople to operate. But Diana and Robin were up for the challenges – and the risks. Because his ventilator ran on electricity, if the house were to unexpectedly lose power, Diana would either need to restore power quickly or hand-pump air into his lungs to keep him alive.
Robin's wheelchair was not only the first of its kind; it became the model for the respiratory wheelchairs that people still use today.
In an interview as an adult, Jonathan Cavendish reflected on his parents' decision to live outside the hospital on a ventilator: "My father's mantra was quality of life," he explained. "He could have stayed in the hospital, but he didn't think that was as good of a life as he could manage. He would rather be two minutes away from death and living a full life."
After a few years of living at home, however, Robin became tired of being confined to his bed. He longed to sit outside, to visit friends, to travel – but had no way of doing so without his ventilator. So together with his friend Teddy Hall, a professor and engineer at Oxford University, the two collaborated in 1962 to create an entirely new invention: a battery-operated wheelchair prototype with a ventilator built in. With this, Robin could now venture outside the house – and soon the Cavendish family became famous for taking vacations. It was something that, by all accounts, had never been done before by someone who was ventilator-dependent. Robin and Hall also designed a van so that the wheelchair could be plugged in and powered during travel. Jonathan Cavendish later recalled a particular family vacation that nearly ended in disaster when the van broke down outside of Barcelona, Spain:
"My poor old uncle [plugged] my father's chair into the wrong socket," Cavendish later recalled, causing the electricity to short. "There was fire and smoke, and both the van and the chair ground to a halt." Johnathan, who was eight or nine at the time, his mother, and his uncle took turns hand-pumping Robin's ventilator by the roadside for the next thirty-six hours, waiting for Professor Hall to arrive in town and repair the van. Rather than being panicked, the Cavendishes managed to turn the vigil into a party. Townspeople came to greet them, bringing food and music, and a local priest even stopped by to give his blessing.
Robin had become a pioneer, showing the world that a person with severe disabilities could still have mobility, access, and a fuller quality of life than anyone had imagined. His mission, along with Hall's, then became gifting this independence to others like himself. Robin and Hall raised money – first from the Ernest Kleinwort Charitable Trust, and then from the British Department of Health – to fund more ventilator chairs, which were then manufactured by Hall's company, Littlemore Scientific Engineering, and given to fellow patients who wanted to live full lives at home. Robin and Hall used themselves as guinea pigs, testing out different models of the chairs and collaborating with scientists to create other devices for those with disabilities. One invention, called the Possum, allowed paraplegics to control things like the telephone and television set with just a nod of the head. Robin's wheelchair was not only the first of its kind; it became the model for the respiratory wheelchairs that people still use today.
Robin went on to enjoy a long and happy life with his family at their house in South Oxfordshire, surrounded by friends who would later attest to his "down-to-earth" personality, his sense of humor, and his "irresistible" charm. When he died peacefully at his home in 1994 at age 64, he was considered the world's oldest-living person who used a ventilator outside the hospital – breaking yet another barrier for what medical science thought was possible.
Frequent, thorough handwashing is essential to protecting yourself from infection.
What's the case-fatality rate?
Currently, the official rate is 3.4%. But this is likely way too high. China was hit particularly hard, and their healthcare system was overwhelmed. The best data we have is from South Korea. The Koreans tested 210,000 people and detected the virus in 7,478 patients. So far, the death toll is 53, which is a case-fatality rate of 0.7%. This is seven times worse than the seasonal flu (which has a case-fatality rate of 0.1%).
What's the best way to clean your hands? Soap and water? Hand sanitizer?
Soap and water is always best. Be sure to wash your hands thoroughly. (The CDC recommends 20 seconds.) If soap and water are not available, the CDC says to use hand sanitizer that is at least 60% alcohol. The problem with hand sanitizer, however, is that people neither use enough nor spread it over their hands properly. Also, the sanitizer should be covering your hands for 10-15 seconds, not evaporating before that.
How often should I wash my hands?
You should wash your hands after being in a public place, before you eat, and before you touch your face. It's a good idea to wash your hands after handling money and your cell phone, too.
How long can coronavirus live on surfaces?
It depends on the surface. According to the New York Times, "[C]old and flu viruses survive longer on inanimate surfaces that are nonporous, like metal, plastic and wood, and less on porous surfaces, like clothing, paper and tissue." According to the Journal of Hospital Infection, human coronaviruses "can persist on inanimate surfaces like metal, glass or plastic for up to 9 days, but can be efficiently inactivated by surface disinfection procedures with 62–71% ethanol, 0.5% hydrogen peroxide or 0.1% sodium hypochlorite within 1 minute." (Note: Sodium hypochlorite is bleach.)
Can Lysol wipes kill it?
Maybe not. It depends on the active ingredient. Many Lysol products use benzalkonium chloride, which the aforementioned Journal of Hospital Infection paper said was "less effective." The EPA has released a list of disinfectants recommended for use against coronavirus.
Should you wear a mask in public?
The CDC does not recommend that healthy people wear a mask in public. The benefit is likely small. However, if you are sick, then you should wear a mask to help catch respiratory droplets as you exhale.
Will pets give it to you?
That can't be ruled out. There is a documented case of human-to-canine transmission. However, an article in LiveScience explains that canine-to-human is unlikely.
Are there any "normal" things we are doing that make things worse?
Yes! Not washing your hands!!
What does it mean that previously cleared people are getting sick again? Is it the virus within or have they caught it via contamination?
It's not entirely clear. It could be that the virus was never cleared to begin with. Or it could be that the person was simply infected again. That could happen if the antibodies generated don't last long.
Will the virus go away with the weather/summer?
Quite likely, yes. Cold and flu viruses don't do well outside in summer weather. (For influenza, the warm weather causes the viral envelope to become a liquid, and it can no longer protect the virus.) That's why cold and flu season is always during the late fall and winter. However, some experts think that it is a "false hope" that the coronavirus will disappear during the summer. We'll have to wait and see.
And will it come back in the fall/winter?
That's a likely outcome. Again, we'll have to wait and see. Some epidemiologists think that COVID-19 will become seasonal like influenza.
Does dry or humid air make a difference?
Flu viruses prefer cold, dry weather. That could be true of coronaviruses, too.
What is the incubation period?
According to the World Health Organization, it's about 5 days. But it could be anywhere from 1 to 14 days.
Should you worry about sitting next to asymptomatic people on a plane or train?
It's not possible to tell if an asymptomatic person is infected or not. That's what makes asymptomatic people tricky. Just be cautious. If you're worried, treat everyone like they might be infected. Don't let them get too close or cough in your face. Be sure to wash your hands.
Should you cancel air travel planned in the next 1-2 months in the U.S.?
There are no hard and fast rules. Use common sense. Avoid hotspots of infection. If you have a trip planned to Wuhan, you might want to wait on that one. If you have a trip planned to Seattle and you're over the age of 60 and/or have an underlying health condition, you may want to hold off on that, too. If you do fly on a plane, former FDA commissioner Dr. Scott Gottlieb recommends cleaning the back of your seat and other close contact areas with antiseptic wipes. He also refuses to take anything handed out by flight attendants, since he says the biggest route of transmission comes from touching contaminated surfaces (and then touching your face).
There have been reports of an escalation of hate crimes towards Asian Americans. Can the microbiologist help illuminate that this disease has impacted all racial groups?
People might be racist, but COVID-19 is not. It can infect anyone. Older people (i.e., 60 years and older) and those with underlying health conditions are most at risk. Interestingly, young people (aged 9 and under) are minimally impacted.
To what extent/if any should toddlers -- who put everything in mouth -- avoid group classes like Gymboree?
If they get infected, toddlers will probably experience only a mild illness. The problem is if the toddler then infects somebody at higher risk, like grandpa or grandma.
Should I avoid events like concerts or theater performances if I live in a place where there is known coronavirus?
It's not an unreasonable thing to do.
Any special advice or concerns for pregnant women?
There isn't good data on this. Previous evidence, reported by the CDC, suggests that pregnant women may be more susceptible to respiratory viruses.
Advice for residents of long-term care facilities/nursing homes?
Remind the nurse or aide to constantly wash their hands.
Can we eat at Chinese restaurants? Does eating onions kill viruses? Can I take an Uber and be safe from infection?
Yes. No. Does the Uber driver or previous passengers have coronavirus? It's not possible to tell. So, treat an Uber like a public space and behave accordingly.
What public spaces should we avoid?
That's hard to say. Some people avoid large gatherings, others avoid leaving the house. Ultimately, it's going to depend on who you are and what sort of risk you're willing to take. (For example, are you young and healthy or old and sick?) I would be willing to do things that I would advise older people avoid, like going to a sporting event.
What are the differences between the L strain and the S strain?
That's not entirely clear, and it's not even clear that they are separate strains. There are some genetic differences between them. However, just because RNA viruses mutate doesn't necessarily mean that the virus will mutate to something more dangerous or unrecognizable by our immune system. The measles virus mutates, but it more or less remains the same, which is why a single vaccine could eradicate it – if enough people actually were willing to get a measles shot.
Should I wear disposable gloves while traveling?
No. If you touch something that's contaminated, the virus will be on your glove instead of your hand. If you then touch your face, you still might get sick.
The Best Coronavirus Experts to Follow on Twitter
Following these experts on social media will help you stay well-informed about the coronavirus. Global virus and disease spread, coronavirus.
As the coronavirus tears across the globe, the world's anxiety is at a fever-pitch, and we're all craving information to stay on top of the crisis.
But turning to the Internet for credible updates isn't as simple as it sounds, since we have an invisible foe spreading as quickly as the virus itself: misinformation. From wild conspiracy theories to baseless rumors, an infodemic is in full swing.
For the latest official information, you should follow the CDC, WHO, and FDA, in addition to your local public health department. But it's also helpful to pay attention to the scientists, doctors, public health experts and journalists who are sharing their perspectives in real time as new developments unfold. Here's a handy guide to get you started:
VIROLOGY
Dr. Trevor Bedford/@trvrb: Scientist at the Fred Hutchinson Cancer Research Center studying viruses, evolution and immunity.
Dr. Benhur Lee/@VirusWhisperer: Professor of microbiology at the Icahn School of Medicine at Mount Sinai
Dr. Angela Rasmussen/@angie_rasmussen: Virologist and associate research scientist at Columbia University
Dr. Florian Krammer/@florian_krammer: Professor of Microbiology at the Icahn School of Medicine at Mount Sinai
EPIDEMIOLOGY:
Dr. Alice Sim/@alicesim: Infectious disease epidemiologist and consultant at the World Health Organization
Dr. Tara C. Smith/@aetiology: Infectious disease specialist and professor at Kent State University
Dr. Caitlin Rivers/@cmyeaton: Epidemiologist and assistant professor at the Johns Hopkins Bloomberg School of Public Health
Dr. Michael Mina/@michaelmina_lab: Physician and Assistant Professor of Epidemiology & Immunology at the Harvard TH Chan School of Public Health
INFECTIOUS DISEASE:
Dr. Nahid Bhadelia/@BhadeliaMD: Infectious diseases physician and the medical director of Special Pathogens Unit at Boston University School of Medicine
Dr. Paul Sax/@PaulSaxMD: Clinical Director of the Division of Infectious Diseases at Brigham and Women's Hospital
Dr. Priya Sampathkumar/@PsampathkumarMD: Infectious Disease Specialist at the Mayo Clinic
Dr. Krutika Kuppalli/@KrutikaKuppalli: Medical doctor and Infectious Disease Specialist based in Palo Alto, CA
PANDEMIC PREP:
Dr. Syra Madad/@syramadad: Senior Director, System-wide Special Pathogens Program at New York City Health + Hospitals
Dr Sylvie Briand/@SCBriand: Director of Pandemic and Epidemic Diseases Department at the World Health Organization
Jeremy Konyndyk/@JeremyKonyndyk: Senior Policy Fellow at the Center for Global Development
Amesh Adalja/@AmeshAA: Senior Scholar at the Johns Hopkins University Center for Health Security
PUBLIC HEALTH:
Scott Becker/@scottjbecker: CEO of the Association of Public Health Laboratories
Dr. Scott Gottlieb/@ScottGottliebMD: Physician, former commissioner of the Food and Drug Administration
APHA Public Health Nursing/@APHAPHN: Public Health Nursing Section of the American Public Health Association
Dr. Tom Inglesby/@T_Inglesby: Director of the Johns Hopkins SPH Center for Health Security
Dr. Nancy Messonnier/@DrNancyM_CDC: Director of the Center for the National Center for Immunization and Respiratory Diseases (NCIRD)
Dr. Arthur Caplan/@ArthurCaplan: Professor of Bioethics at New York University Langone Medical Center
SCIENCE JOURNALISTS:
Laura Helmuth/@laurahelmuth: Incoming Editor in Chief of Scientific American
Helen Branswell/@HelenBranswell: Infectious disease and public health reporter at STAT
Sharon Begley/@sxbegle: Senior writer at STAT
Carolyn Johnson/@carolynyjohnson: Science reporter at the Washington Post
Amy Maxmen/@amymaxmen: Science writer and senior reporter at Nature
Laurie Garrett/@Laurie_Garrett: Pulitzer-prize winning science journalist, author of The Coming Plague, former senior fellow for global health at the Council on Foreign Relations
Soumya Karlamangla/@skarlamangla: Health writer at the Los Angeles Times
André Picard/@picardonhealth: Health Columnist, The Globe and Mail
Caroline Chen/@CarolineYLChen: Healthcare reporter at ProPublica
Andrew Jacobs/@AndrewJacobsNYT: Science reporter at the New York Times
Meg Tirrell/@megtirrell: Biotech and pharma reporter for CNBC
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

