Paralyzed By Polio, This British Tea Broker Changed the Course Of Medical History Forever

Robin Cavendish in his special wheelchair with his son Jonathan in the 1960s.
In December 1958, on a vacation with his wife in Kenya, a 28-year-old British tea broker named Robin Cavendish became suddenly ill. Neither he nor his wife Diana knew it at the time, but Robin's illness would change the course of medical history forever.
Robin was rushed to a nearby hospital in Kenya where the medical staff delivered the crushing news: Robin had contracted polio, and the paralysis creeping up his body was almost certainly permanent. The doctors placed Robin on a ventilator through a tracheotomy in his neck, as the paralysis from his polio infection had rendered him unable to breathe on his own – and going off the average life expectancy at the time, they gave him only three months to live. Robin and Diana (who was pregnant at the time with their first child, Jonathan) flew back to England so he could be admitted to a hospital. They mentally prepared to wait out Robin's final days.
But Robin did something unexpected when he returned to the UK – just one of many things that would astonish doctors over the next several years: He survived. Diana gave birth to Jonathan in February 1959 and continued to visit Robin regularly in the hospital with the baby. Despite doctors warning that he would soon succumb to his illness, Robin kept living.
After a year in the hospital, Diana suggested something radical: She wanted Robin to leave the hospital and live at home in South Oxfordshire for as long as he possibly could, with her as his nurse. At the time, this suggestion was unheard of. People like Robin who depended on machinery to keep them breathing had only ever lived inside hospital walls, as the prevailing belief was that the machinery needed to keep them alive was too complicated for laypeople to operate. But Diana and Robin were up for the challenges – and the risks. Because his ventilator ran on electricity, if the house were to unexpectedly lose power, Diana would either need to restore power quickly or hand-pump air into his lungs to keep him alive.
Robin's wheelchair was not only the first of its kind; it became the model for the respiratory wheelchairs that people still use today.
In an interview as an adult, Jonathan Cavendish reflected on his parents' decision to live outside the hospital on a ventilator: "My father's mantra was quality of life," he explained. "He could have stayed in the hospital, but he didn't think that was as good of a life as he could manage. He would rather be two minutes away from death and living a full life."
After a few years of living at home, however, Robin became tired of being confined to his bed. He longed to sit outside, to visit friends, to travel – but had no way of doing so without his ventilator. So together with his friend Teddy Hall, a professor and engineer at Oxford University, the two collaborated in 1962 to create an entirely new invention: a battery-operated wheelchair prototype with a ventilator built in. With this, Robin could now venture outside the house – and soon the Cavendish family became famous for taking vacations. It was something that, by all accounts, had never been done before by someone who was ventilator-dependent. Robin and Hall also designed a van so that the wheelchair could be plugged in and powered during travel. Jonathan Cavendish later recalled a particular family vacation that nearly ended in disaster when the van broke down outside of Barcelona, Spain:
"My poor old uncle [plugged] my father's chair into the wrong socket," Cavendish later recalled, causing the electricity to short. "There was fire and smoke, and both the van and the chair ground to a halt." Johnathan, who was eight or nine at the time, his mother, and his uncle took turns hand-pumping Robin's ventilator by the roadside for the next thirty-six hours, waiting for Professor Hall to arrive in town and repair the van. Rather than being panicked, the Cavendishes managed to turn the vigil into a party. Townspeople came to greet them, bringing food and music, and a local priest even stopped by to give his blessing.
Robin had become a pioneer, showing the world that a person with severe disabilities could still have mobility, access, and a fuller quality of life than anyone had imagined. His mission, along with Hall's, then became gifting this independence to others like himself. Robin and Hall raised money – first from the Ernest Kleinwort Charitable Trust, and then from the British Department of Health – to fund more ventilator chairs, which were then manufactured by Hall's company, Littlemore Scientific Engineering, and given to fellow patients who wanted to live full lives at home. Robin and Hall used themselves as guinea pigs, testing out different models of the chairs and collaborating with scientists to create other devices for those with disabilities. One invention, called the Possum, allowed paraplegics to control things like the telephone and television set with just a nod of the head. Robin's wheelchair was not only the first of its kind; it became the model for the respiratory wheelchairs that people still use today.
Robin went on to enjoy a long and happy life with his family at their house in South Oxfordshire, surrounded by friends who would later attest to his "down-to-earth" personality, his sense of humor, and his "irresistible" charm. When he died peacefully at his home in 1994 at age 64, he was considered the world's oldest-living person who used a ventilator outside the hospital – breaking yet another barrier for what medical science thought was possible.
Harvard Scientist’s Breakthrough Could Make Humans Resistant to All Viruses
DNA recoding has already made E. coli bacteria immune to 90 percent of viruses that can infect it.
[Ed. Note: We're thrilled to present the first episode in our new Moonshot series, which will explore four cutting-edge scientific developments that stand to fundamentally transform our world.]
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
In the future, a paper strip reminiscent of a pregnancy test could be used to quickly diagnose the flu and other infectious diseases.
Trying to get a handle on CRISPR news in 2019 can be daunting if you haven't been avidly reading up on it for the last five years.
CRISPR as a diagnostic tool would be a major game changer for medicine and agriculture.
On top of trying to grasp how the science works, and keeping track of its ever expanding applications, you may also have seen coverage of an ongoing legal battle about who owns the intellectual property behind the gene-editing technology CRISPR-Cas9. And then there's the infamous controversy surrounding a scientist who claimed to have used the tool to edit the genomes of two babies in China last year.
But gene editing is not the only application of CRISPR-based biotechnologies. In the future, it may also be used as a tool to diagnose infectious diseases, which could be a major game changer for medicine and agriculture.
How It Works
CRISPR is an acronym for a naturally occurring DNA sequence that normally protects microbes from viruses. It's been compared to a Swiss army knife that can recognize an invader's DNA and precisely destroy it. Repurposed for humans, CRISPR can be paired with a protein called Cas9 that can detect a person's own DNA sequence (usually a problematic one), cut it out, and replace it with a different sequence. Used this way, CRISPR-Cas9 has become a valuable gene-editing tool that is currently being tested to treat numerous genetic diseases, from cancer to blood disorders to blindness.
CRISPR can also be paired with other proteins, like Cas13, which target RNA, the single-stranded twin of DNA that viruses rely on to infect their hosts and cause disease. In a future clinical setting, CRISPR-Cas13 might be used to diagnose whether you have the flu by cutting a target RNA sequence from the virus. That spliced sequence could stick to a paper test strip, causing a band to show up, like on a pregnancy test strip. If the influenza virus and its RNA are not present, no band would show up.
To understand how close to reality this diagnostic scenario is right now, leapsmag chatted with CRISPR pioneer Dr. Feng Zhang, a molecular biologist at the Broad Institute of MIT and Harvard.
What do you think might be the first point of contact that a regular person or patient would have with a CRISPR diagnostic tool?
FZ: I think in the long run it will be great to see this for, say, at-home disease testing, for influenza and other sorts of important public health [concerns]. To be able to get a readout at home, people can potentially quarantine themselves rather than traveling to a hospital and then carrying the risk of spreading that disease to other people as they get to the clinic.
"You could conceivably get a readout during the same office visit, and then the doctor will be able to prescribe the right treatment right away."
Is this just something that people will use at home, or do you also foresee clinical labs at hospitals applying CRISPR-Cas13 to samples that come through?
FZ: I think we'll see applications in both settings, and I think there are advantages to both. One of the nice things about SHERLOCK [a playful acronym for CRISPR-Cas13's longer name, Specific High-sensitivity Enzymatic Reporter unLOCKing] is that it's rapid; you can get a readout fairly quickly. So, right now, what people do in hospitals is they will collect your sample and then they'll send it out to a clinical testing lab, so you wouldn't get a result back until many hours if not several days later. With SHERLOCK, you could conceivably get a readout during the same office visit, and then the doctor will be able to prescribe the right treatment right away.
I just want to clarify that when you say a doctor would take a sample, that's referring to urine, blood, or saliva, correct?
FZ: Right. Yeah, exactly.
Thinking more long term, are there any Holy Grail applications that you hope CRISPR reaches as a diagnostic tool?
FZ: I think in the developed world we'll hopefully see this being used for influenza testing, and many other viral and pathogen-based diseases—both at home and also in the hospital—but I think the even more exciting direction is that this could be used and deployed in parts of the developing world where there isn't a fancy laboratory with elaborate instrumentation. SHERLOCK is relatively inexpensive to develop, and you can turn it into a paper strip test.
Can you quantify what you mean by relatively inexpensive? What range of prices are we talking about here?
FZ: So without accounting for economies of scale, we estimate that it can cost less than a dollar per test. With economy of scale that cost can go even lower.
Is there value in developing what is actually quite an innovative tool in a way that visually doesn't seem innovative because it's reminiscent of a pregnancy test? And I don't mean that as an insult.
FZ: [Laughs] Ultimately, we want the technology to be as accessible as possible, and pregnancy test strips have such a convenient and easy-to-use form. I think modeling after something that people are already familiar with and just changing what's under the hood makes a lot of sense.
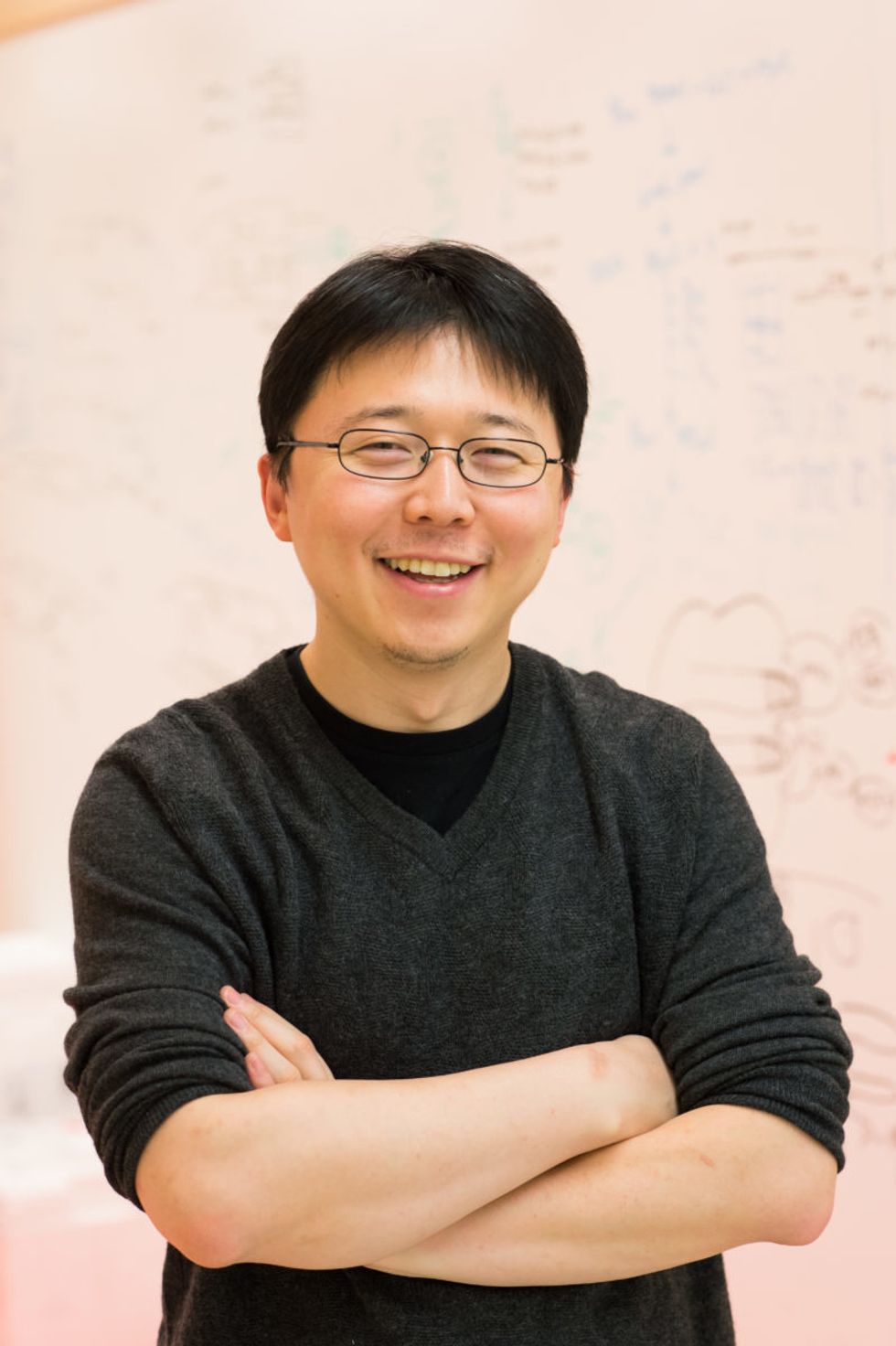
Feng Zhang
(Photo credit: Justin Knight, McGovern Institute)
It's probably one of the most accessible at-home diagnostic tools at this point that people are familiar with.
FZ: Yeah, so if people know how to use that, then using something that's very similar to it should make the option very easy.
You've been quite vocal in calling for some pauses in CRISPR-Cas9 research to make sure it doesn't outpace the ethics of establishing pregnancies with that version of the tool. Do you have any concerns about using CRISPR-Cas13 as a diagnostic tool?
I think overall, the reception for CRISPR-based diagnostics has been overwhelmingly positive. People are very excited about the prospect of using this—for human health and also in agriculture [for] detection of plant infections and plant pathogens, so that farmers will be able to react quickly to infection in the field. If we're looking at contamination of foods by certain bacteria, [food safety] would also be a really exciting application.
Do you feel like the controversies surrounding using CRISPR as a gene-editing tool have overshadowed its potential as a diagnostics tool?
FZ: I don't think so. I think the potential for using CRISPR-Cas9 or CRISPR-Cas12 for gene therapy, and treating disease, has captured people's imaginations, but at the same time, every time I talk with someone about the ability to use CRISPR-Cas13 as a diagnostic tool, people are equally excited. Especially when people see the very simple paper strip that we developed for detecting diseases.
Are CRISPR as a gene-editing tool and CRISPR as a diagnostics tool on different timelines, as far as when the general public might encounter them in their real lives?
FZ: I think they are all moving forward quite quickly. CRISPR as a gene-editing tool is already being deployed in human health and agriculture. We've already seen the approval for the development of growing genome-edited mushrooms, soybeans, and other crop species. So I think people will encounter those in their daily lives in that manner.
Then, of course, for disease treatment, that's progressing rapidly as well. For patients who are affected by sickle cell disease, and also by a degenerative eye disease, clinical trials are already starting in those two areas. Diagnostic tests are also developing quickly, and I think in the coming couple of years, we'll begin to see some of these reaching into the public realm.
"There are probably 7,000 genetic diseases identified today, and most of them don't have any way of being treated."
As far its limits, will it be hard to use CRISPR as a diagnostic tool in situations where we don't necessarily understand the biological underpinnings of a disease?
FZ: CRISPR-Cas13, as a diagnostic tool, at least in the current way that it's implemented, is a detection tool—it's not a discovery tool. So if we don't know what we're looking for, then it's going to be hard to develop Cas13 to detect it. But even in the case of a new infectious disease, if DNA sequencing or RNA sequencing information is available for that new virus, then we can very rapidly program a Cas13-based system to detect it, based on that sequence.
What's something you think the public misunderstands about CRISPR, either in general, or specifically as a diagnostic tool, that you wish were better understood?
FZ: That's a good question. CRISPR-Cas9 and CRISPR-Cas12 as gene editing tools, and also CRISPR-Cas13 as a diagnostic tool, are able to do some things, but there are still a lot of capabilities that need to be further developed. So I think the potential for the technology will unfold over the next decade or so, but it will take some time for the full impact of the technology to really get realized in real life.
What do you think that full impact is?
FZ: There are probably 7,000 genetic diseases identified today, and most of them don't have any way of being treated. It will take some time for CRISPR-Cas9 and Cas12 to be really developed for addressing a larger number of those diseases. And then for CRISPR-based diagnostics, I think you'll see the technology being applied in a couple of initial cases, and it will take some time to develop that more broadly for many other applications.