One of the World’s Most Famous Neuroscientists Wants You to Embrace Meditation and Spirituality
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
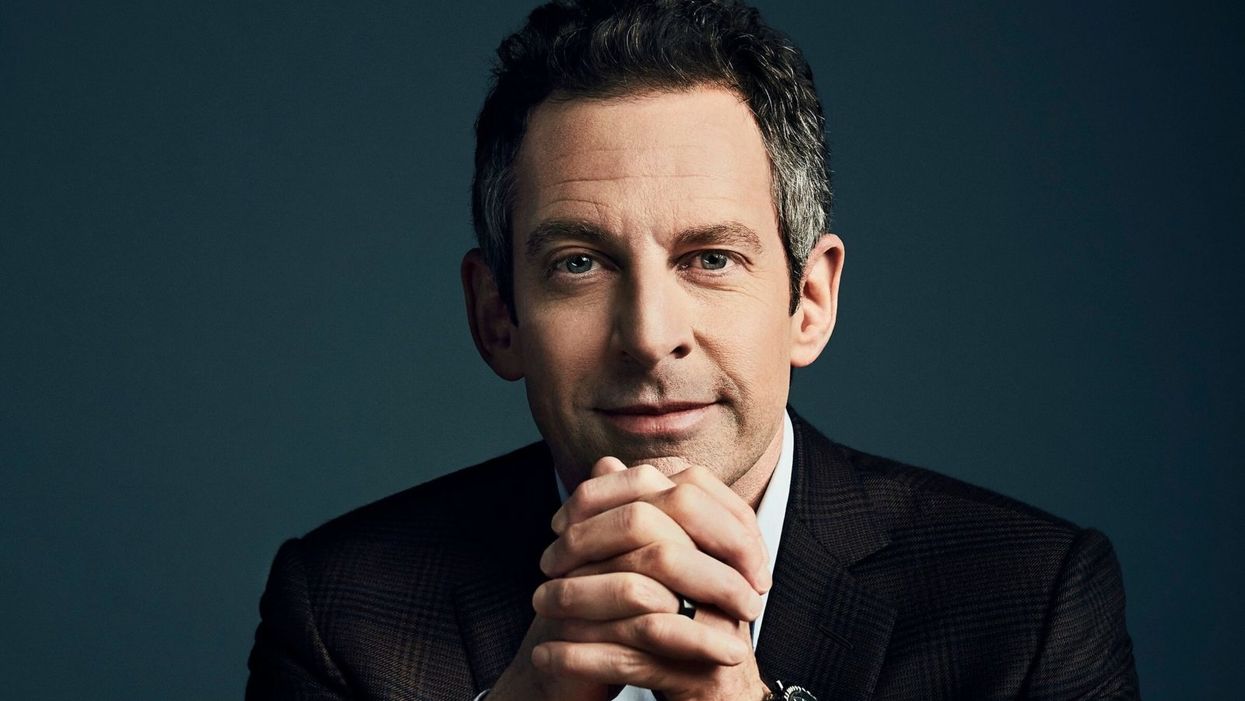
Sam Harris, the neuroscientist and bestselling author, discusses mindfulness meditation.
Neuroscientist, philosopher, and bestselling author Sam Harris is famous for many reasons, among them his vocal criticism of religion, his scientific approach to moral questions, and his willingness to tackle controversial topics on his popular podcast.
"Until you have some capacity to be mindful, you have no choice but to be lost in every next thought that arises."
He is also a passionate advocate of mindfulness meditation, having spent formative time as a young adult learning from teachers in India and Tibet before returning to the West.
Now his new app called Waking Up aims to teach the principles of meditation to anyone who is willing to slow down, turn away from everyday distractions, and pay attention to their own mind. Harris recently chatted with leapsmag about the science of mindfulness, the surprising way he discovered it, and the fundamental—but under-appreciated—reason to do it. This conversation has been lightly edited and condensed.
One of the biggest struggles that so many people face today is how to stay present in the moment. Is this the default state for human beings, or is this a more recent phenomenon brought on by our collective addiction to screens?
Sam: No, it certainly predates our technology. This is something that yogis have been talking about and struggling with for thousands of years. Just imagine you're on a beach on vacation where you vowed not to pick up your smart phone for 24 hours. You haven't looked at a screen, you're just enjoying the sound of the waves and the sunset, or trying to. What you're competing with there is this incessant white noise of discursive thinking. And that's something that follows you everywhere. It's something that people tend to only become truly sensitive to once they try to learn to meditate.
You've mentioned in one of your lessons that the more you train in mindful meditation, the more freedom you will have. What do you mean?
Sam: Well, until you have some capacity to be mindful, you have no choice but to be lost in every next thought that arises. You can't notice thought as thought, it just feels like you. So therefore, you're hostage to whatever the emotional or behavioral consequences of those thoughts are. If they're angry thoughts, you're angry. If they're desire thoughts, you're filled with desire. There is very little understanding in Western psychology around an alternative to that. And it's only by importing mindfulness into our thinking that we have begun to dimly see an alternative.
You've said that even if there were no demonstrable health benefits, it would still be valuable to meditate. Why?
Sam: Yeah, people are putting a lot of weight on the demonstrated health and efficiency benefits of mindfulness. I don't doubt that they exist, I think some of the research attesting to them is pretty thin, but it just may in fact be the case that meditation improves your immune system, and staves off dementia, or the thinning of the cortex as we age and many other benefits.
"What was Jesus talking about? Well, he certainly seemed to be talking about a state of mind that I first discovered on MDMA."
[But] it trivializes the real power of the practice. The power of the practice is to discover something fundamental about the nature of consciousness that can liberate you from psychological suffering in each moment that you can be aware of it. And that's a fairly esoteric goal and concern, it's an ancient one. It is something more than a narrow focus on physical health or even the ordinary expectations of well-being.
Yet many scientists in the West and intellectuals, like Richard Dawkins, are skeptical of it. Would you support a double-blind placebo-controlled study of meditation or does that miss the deeper point?
Sam: No, I see value in studying it any way we can. It's a little hard to pick a control condition that really makes sense. But yeah, that's research that I'm actually collaborating in now. There's a team just beginning a study of my app and we're having to pick a control condition. You can't do a true double-blind placebo control because meditation is not a pill, it's a practice. You know what you're being told to do. And if you're being told that you're in the control condition, you might be told to just keep a journal, say, of everything that happened to you yesterday.
One way to look at it is just to take people who haven't done any significant practice and to have them start and compare them to themselves over time using each person as his own control. But there are limitations with that as well. So, it's a little hard to study, but it's certainly not impossible.
And again, the purpose of meditation is not merely to reduce stress or to improve a person's health. And there are certain aspects to it which don't in any linear way reduce stress. You can have stressful experiences as you begin to learn to be mindful. You become more aware of your own neuroses certainly in the beginning, and you become more aware of your capacity to be petty and deceptive and self-deceptive. There are unflattering things to be realized about the character of your own mind. And the question is, "Is there a benefit ultimately to realizing those things?" I think there clearly is.
I'm curious about your background. You left Stanford to practice meditation after an experience with the drug MDMA. How did that lead you to meditation?
Sam: The experience there was that I had a feeling -- what I would consider unconditional love -- for the first time. Whether I ever had the concept of unconditional love in my head at that point, I don't know, I was 18 and not at all religious. But it was an experience that certainly made sense of the kind of language you find in many spiritual traditions, not just what it's like to be fully actualized by those, by, let's say, Christian values. Like, what was Jesus talking about? Well, he certainly seemed to be talking about a state of mind that I first discovered on MDMA. So that led me to religious literature, spiritual or new age literature, and Eastern philosophy.
Looking to make sense of this and put into a larger context that wasn't just synonymous with taking drugs, it was a sketching a path of practice and growth that could lead further across this landscape of mind, which I just had no idea existed. I basically thought you have whatever mind you have, and the prospect of having a radically different experience of consciousness, that would just be a fool's errand, and anyone who claimed to have such an experience would probably be lying.
As you probably know, there's a resurgence of research in psychedelics now, which again I also fully support, and I've had many useful experiences since that first one, on LSD and psilocybin. I don't tend to take those drugs now; it's been many years since I've done anything significant in that area, but the utility is that they work for everyone, more or less, which is to say that they prove beyond any doubt to everyone that it's possible to have a very different experience of consciousness moment to moment. Now, you can have scary experiences on some of these drugs, and I don't recommend them for everybody, but the one thing you can't have is the experience of boredom. [chuckle]
Very true. Going back to your experiences, you've done silent meditation for 18 hours a day with monks abroad. Do you think that kind of immersive commitment is an ideal goal, or is there a point where too much meditation is counter-productive to a full life?
Sam: I think all of those possibilities are true, depending on the person. There are people who can't figure out how to live a satisfying life in the world, and they retreat as a way of trying to untie the knot of their unhappiness directly through practice.
But the flip side is also true, that in order to really learn this skill deeply, most people need some kind of full immersion experience, at least at some point, to break through to a level of familiarity with it that would be very hard to get for most people practicing for 10 minutes a day, or an hour a day. But ultimately, I think it is a matter of practicing for short periods, frequently, more than it's a matter of long hours in one's daily life. If you could practice for one minute, 100 times a day, that would be an extraordinarily positive way to punctuate your habitual distraction. And I think probably better than 100 minutes all in one go first thing in the morning.
"It's amazing to me to walk into a classroom where you see 15 or 20 six-year-olds sitting in silence for 10 or 15 minutes."
What's your daily meditation practice like today? How does it fit into your routine?
Sam: It's super variable. There are days where I don't find any time to practice formally, there are days where it's very brief, and there are days where I'll set aside a half hour. I have young kids who I don't feel like leaving to go on retreat just yet, but I'm sure retreat will be a part of my future as well. It's definitely useful to just drop everything and give yourself permission to not think about anything for a certain period. And you're left with this extraordinarily vivid confrontation with your default state, which is your thoughts are incessantly appearing and capturing your attention and deluding you.
Every time you're lost in thought, you're very likely telling yourself a story for the 15th time that you don't even have the decency to find boring, right? Just imagine what it would sound like if you could broadcast your thoughts on a loud speaker, it would be mortifying. These are desperately boring, repetitive rehearsals of past conversations and anxieties about the future and meaningless judgments and observations. And in each moment that we don't notice a thought as a thought, we are deluded about what has happened. It's created this feeling of self that is a misconstrual of what consciousness is actually like, and it's created in most cases a kind of emotional emergency, which is our lives and all of the things we're worrying about. But our worry adds absolutely nothing to our capacity to deal with the problems when they actually arise.
Right. You mentioned you're a parent of a young kid, and so am I. Is there anything we as parents can do to encourage a mindfulness habit when our kids are young?
Sam: Actually, we just added meditations for kids in the app. My wife, Annaka, teaches meditation to kids as young as five in school. And they can absolutely learn to be mindful, even at that age. And it's amazing to me to walk into a classroom where you see 15 or 20 six-year-olds sitting in silence for 10 or 15 minutes, it's just amazing. And that's not what happens on the first day, but after five or six classes that is what happens. For a six-year-old to become aware of their emotional life in a clear way and to recognize that he was sad, or angry…that's a kind of super power. And it becomes a basis of any further capacity to regulate emotion and behavior.
It can be something that they're explicitly taught early and it can be something that they get modeled by us. They can know that we practice. You can just sit with your kid when your kid is playing. Just a few minutes goes a long way. You model this behavior and punctuate your own distraction for a short period of time, and it can be incredibly positive.
Lastly, a bonus question that is definitely tongue-in-cheek. Who would win in a fight, you or Ben Affleck?
Sam: That's funny. That question was almost resolved in the green room after that encounter. That was an unpleasant meeting…I spend some amount of time training in the martial arts. This is one area where knowledge does count for a lot, but I don't think we'll have to resolve that uncertainty any time soon. We're both getting old.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Opioid prescription policies may hurt those in chronic pain
Guidelines aim to prevent opioid-related deaths by making it more challenging to get prescriptions, but they can also block access for those who desperately need them.
Tinu Abayomi-Paul works as a writer and activist, plus one unwanted job: Trying to fill her opioid prescription. She says that some pharmacists laugh and tell her that no one needs the amount of pain medication that she is seeking. Another pharmacist near her home in Venus, Tex., refused to fill more than seven days of a 30-day prescription.
To get a new prescription—partially filled opioid prescriptions can’t be dispensed later—Abayomi-Paul needed to return to her doctor’s office. But without her medication, she was having too much pain to travel there, much less return to the pharmacy. She rationed out the pills over several weeks, an agonizing compromise that left her unable to work, interact with her children, sleep restfully, or leave the house. “Don’t I deserve to do more than survive?” she says.
Abayomi-Paul’s pain results from a degenerative spine disorder, chronic lymphocytic leukemia, and more than a dozen other diagnoses and disabilities. She is part of a growing group of people with chronic pain who have been negatively impacted by the fallout from efforts to prevent opioid overdose deaths.
Guidelines for dispensing these pills are complicated because many opioids, like codeine, oxycodone, and morphine, are prescribed legally for pain. Yet, deaths from opioids have increased rapidly since 1999 and become a national emergency. Many of them, such as heroin, are used illegally. The CDC identified three surges in opioid use: an increase in opioid prescriptions in the ‘90s, a surge of heroin around 2010, and an influx of fentanyl and other powerful synthetic opioids in 2013.
As overdose deaths grew, so did public calls to address them, prompting the CDC to change its prescription guidelines in 2016. The new guidelines suggested limiting medication for acute pain to a seven-day supply, capping daily doses of morphine, and other restrictions. Some statistics suggest that these policies have worked; from 2016 to 2019, prescriptions for opiates fell 44 percent. Physicians also started progressively lowering opioid doses for patients, a practice called tapering. A study tracking nearly 100,000 Medicare subscribers on opioids found that about 13 percent of patients were tapering in 2012, and that number increased to about 23 percent by 2017.
But some physicians may be too aggressive with this tapering strategy. About one in four people had doses reduced by more than 10 percent per week, a rate faster than the CDC recommends. The approach left people like Abayomi-Paul without the medication they needed. Every year, Abayomi-Paul says, her prescriptions are harder to fill. David Brushwood, a pharmacy professor who specializes in policy and outcomes at the University of Florida in Gainesville, says opioid dosing isn’t one-size-fits-all. “Patients need to be taken care of individually, not based on what some government agency says they need,” he says.
‘This is not survivable’
Health policy and disability rights attorney Erin Gilmer advocated for people with pain, using her own experience with chronic pain and a host of medical conditions as a guidepost. She launched an advocacy website, Healthcare as a Human Right, and shared her struggles on Twitter: “This pain is more than anything I've endured before and I've already been through too much. Yet because it's not simply identified no one believes it's as bad as it is. This is not survivable.”
When her pain dramatically worsened midway through 2021, Gilmer’s posts grew ominous: “I keep thinking it can't possibly get worse but somehow every day is worse than the last.”
The CDC revised its guidelines in 2022 after criticisms that people with chronic pain were being undertreated, enduring dangerous withdrawal symptoms, and suffering psychological distress. (Long-term opioid use can cause physical dependency, an adaptive reaction that is different than the compulsive misuse associated with a substance use disorder.) It was too late for Gilmer. On July 7, 2021, the 38-year-old died by suicide.
Last August, an Ohio district court ruling set forth a new requirement for Walgreens, Walmart, and CVS pharmacists in two counties. These pharmacists must now document opioid prescriptions that are turned down, even for customers who have no previous purchases at that pharmacy, and they’re required to share this information with other locations in the same chain. None of the three pharmacies responded to an interview request from Leaps.org.
In a practice called red flagging, pharmacists may label a prescription suspicious for a variety of reasons, such as if a pharmacist observes an unusually high dose, a long distance from the patient’s home to the pharmacy, or cash payment. Pharmacists may question patients or prescribers to resolve red flags but, regardless of the explanation, they’re free to refuse to fill a prescription.
As the risk of litigation has grown, so has finger-pointing, says Seth Whitelaw, a compliance consultant at Whitelaw Compliance Group in West Chester, PA, who advises drug, medical device, and biotech companies. Drugmakers accused in National Prescription Opioid Litigation (NPOL), a complex set of thousands of cases on opioid epidemic deaths, which includes the Ohio district case, have argued that they shouldn’t be responsible for the large supply of opiates and overdose deaths. Yet, prosecutors alleged that these pharmaceutical companies hid addiction and overdose risks when labeling opioids, while distributors and pharmacists failed to identify suspicious orders or scripts.
Patients and pharmacists fear red flags
The requirements that pharmacists document prescriptions they refuse to fill so far only apply to two counties in Ohio. But Brushwood fears they will spread because of this precedent, and because there’s no way for pharmacists to predict what new legislation is on the way. “There is no definition of a red flag, there are no lists of red flags. There is no instruction on what to do when a red flag is detected. There’s no guidance on how to document red flags. It is a standardless responsibility,” Brushwood says. This adds trepidation for pharmacists—and more hoops to jump through for patients.
“I went into the doctor one day here and she said, ‘I'm going to stop prescribing opioids to all my patients effective immediately,” Nicolson says.
“We now have about a dozen studies that show that actually ripping somebody off their medication increases their risk of overdose and suicide by three to five times, destabilizes their health and mental health, often requires some hospitalization or emergency care, and can cause heart attacks,” says Kate Nicolson, founder of the National Pain Advocacy Center based in Boulder, Colorado. “It can kill people.” Nicolson was in pain for decades due to a surgical injury to the nerves leading to her spinal cord before surgeries fixed the problem.
Another issue is that primary care offices may view opioid use as a reason to turn down new patients. In a 2021 study, secret shoppers called primary care clinics in nine states, identifying themselves as long-term opioid users. When callers said their opioids were discontinued because their former physician retired, as opposed to an unspecified reason, they were more likely to be offered an appointment. Even so, more than 40 percent were refused an appointment. The study authors say their findings suggest that some physicians may try to avoid treating people who use opioids.
Abayomi-Paul says red flagging has changed how she fills prescriptions. “Once I go to one place, I try to [continue] going to that same place because of the amount of records that I have and making sure my medications don’t conflict,” Abayomi-Paul says.
Nicolson moved to Colorado from Washington D.C. in 2015, before the CDC issued its 2016 guidelines. When the guidelines came out, she found the change to be shockingly abrupt. “I went into the doctor one day here and she said, ‘I'm going to stop prescribing opioids to all my patients effective immediately.’” Since then, she’s spoken with dozens of patients who have been red-flagged or simply haven’t been able to access pain medication.
Despite her expertise, Nicolson isn’t positive she could successfully fill an opioid prescription today even if she needed one. At this point, she’s not sure exactly what various pharmacies would view as a red flag. And she’s not confident that these red flags even work. “You can have very legitimate reasons for being 50 miles away or having to go to multiple pharmacies, given that there are drug shortages now, as well as someone refusing to fill [a prescription.] It doesn't mean that you’re necessarily ‘drug seeking.’”
While there’s no easy solution. Whitelaw says clarifying the role of pharmacists and physicians in patient access to opioids could help people get the medication they need. He is seeking policy changes that focus on the needs of people in pain more than the number of prescriptions filled. He also advocates standardizing the definition of red flags and procedures for resolving them. Still, there will never be a single policy that can be applied to all people, explains Brushwood, the University of Florida professor. “You have to make a decision about each individual prescription.”
Recent immigration restrictions have left many foreign researchers' projects and careers in limbo—and some in jeopardy.
This article is part of the magazine, "The Future of Science In America: The Election Issue," co-published by LeapsMag, the Aspen Institute Science & Society Program, and GOOD.
When COVID-19 cases were surging in New York City in early spring, Chitra Mohan, a postdoctoral fellow at Weill Cornell, was overwhelmed with worry. But the pandemic was only part of her anxieties. Having come to the United States from India on a student visa that allowed her to work for a year after completing her degree, she had applied for a two-year extension, typically granted for those in STEM fields. But due to a clerical error—Mohan used an electronic signatureinstead of a handwritten one— her application was denied and she could no longerwork in the United States.
"I was put on unpaid leave and I lost my apartment and my health insurance—and that was in the middle of COVID!" she says.
Meanwhile her skills were very much needed in those unprecedented times. A molecular biologist studying how DNA can repair itself, Mohan was trained in reverse transcription polymerase chain reaction or RT-PCR—a lab technique that detects pathogens and is used to diagnose COVID-19. Mohan wanted to volunteer at testing centers, but because she couldn't legally work in the U.S., she wasn't allowed to help either. She moved to her cousin's house, hired a lawyer, and tried to restore her work status.
"I spent about $4,000 on lawyer fees and another $1,200 to pay for the motions I filed," she recalls. "I had to borrow money from my parents and my cousin because without my salary I just didn't have the $7,000 at hand." But the already narrow window of opportunity slammed completely shut when the Trump administration suspended issuing new visas for foreign researchers in June. All Mohan's attempts were denied. In August, she had to leave the country. "Given the recent work visa ban by the administration, all my options in the U.S. are closed," she wrote a bitter note on Twitter. "I have to uproot my entire life in NY for the past 6 years and leave." She eventually found a temporary position in Calcutta, where she can continue research.
Mohan is hardly alone in her visa saga. Many foreign scholars on H- and J-type visas and other permits that let them remain employed in America had been struggling to keep their rights to continue research, which in certain cases is crucial to battling the pandemic. Some had to leave the country, some filed every possible extension to buy time, and others are stuck in their home countries, unable to return. The already cumbersome process of applying for visas and extensions became crippled during the lockdowns. But in June, when President Trump extended and expanded immigration restrictions to cut the number of immigrant workers entering the U.S., the new limits left researchers' projects and careers in limbo—and some in jeopardy.
"We have been a beneficiary of this flow of human capacity and resource investment for many generations—and this is now threatened."
Rakesh Ramachandran, whose computational biology work contributed to one of the first coronavirus studies to map out its protein structures—is stranded in India. In early March, he had travelled there to attend a conference and visit the American consulate to stamp his H1 visa for a renewal, already granted. The pandemic shut down both the conference and the consulates, and Ramachandran hasn't been able to come back since. The consulates finally opened in September, but so far the online portal has no available appointment slots. "I'm told to keep trying," Ramachandran says.
The visa restrictions affected researchers worldwide, regardless of disciplines or countries. A Ph.D. student in neuroscience, Morgane Leroux had to do her experiments with mice at Gladstone Institutes in America and analyze the data back home at Sorbonne University in France. She had finished her first round of experiments when the lockdowns forced her to return to Paris, and she hasn't been able to come back to resume her work since. "I can't continue the experiments, which is really frustrating," she says, especially because she doesn't know what it means for her Ph.D. "I may have to entirely change my subject," she says, which she doesn't want to do—it would be a waste of time and money.
But besides wreaking havoc in scholars' personal lives and careers, the visa restrictions had—and will continue to have—tremendous deleterious effects on America's research and its global scientific competitiveness. "It's incredibly short-sighted and self-destructing to restrict the immigration of scientists into the U.S.," says Benjamin G. Neel, who directs the Laura and Isaac Perlmutter Cancer Center at New York University. "If they can't come here, they will go elsewhere," he says, causing a brain drain.

Neel in his lab with postdocs
(Courtesy of Neel)
Neel felt the outcomes of the shortsighted policies firsthand. In the past few months, his lab lost two postdoctoral researchers who had made major strides in understanding the biology of several particularly stubborn, treatment-resistant malignancies. One postdoc studied the underlying mechanisms responsible for 90 percent of pancreatic cancers and half of the colon ones. The other one devised a new system of modeling ovarian cancer in mice to test new therapeutic drug combinations for the deadliest tumor types—but had to return home to China.
"By working around the clock, she was able to get her paper accepted, but she hasn't been able to train us to use this new system, which can set us back six months," Neel says.
Her discoveries also helped the lab secure about $900,000 in grants for new research. Losing people like this is "literally killing the goose that lays the golden eggs," Neel adds. "If you want to make America poor again, this is the way to do it."
Cassidy R. Sugimoto at Indiana University Bloomington, who studies how scientific knowledge is produced and disseminated, says that scientists are the most productive when they are free to move, exchange ideas, and work at labs with the best equipment. Restricting that freedom reduces their achievement.
"Several empirical studied demonstrated the benefits to the U.S. by attracting and retaining foreign scientists. The disproportional number of our Nobel Prize winners were not only foreign-born but also foreign-educated," she says. Scientific advancement bolsters the country's economic prowess, too, so turning scholars away is bad for the economy long-term. "We have been a beneficiary of this flow of human capacity and resource investment for many generations—and this is now threatened," Sugimoto adds—because scientists will look elsewhere. "We are seeing them shifting to other countries that are more hospitable, both ideologically and in terms of health security. Many visiting scholars, postdocs, and graduate students who would otherwise come to the United States are now moving to Canada."
It's not only the Ph.D. students and postdocs who are affected. In some cases, even well-established professors who have already made their marks in the field and direct their own labs at prestigious research institutions may have to pack up and leave the country in the next few months. One scientist who directs a prominent neuroscience lab is betting on his visa renewal and a green card application, but if that's denied, the entire lab may be in jeopardy, as many grants hinge on his ability to stay employed in America.
"It's devastating to even think that it can happen," he says—after years of efforts invested. "I can't even comprehend how it would feel. It would be terrifying and really sad." (He asked to withhold his name for fear that it may adversely affect his applications.) Another scientist who originally shared her story for this article, later changed her mind and withdrew, worrying that speaking out may hurt the entire project, a high-profile COVID-19 effort. It's not how things should work in a democratic country, scientists admit, but that's the reality.
Still, some foreign scholars are speaking up. Mehmet Doğan, a physicist at University of California Berkeley who has been fighting a visa extension battle all year, says it's important to push back in an organized fashion with petitions and engage legislators. "This administration was very creative in finding subtle and not so subtle ways to make our lives more difficult," Doğan says. He adds that the newest rules, proposed by the Department of Homeland Security on September 24, could further limit the time scholars can stay, forcing them into continuous extension battles. That's why the upcoming election might be a turning point for foreign academics. "This election will decide if many of us will see the U.S. as the place to stay and work or whether we look at other countries," Doğan says, echoing the worries of Neel, Sugimoto, and others in academia.

Dogan on Zoom talking to his fellow union members of the Academic Researchers United, a union of almost 5,000 Academic Researchers.
(Credit: Ceyda Durmaz Dogan)
If this year has shown us anything, it is that viruses and pandemics know no borders as they sweep across the globe. Likewise, science can't be restrained by borders either. "Science is an international endeavor," says Neel—and right now humankind now needs unified scientific research more than ever, unhindered by immigration hurdles and visa wars. Humanity's wellbeing in America and beyond depends on it.
[Editor's Note: To read other articles in this special magazine issue, visit the beautifully designed e-reader version.]
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

