One of the World’s Most Famous Neuroscientists Wants You to Embrace Meditation and Spirituality
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
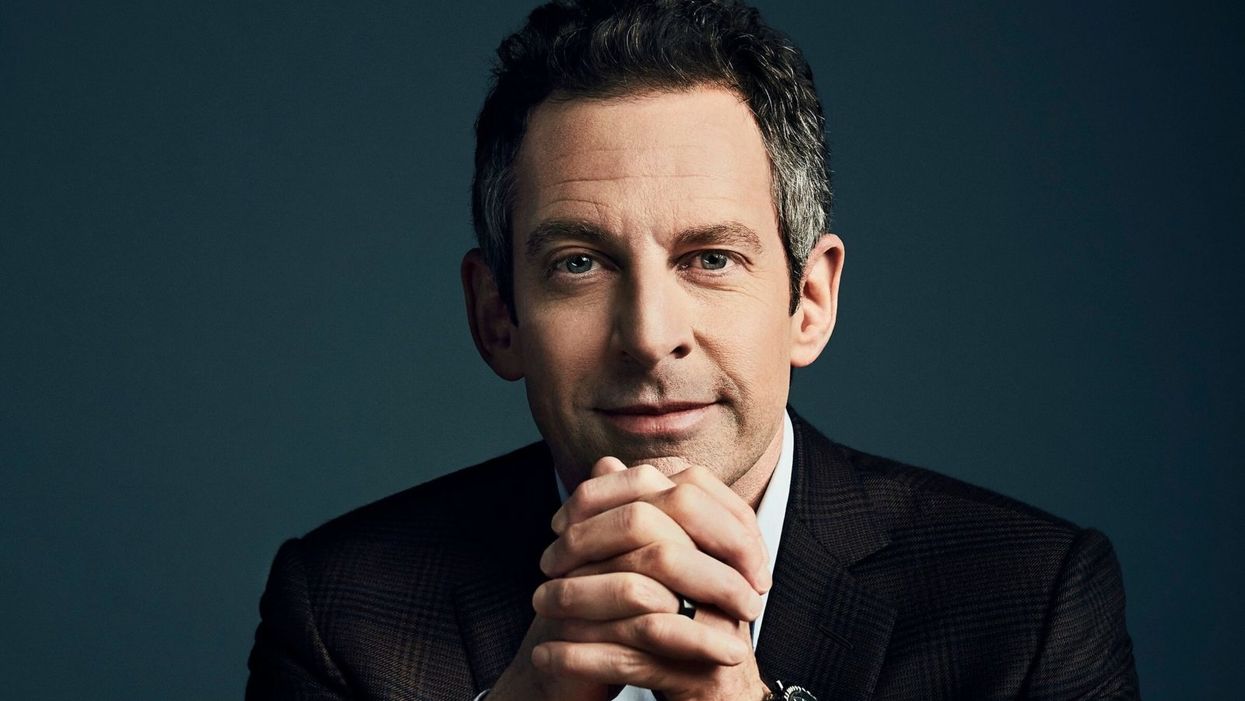
Sam Harris, the neuroscientist and bestselling author, discusses mindfulness meditation.
Neuroscientist, philosopher, and bestselling author Sam Harris is famous for many reasons, among them his vocal criticism of religion, his scientific approach to moral questions, and his willingness to tackle controversial topics on his popular podcast.
"Until you have some capacity to be mindful, you have no choice but to be lost in every next thought that arises."
He is also a passionate advocate of mindfulness meditation, having spent formative time as a young adult learning from teachers in India and Tibet before returning to the West.
Now his new app called Waking Up aims to teach the principles of meditation to anyone who is willing to slow down, turn away from everyday distractions, and pay attention to their own mind. Harris recently chatted with leapsmag about the science of mindfulness, the surprising way he discovered it, and the fundamental—but under-appreciated—reason to do it. This conversation has been lightly edited and condensed.
One of the biggest struggles that so many people face today is how to stay present in the moment. Is this the default state for human beings, or is this a more recent phenomenon brought on by our collective addiction to screens?
Sam: No, it certainly predates our technology. This is something that yogis have been talking about and struggling with for thousands of years. Just imagine you're on a beach on vacation where you vowed not to pick up your smart phone for 24 hours. You haven't looked at a screen, you're just enjoying the sound of the waves and the sunset, or trying to. What you're competing with there is this incessant white noise of discursive thinking. And that's something that follows you everywhere. It's something that people tend to only become truly sensitive to once they try to learn to meditate.
You've mentioned in one of your lessons that the more you train in mindful meditation, the more freedom you will have. What do you mean?
Sam: Well, until you have some capacity to be mindful, you have no choice but to be lost in every next thought that arises. You can't notice thought as thought, it just feels like you. So therefore, you're hostage to whatever the emotional or behavioral consequences of those thoughts are. If they're angry thoughts, you're angry. If they're desire thoughts, you're filled with desire. There is very little understanding in Western psychology around an alternative to that. And it's only by importing mindfulness into our thinking that we have begun to dimly see an alternative.
You've said that even if there were no demonstrable health benefits, it would still be valuable to meditate. Why?
Sam: Yeah, people are putting a lot of weight on the demonstrated health and efficiency benefits of mindfulness. I don't doubt that they exist, I think some of the research attesting to them is pretty thin, but it just may in fact be the case that meditation improves your immune system, and staves off dementia, or the thinning of the cortex as we age and many other benefits.
"What was Jesus talking about? Well, he certainly seemed to be talking about a state of mind that I first discovered on MDMA."
[But] it trivializes the real power of the practice. The power of the practice is to discover something fundamental about the nature of consciousness that can liberate you from psychological suffering in each moment that you can be aware of it. And that's a fairly esoteric goal and concern, it's an ancient one. It is something more than a narrow focus on physical health or even the ordinary expectations of well-being.
Yet many scientists in the West and intellectuals, like Richard Dawkins, are skeptical of it. Would you support a double-blind placebo-controlled study of meditation or does that miss the deeper point?
Sam: No, I see value in studying it any way we can. It's a little hard to pick a control condition that really makes sense. But yeah, that's research that I'm actually collaborating in now. There's a team just beginning a study of my app and we're having to pick a control condition. You can't do a true double-blind placebo control because meditation is not a pill, it's a practice. You know what you're being told to do. And if you're being told that you're in the control condition, you might be told to just keep a journal, say, of everything that happened to you yesterday.
One way to look at it is just to take people who haven't done any significant practice and to have them start and compare them to themselves over time using each person as his own control. But there are limitations with that as well. So, it's a little hard to study, but it's certainly not impossible.
And again, the purpose of meditation is not merely to reduce stress or to improve a person's health. And there are certain aspects to it which don't in any linear way reduce stress. You can have stressful experiences as you begin to learn to be mindful. You become more aware of your own neuroses certainly in the beginning, and you become more aware of your capacity to be petty and deceptive and self-deceptive. There are unflattering things to be realized about the character of your own mind. And the question is, "Is there a benefit ultimately to realizing those things?" I think there clearly is.
I'm curious about your background. You left Stanford to practice meditation after an experience with the drug MDMA. How did that lead you to meditation?
Sam: The experience there was that I had a feeling -- what I would consider unconditional love -- for the first time. Whether I ever had the concept of unconditional love in my head at that point, I don't know, I was 18 and not at all religious. But it was an experience that certainly made sense of the kind of language you find in many spiritual traditions, not just what it's like to be fully actualized by those, by, let's say, Christian values. Like, what was Jesus talking about? Well, he certainly seemed to be talking about a state of mind that I first discovered on MDMA. So that led me to religious literature, spiritual or new age literature, and Eastern philosophy.
Looking to make sense of this and put into a larger context that wasn't just synonymous with taking drugs, it was a sketching a path of practice and growth that could lead further across this landscape of mind, which I just had no idea existed. I basically thought you have whatever mind you have, and the prospect of having a radically different experience of consciousness, that would just be a fool's errand, and anyone who claimed to have such an experience would probably be lying.
As you probably know, there's a resurgence of research in psychedelics now, which again I also fully support, and I've had many useful experiences since that first one, on LSD and psilocybin. I don't tend to take those drugs now; it's been many years since I've done anything significant in that area, but the utility is that they work for everyone, more or less, which is to say that they prove beyond any doubt to everyone that it's possible to have a very different experience of consciousness moment to moment. Now, you can have scary experiences on some of these drugs, and I don't recommend them for everybody, but the one thing you can't have is the experience of boredom. [chuckle]
Very true. Going back to your experiences, you've done silent meditation for 18 hours a day with monks abroad. Do you think that kind of immersive commitment is an ideal goal, or is there a point where too much meditation is counter-productive to a full life?
Sam: I think all of those possibilities are true, depending on the person. There are people who can't figure out how to live a satisfying life in the world, and they retreat as a way of trying to untie the knot of their unhappiness directly through practice.
But the flip side is also true, that in order to really learn this skill deeply, most people need some kind of full immersion experience, at least at some point, to break through to a level of familiarity with it that would be very hard to get for most people practicing for 10 minutes a day, or an hour a day. But ultimately, I think it is a matter of practicing for short periods, frequently, more than it's a matter of long hours in one's daily life. If you could practice for one minute, 100 times a day, that would be an extraordinarily positive way to punctuate your habitual distraction. And I think probably better than 100 minutes all in one go first thing in the morning.
"It's amazing to me to walk into a classroom where you see 15 or 20 six-year-olds sitting in silence for 10 or 15 minutes."
What's your daily meditation practice like today? How does it fit into your routine?
Sam: It's super variable. There are days where I don't find any time to practice formally, there are days where it's very brief, and there are days where I'll set aside a half hour. I have young kids who I don't feel like leaving to go on retreat just yet, but I'm sure retreat will be a part of my future as well. It's definitely useful to just drop everything and give yourself permission to not think about anything for a certain period. And you're left with this extraordinarily vivid confrontation with your default state, which is your thoughts are incessantly appearing and capturing your attention and deluding you.
Every time you're lost in thought, you're very likely telling yourself a story for the 15th time that you don't even have the decency to find boring, right? Just imagine what it would sound like if you could broadcast your thoughts on a loud speaker, it would be mortifying. These are desperately boring, repetitive rehearsals of past conversations and anxieties about the future and meaningless judgments and observations. And in each moment that we don't notice a thought as a thought, we are deluded about what has happened. It's created this feeling of self that is a misconstrual of what consciousness is actually like, and it's created in most cases a kind of emotional emergency, which is our lives and all of the things we're worrying about. But our worry adds absolutely nothing to our capacity to deal with the problems when they actually arise.
Right. You mentioned you're a parent of a young kid, and so am I. Is there anything we as parents can do to encourage a mindfulness habit when our kids are young?
Sam: Actually, we just added meditations for kids in the app. My wife, Annaka, teaches meditation to kids as young as five in school. And they can absolutely learn to be mindful, even at that age. And it's amazing to me to walk into a classroom where you see 15 or 20 six-year-olds sitting in silence for 10 or 15 minutes, it's just amazing. And that's not what happens on the first day, but after five or six classes that is what happens. For a six-year-old to become aware of their emotional life in a clear way and to recognize that he was sad, or angry…that's a kind of super power. And it becomes a basis of any further capacity to regulate emotion and behavior.
It can be something that they're explicitly taught early and it can be something that they get modeled by us. They can know that we practice. You can just sit with your kid when your kid is playing. Just a few minutes goes a long way. You model this behavior and punctuate your own distraction for a short period of time, and it can be incredibly positive.
Lastly, a bonus question that is definitely tongue-in-cheek. Who would win in a fight, you or Ben Affleck?
Sam: That's funny. That question was almost resolved in the green room after that encounter. That was an unpleasant meeting…I spend some amount of time training in the martial arts. This is one area where knowledge does count for a lot, but I don't think we'll have to resolve that uncertainty any time soon. We're both getting old.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Questions remain about new drug for hot flashes
In May, a new drug, Fezolinetant, was approved by the FDA to treat hot flashes associated with menopause.
Vascomotor symptoms (VMS) is the medical term for hot flashes associated with menopause. You are going to hear a lot more about it because a company has a new drug to sell. Here is what you need to know.
Menopause marks the end of a woman’s reproductive capacity. Normal hormonal production associated with that monthly cycle becomes erratic and finally ceases. For some women the transition can be relatively brief with only modest symptoms, while for others the body's “thermostat” in the brain is disrupted and they experience hot flashes and other symptoms that can disrupt daily activity. Lifestyle modification and drugs such as hormone therapy can provide some relief, but women at risk for cancer are advised not to use them and other women choose not to do so.
Fezolinetant, sold by Astellas Pharma Inc. under the product name Veozah™, was approved by the Food and Drug Administration (FDA) on May 12 to treat hot flashes associated with menopause. It is the first in a new class of drugs called neurokinin 3 receptor antagonists, which block specific neurons in the brain “thermostat” that trigger VMS. It does not appear to affect other symptoms of menopause. As with many drugs targeting a brain cell receptor, it must be taken continuously for a few days to build up a good therapeutic response, rather than working as a rescue product such as an asthma inhaler to immediately treat that condition.
Hot flashes vary greatly and naturally get better or resolve completely with time. That contributes to a placebo effect and makes it more difficult to judge the outcome of any intervention. Early this year, a meta analysis of 17 studies of drug trials for hot flashes found an unusually large placebo response in those types of studies; the placebo groups had an average of 5.44 fewer hot flashes and a 36 percent reduction in their severity.
In studies of fezolinetant, the drug recently approved by the FDA, the placebo benefit was strong and persistent. The drug group bested the placebo response to a statistically significant degree but, “If people have gone from 11 hot flashes a day to eight or seven in the placebo group and down to a couple fewer ones in the drug groups, how meaningful is that? Having six hot flashes a day is still pretty unpleasant,” says Diana Zuckerman, president of the National Center for Health Research (NCHR), a health oriented think tank.
“Is a reduction compared to placebo of 2-3 hot flashes per day, in a population of women experiencing 10-11 moderate to severe hot flashes daily, enough relief to be clinically meaningful?” Andrea LaCroix asked a commentary published in Nature Medicine. She is an epidemiologist at the University of California San Diego and a leader of the MsFlash network that has conducted a handful of NIH-funded studies on menopause.
Questions Remain
LaCroix and others have raised questions about how Astellas, the company that makes the new drug, handled missing data from patients who dropped out of the clinical trials. “The lack of detailed information about important parameters such as adherence and missing data raises concerns that the reported benefits of fezolinetant very likely overestimate those that will be observed in clinical practice," LaCroix wrote.
In response to this concern, Anna Criddle, director of global portfolio communications at Astellas, wrote in an email to Leaps.org: “…a full analysis of data, including adherence data and any impact of missing data, was submitted for assessment by [the FDA].”
The company ran the studies at more than 300 sites around the world. Curiously, none appear to have been at academic medical centers, which are known for higher quality research. Zuckerman says, "When somebody is paid to do a study, if they want to get paid to do another study by the same company, they will try to make sure that the results are the results that the company wants.”
Criddle said that Astellas picked the sites “that would allow us to reach a diverse population of women, including race and ethnicity.”
A trial of a lower dose of the drug was conducted in Asia. In March 2022, Astellas issued a press release saying it had failed to prove effectiveness. No further data has been released. Astellas still plans to submit the data, according to Criddle. Results from clinical trials funded by the U.S. goverment must be reported on clinicaltrials.gov within one year of the study's completion - a deadline that, in this case, has expired.
The measurement scale for hot flashes used in the studies, mild-moderate-severe, also came in for criticism. “It is really not good scale, there probably isn’t a broad enough range of things going on or descriptors,” says David Rind. He is chief medical officer of the Institute for Clinical and Economic Review (ICER), a nonprofit authority on new drugs. It conducted a thorough review and analysis of fezolinestant using then existing data gathered from conference abstracts, posters and presentations and included a public stakeholder meeting in December. A 252-page report was published in January, finding “considerable uncertainty about the comparative net health benefits of fezolinetant” versus hormone therapy.
Questions surrounding some of these issues might have been answered if the FDA had chosen to hold a public advisory committee meeting on fezolinetant, which it regularly does for first in class medicines. But the agency decided such a meeting was unnecessary.
Cost
There was little surprise when Astellas announced a list price for fezolinetant of $550 a month ($6000 annually) and a program of patient assistance to ease out of pocket expenses. The company had already incurred large expenses.
In 2017 Astellas purchased the company that originally developed fezolinetant for $534 million plus several hundred million in potential royalties. The drug company ran a "disease awareness” ad, Heat on the Street, hat aired during the Super Bowl in February, where 30 second ads cost about $7 million. Industry analysts have projected sales to be $1.9 billion by 2028.
ICER’s pre-approval evaluation said fezolinetant might "be considered cost-effective if priced around $2,000 annually. ... [It]will depend upon its price and whether it is considered an alternative to MHT [menopause hormone treatment] for all women or whether it will primarily be used by women who cannot or will not take MHT."
Criddle wrote that Astellas set the price based on the novelty of the science, the quality of evidence for the drug and its uniqueness compared to the rest of the market. She noted that an individual’s payment will depend on how much their insurance company decides to cover. “[W]e expect insurance coverage to increase over the course of the year and to achieve widespread coverage in the U.S. over time.”
Leaps.org wrote to and followed up with nine of the largest health insurers/providers asking basic questions about their coverage of fezolinetant. Only two responded. Jennifer Martin, the deputy chief consultant for pharmacy benefits management at the Department of Veterans Affairs, said the agency “covers all drugs from the date that they are launched.” Decisions on whether it will be included in the drug formulary and what if any copays might be required are under review.
“[Fezolinetant] will go through our standard P&T Committee [patient and treatment] review process in the next few months, including a review of available efficacy data, safety data, clinical practice guidelines, and comparison with other agents used for vasomotor symptoms of menopause," said Phil Blando, executive director of corporate communications for CVS Health.
Other insurers likely are going through a similar process to decide issues such as limiting coverage to women who are advised not to use hormones, how much copay will be required, and whether women will be required to first try other options or obtain approvals before getting a prescription.
Rind wants to see a few years of use before he prescribes fezolinetant broadly, and believes most doctors share his view. Nor will they be eager to fill out the additional paperwork required for women to participate in the Astellas patient assistance program, he added.
Safety
Astellas is marketing its drug by pointing out risks of hormone therapy, such as a recent paper in The BMJ, which noted that women who took hormones for even a short period of time had a 24 percent increased risk of dementia. While the percentage was scary, the combined number of women both on and off hormones who developed dementia was small. And it is unclear whether hormones are causing dementia or if more severe hot flashes are a marker for higher risk of developing dementia. This information is emerging only after 80 years of hundreds of millions of women using hormones.
In contrast, the label for fezolinetant prohibits “concomitant use with CYP1A2 inhibitors” and requires testing for liver and kidney function prior to initiating the drug and every three months thereafter. There is no human or animal data on use in a geriatric population, defined as 65 or older, a group that is likely to use the drug. Only a few thousand women have ever taken fezolinetant and most have used it for just a few months.
Options
A woman seeking relief from symptoms of menopause would like to see how fezolintant compares with other available treatment options. But Astellas did not conduct such a study and Andrea LaCroix says it is unlikely that anyone ever will.
ICER has come the closest, with a side-by-side analysis of evidence-based treatments and found that fezolinetant performed quite similarly and modestly as the others in providing relief from hot flashes. Some treatments also help with other symptoms of menopause, which fezolinetant does not.
There are many coping strategies that women can adopt to deal with hot flashes; one of the most common is dressing in layers (such as a sleeveless blouse with a sweater) that can be added or subtracted as conditions require. Avoiding caffeine, hot liquids, and spicy foods is another common strategy. “I stopped drinking hot caffeinated drinks…for several years, and you get out of the habit of drinking them,” says Zuckerman.
LaCroix curates those options at My Meno Plan, which includes a search function where you can enter your symptoms and identify which treatments might work best for you. It also links to published research papers. She says the goal is to empower women with information to make informed decisions about menopause.
A company in England has made a test that picks out the compounds from breath that reveal if people have liver disease.
Every year, around two million people worldwide die of liver disease. While some people inherit the disease, it’s most commonly caused by hepatitis, obesity and alcoholism. These underlying conditions kill liver cells, causing scar tissue to form until eventually the liver cannot function properly. Since 1979, deaths due to liver disease have increased by 400 percent.
The sooner the disease is detected, the more effective treatment can be. But once symptoms appear, the liver is already damaged. Around 50 percent of cases are diagnosed only after the disease has reached the final stages, when treatment is largely ineffective.
To address this problem, Owlstone Medical, a biotech company in England, has developed a breath test that can detect liver disease earlier than conventional approaches. Human breath contains volatile organic compounds (VOCs) that change in the first stages of liver disease. Owlstone’s breath test can reliably collect, store and detect VOCs, while picking out the specific compounds that reveal liver disease.
“There’s a need to screen more broadly for people with early-stage liver disease,” says Owlstone’s CEO Billy Boyle. “Equally important is having a test that's non-invasive, cost effective and can be deployed in a primary care setting.”
The standard tool for detection is a biopsy. It is invasive and expensive, making it impractical to use for people who aren't yet symptomatic. Meanwhile, blood tests are less invasive, but they can be inaccurate and can’t discriminate between different stages of the disease.
In the past, breath tests have not been widely used because of the difficulties of reliably collecting and storing breath. But Owlstone’s technology could help change that.
The team is testing patients in the early stages of advanced liver disease, or cirrhosis, to identify and detect these biomarkers. In an initial study, Owlstone’s breathalyzer was able to pick out patients who had early cirrhosis with 83 percent sensitivity.
Boyle’s work is personally motivated. His wife died of colorectal cancer after she was diagnosed with a progressed form of the disease. “That was a big impetus for me to see if this technology could work in early detection,” he says. “As a company, Owlstone is interested in early detection across a range of diseases because we think that's a way to save lives and a way to save costs.”
How it works
In the past, breath tests have not been widely used because of the difficulties of reliably collecting and storing breath. But Owlstone’s technology could help change that.
Study participants breathe into a mouthpiece attached to a breath sampler developed by Owlstone. It has cartridges are designed and optimized to collect gases. The sampler specifically targets VOCs, extracting them from atmospheric gases in breath, to ensure that even low levels of these compounds are captured.
The sampler can store compounds stably before they are assessed through a method called mass spectrometry, in which compounds are converted into charged atoms, before electromagnetic fields filter and identify even the tiniest amounts of charged atoms according to their weight and charge.
The top four compounds in our breath
In an initial study, Owlstone captured VOCs in breath to see which ones could help them tell the difference between people with and without liver disease. They tested the breath of 46 patients with liver disease - most of them in the earlier stages of cirrhosis - and 42 healthy people. Using this data, they were able to create a diagnostic model. Individually, compounds like 2-Pentanone and limonene performed well as markers for liver disease. Owlstone achieved even better performance by examining the levels of the top four compounds together, distinguishing between liver disease cases and controls with 95 percent accuracy.
“It was a good proof of principle since it looks like there are breath biomarkers that can discriminate between diseases,” Boyle says. “That was a bit of a stepping stone for us to say, taking those identified, let’s try and dose with specific concentrations of probes. It's part of building the evidence and steering the clinical trials to get to liver disease sensitivity.”
Sabine Szunerits, a professor of chemistry in Institute of Electronics at the University of Lille, sees the potential of Owlstone’s technology.
“Breath analysis is showing real promise as a clinical diagnostic tool,” says Szunerits, who has no ties with the company. “Owlstone Medical’s technology is extremely effective in collecting small volatile organic biomarkers in the breath. In combination with pattern recognition it can give an answer on liver disease severity. I see it as a very promising way to give patients novel chances to be cured.”
Improving the breath sampling process
Challenges remain. With more than one thousand VOCs found in the breath, it can be difficult to identify markers for liver disease that are consistent across many patients.
Julian Gardner is a professor of electrical engineering at Warwick University who researches electronic sensing devices. “Everyone’s breath has different levels of VOCs and different ones according to gender, diet, age etc,” Gardner says. “It is indeed very challenging to selectively detect the biomarkers in the breath for liver disease.”
So Owlstone is putting chemicals in the body that they know interact differently with patients with liver disease, and then using the breath sampler to measure these specific VOCs. The chemicals they administer are called Exogenous Volatile Organic Compound) probes, or EVOCs.
Most recently, they used limonene as an EVOC probe, testing 29 patients with early cirrhosis and 29 controls. They gave the limonene to subjects at specific doses to measure how its concentrations change in breath. The aim was to try and see what was happening in their livers.
“They are proposing to use drugs to enhance the signal as they are concerned about the sensitivity and selectivity of their method,” Gardner says. “The approach of EVOC probes is probably necessary as you can then eliminate the person-to-person variation that will be considerable in the soup of VOCs in our breath.”
Through these probes, Owlstone could identify patients with liver disease with 83 percent sensitivity. By targeting what they knew was a disease mechanism, they were able to amplify the signal. The company is starting a larger clinical trial, and the plan is to eventually use a panel of EVOC probes to make sure they can see diverging VOCs more clearly.
“I think the approach of using probes to amplify the VOC signal will ultimately increase the specificity of any VOC breath tests, and improve their practical usability,” says Roger Yazbek, who leads the South Australian Breath Analysis Research (SABAR) laboratory in Flinders University. “Whilst the findings are interesting, it still is only a small cohort of patients in one location.”
The future of breath diagnosis
Owlstone wants to partner with pharmaceutical companies looking to learn if their drugs have an effect on liver disease. They’ve also developed a microchip, a miniaturized version of mass spectrometry instruments, that can be used with the breathalyzer. It is less sensitive but will enable faster detection.
Boyle says the company's mission is for their tests to save 100,000 lives. "There are lots of risks and lots of challenges. I think there's an opportunity to really establish breath as a new diagnostic class.”

