Why Are Scientists and Patients Visiting This Island Paradise?
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

An inviting beach in Nassau, Bahamas.
Dr. Conville Brown, a cardiologist-researcher in The Bahamas, is at the helm of a fascinating worldwide project: He's leading a movement to help accelerate innovation by providing scientists and patients from around the globe with a legal, cost-effective, and ethically rigorous place to conduct medical research, as well as to offer commercial therapies that are already approved in some jurisdictions, but not others. He recently spoke with Editor-In-Chief Kira Peikoff about The Bahamas' emerging ascendance in the scientific world. This interview has been edited and condensed for brevity.
"You don't want to take shortcuts from the perspective of not giving proper due diligence to the process, but you also don't want it to be overwhelmed with red tape."
Tell me about the work you do in the Bahamas – what is the research focus?
We have a couple research opportunities here. Several years ago, we established the Partners Clinical Research Centre, the idea being that we can partner with different people in different territories in the world, including the United States, and be able to perform ethical research as would be defined and adjudicated by an institutional review board and a properly constituted ethics committee. We do all of this with FDA rigor, but in a non-FDA jurisdiction.
By doing this, we want to look for the science behind the research, and want to know that there is a sound clinical hypothesis that's going to be tested. We also want to know that the safety of the human subjects is assured as much as possible, and of course, assess the efficacy of that which you're testing. We want to do this in the same manner as the FDA, except in a more accelerated and probably less bureaucratic manner. You don't want to take shortcuts from the perspective of not giving proper due diligence to the process, but you also don't want it to be overwhelmed with red tape, so that what could be 3 months takes 3 years. A jet ski turns around a lot faster than the Queen Mary.
Why do you think the clinical research process in other countries like the U.S. has become burdened with red tape?
The litigious nature of society is a contributing factor. If people are negligent, they deserve to be sued. Unfortunately, all too often, some things get taken too far, and sometimes, the pendulum swings too far in the wrong direction and then it's counterproductive, so the whole process then becomes so very heavily regulated and financially burdensome. A lot of American companies have gone outside the country to get their clinical trials and/or device testing done because it's too phenomenally expensive and time-consuming. We seek to make sure the same degree of diligence is exercised but in a lesser time frame, and of course, at a much lower cost.
The other aspect, of course, is that there are certain opportunities where we have major jurisdictions, as in Europe, that have determined that a therapy or device is safe. Those services and devices we can utilize in the Bahamas--not as a clinical research tool, but as a therapy, which of course, the United States is not able to do without FDA approval. That could easily take another five years. So there is an opportunity for us in that window to make available such therapies and devices to the North American community. I like to call this "Advanced Medical Tourism" or "Advanced TransNational Medical Care." Instead of somebody flying nine hours to Europe, they can also now fly to the Bahamas, as little as half an hour away, and as long as we are satisfied that the science is sound and the approvals are in place from a senior jurisdiction, then we can legally serve any patient that is eligible for that particular therapy.

Dr. Conville Brown
(Courtesy)
Are you seeing an influx of patients for that kind of medical tourism?
The numbers are increasing. The stem cell legislation has now been in place for two to three years, so we have a number of entities including some large international companies coming to the shores of the Bahamas to provide some therapies here, and others for research. The vast majority of our clientele are from abroad, particularly the U.S. We fully plan to increase the traffic flow to the Bahamas for medical tourism, or preferably, TransNational Medical Care, Advanced and Conventional.
How do patients find out about available therapies and trials happening there?
Advertising in the international arena for something that is perfectly legal within the confines of Bahamas is par for the course. But the marketing efforts have not been that heavy while all the processes and procedures are being fine-tuned and the various entities are set up to handle more than 100 people at a time.
"We were able to accelerate those programs, and do it a lot less expensively than can be done in continental countries, but just as well."
What kind of research is being done by companies who have come to the Bahamas?
We've been involved in first-in-man procedures for neuromodulation of the cardiovascular system, where we inserted a device into the blood vessels and stimulated the autonomic nervous system with a view to controlling patients' blood pressure and heart rate in conditions such as congestive heart failure. We have also looked at injectable glucose sensors, to continually monitor the blood glucose, and via a chip, can send the blood glucose measurement back to the patient's cell phone. So the patient looks at his phone for his blood sugar. That was phenomenally exciting, the clinical trial was very positive, and the company is now developing a final prototype to commercialize the product. We were able to accelerate those programs, and do it a lot less expensively than can be done in continental countries, but just as well. The Bahamas has also crafted legislation specifically for regenerative medicine and stem cell research, so that becomes an additional major attraction.
Do you ever find that there is skepticism around going to the Caribbean to do science?
When it comes to clinical research and new medical devices, one might be skeptical about the level of medical/scientific expertise that is resident here. We're here to show that we do in fact have that expertise resident within The Partners Clinical Research Centre, within The Partners Stem Cell Centre, and we have formed our partnerships accordingly so that when prudent and necessary, we bring in additional expertise from the very territories that are seeking to accelerate.
Have you seen a trend toward increasing interest from researchers around the world?
Absolutely. One company, for example, is interested not only in the clinical side, but also the preclinical side--where you can have animal lab experiments done in the Bahamas, and being able to bridge that more readily with the clinical side. That presents a major opportunity for parties involved because again, the financial savings are exponential without compromising standards.
"A person who is 75 and frail, he doesn't want to wait to see if he will make it to 80 to benefit from the agent if it's approved in five years. Instead he can come to our center."
Where are some of these researchers from?
The United States, the Czech Republic, Russia, Canada, and South America. I expect significantly more interest once we promote the idea of European products having a welcome niche in the Bahamas, because we accept federal approvals from the U.S., Canada, and the European Union.
What do you think will be the first medical breakthrough to come out of research there?
One of the biggest killers in the world is heart disease, and we have the opportunity to implement a number of cardiac protocols utilizing stem cell therapy, particularly for those with no options. We just completed a state-of-the art medical center that we fashioned after the University of Miami that is getting ready for prime time. The sky will be the limit for the cardiac patient with respect to stem cell medicine.
Second, we are extremely pleased to be involved with a company called Longeveron, which is looking at how one might age better, and age more slowly, particularly with the administration of young blood and mesenchymal stem cells to frail, elderly candidates. Healthy young men have their mesenchymal stem cells harvested, expanded, and then administered to frail, elderly individuals with a view to improving their Frailty Index and functionality (feeling younger). There is a lot of interest in this arena, as one could imagine.
And herein lies the classical scenario for the Bahamas: Longeveron is now recruiting patients for its phase IIB double blind, placebo-controlled clinical trial at multiple sites across the U.S., which will add some two to three years to its data collection. Originally this work was done with NIH support at the University of Miami's Interdisciplinary Stem Cell Institute by Dr. Joshua Hare, and published in the Journal of Gerontology. So now, during the ongoing and expanded clinical trial, with those positive signals, we are able to have a commercially available clinical registry in the Bahamas. This has been approved by the ethics committee here, which is comprised of international luminaries in regenerative medicine. Longeveron will also be conducting an additional randomized clinical trial arm of same at our Centre in The Bahamas, The Partners Stem Cell Centre.
Can you clarify what you mean by "registry"?
In other words, you still have to fit the eligibility criteria to receive the active agent, but the difference is that in a placebo-controlled double-blind clinical trial, the physician/researcher and the patient don't know if they are getting the active agent or placebo. In the registry, there is no placebo, and you know you're getting the active agent, what we call "open label." You're participating because of the previous information on efficacy and safety.
A person who is 75 and frail, he doesn't want to wait to see if he will make it to 80 to benefit from the agent if it's approved in five years. Instead he can come to our center, one of the designated centers, and as long as he meets the inclusion criteria, may participate in said registry. The additional data from our patients can bolster the numbers in the clinical trial, which can contribute to the FDA approval process. One can see how this could accelerate the process of discovery and acceptance, as well as prove if the agent was not as good as it was made out to be. It goes both ways.
"We would love to be known as a place that facilitates the acceleration of ethical science and ethical therapies, and therefore brings global relief to those in need."
Do you think one day the Bahamas will be more well-known for its science than its beaches?
I doubt that. What I would like to say is that the Bahamas would love to always be known for its beautiful beaches, but we would also like to be known for diversity and innovation. Apart from all that beauty, we can still play a welcoming role to the rest of the scientific world. We would love to be known as a place that facilitates the acceleration of ethical science and ethical therapies, and therefore brings global relief to those in need.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Bivalent Boosters for Young Children Are Elusive. The Search Is On for Ways to Improve Access.
Theo, an 18-month-old in rural Nebraska, walks with his father in their backyard. For many toddlers, the barriers to accessing COVID-19 vaccines are many, such as few locations giving vaccines to very young children.
It’s Theo’s* first time in the snow. Wide-eyed, he totters outside holding his father’s hand. Sarah Holmes feels great joy in watching her 18-month-old son experience the world, “His genuine wonder and excitement gives me so much hope.”
In the summer of 2021, two months after Theo was born, Holmes, a behavioral health provider in Nebraska lost her grandparents to COVID-19. Both were vaccinated and thought they could unmask without any risk. “My grandfather was a veteran, and really trusted the government and faith leaders saying that COVID-19 wasn’t a threat anymore,” she says.” The state of emergency in Louisiana had ended and that was the message from the people they respected. “That is what killed them.”
The current official public health messaging is that regardless of what variant is circulating, the best way to be protected is to get vaccinated. These warnings no longer mention masking, or any of the other Swiss-cheese layers of mitigation that were prevalent in the early days of this ongoing pandemic.
The problem with the prevailing, vaccine centered strategy is that if you are a parent with children under five, barriers to access are real. In many cases, meaningful tools and changes that would address these obstacles are lacking, such as offering vaccines at more locations, mandating masks at these sites, and providing paid leave time to get the shots.
Children are at risk
Data presented at the most recent FDA advisory panel on COVID-19 vaccines showed that in the last year infants under six months had the third highest rate of hospitalization. “From the beginning, the message has been that kids don’t get COVID, and then the message was, well kids get COVID, but it’s not serious,” says Elias Kass, a pediatrician in Seattle. “Then they waited so long on the initial vaccines that by the time kids could get vaccinated, the majority of them had been infected.”
A closer look at the data from the CDC also reveals that from January 2022 to January 2023 children aged 6 to 23 months were more likely to be hospitalized than all other vaccine eligible pediatric age groups.
“We sort of forced an entire generation of kids to be infected with a novel virus and just don't give a shit, like nobody cares about kids,” Kass says. In some cases, COVID has wreaked havoc with the immune systems of very young children at his practice, making them vulnerable to other illnesses, he said. “And now we have kids that have had COVID two or three times, and we don’t know what is going to happen to them.”
Jumping through hurdles
Children under five were the last group to have an emergency use authorization (EUA) granted for the COVID-19 vaccine, a year and a half after adult vaccine approval. In June 2022, 30,000 sites were initially available for children across the country. Six months later, when boosters became available, there were only 5,000.
Currently, only 3.8% of children under two have completed a primary series, according to the CDC. An even more abysmal 0.2% under two have gotten a booster.
Ariadne Labs, a health center affiliated with Harvard, is trying to understand why these gaps exist. In conjunction with Boston Children’s Hospital, they have created a vaccine equity planner that maps the locations of vaccine deserts based on factors such as social vulnerability indexes and transportation access.
“People are having to travel farther because the sites are just few and far between,” says Benjy Renton, a research assistant at Ariadne.
Michelle Baltes-Breitwisch, a pharmacist, and her two-year-old daughter, Charlee, live in Iowa. When the boosters first came out she expected her toddler could get it close to home, but her husband had to drive Charlee four hours roundtrip.
This experience hasn’t been uncommon, especially in rural parts of the U.S. If parents wanted vaccines for their young children shortly after approval, they faced the prospect of loading babies and toddlers, famous for their calm demeanor, into cars for lengthy rides. The situation continues today. Mrs. Smith*, a grant writer and non-profit advisor who lives in Idaho, is still unable to get her child the bivalent booster because a two-hour one-way drive in winter weather isn’t possible.
It can be more difficult for low wage earners to take time off, which poses challenges especially in a number of rural counties across the country, where weekend hours for getting the shots may be limited.
Protect Their Future (PTF), a grassroots organization focusing on advocacy for the health care of children, hears from parents several times a week who are having trouble finding vaccines. The vaccine rollout “has been a total mess,” says Tamara Lea Spira, co-founder of PTF “It’s been very hard for people to access vaccines for children, particularly those under three.”
Seventeen states have passed laws that give pharmacists authority to vaccinate as young as six months. Under federal law, the minimum age in other states is three. Even in the states that allow vaccination of toddlers, each pharmacy chain varies. Some require prescriptions.
It takes time to make phone calls to confirm availability and book appointments online. “So it means that the parents who are getting their children vaccinated are those who are even more motivated and with the time and the resources to understand whether and how their kids can get vaccinated,” says Tiffany Green, an associate professor in population health sciences at the University of Wisconsin at Madison.
Green adds, “And then we have the contraction of vaccine availability in terms of sites…who is most likely to be affected? It's the usual suspects, children of color, disabled children, low-income children.”
It can be more difficult for low wage earners to take time off, which poses challenges especially in a number of rural counties across the country, where weekend hours for getting the shots may be limited. In Bibb County, Ala., vaccinations take place only on Wednesdays from 1:45 to 3:00 pm.
“People who are focused on putting food on the table or stressed about having enough money to pay rent aren't going to prioritize getting vaccinated that day,” says Julia Raifman, assistant professor of health law, policy and management at Boston University. She created the COVID-19 U.S. State Policy Database, which tracks state health and economic policies related to the pandemic.
Most states in the U.S. lack paid sick leave policies, and the average paid sick days with private employers is about one week. Green says, “I think COVID should have been a wake-up call that this is necessary.”
Maskless waiting rooms
For her son, Holmes spent hours making phone calls but could uncover no clear answers. No one could estimate an arrival date for the booster. “It disappoints me greatly that the process for locating COVID-19 vaccinations for young children requires so much legwork in terms of time and resources,” she says.
In January, she found a pharmacy 30 minutes away that could vaccinate Theo. With her son being too young to mask, she waited in the car with him as long as possible to avoid a busy, maskless waiting room.
Kids under two, such as Theo, are advised not to wear masks, which make it too hard for them to breathe. With masking policies a rarity these days, waiting rooms for vaccines present another barrier to access. Even in healthcare settings, current CDC guidance only requires masking during high transmission or when treating COVID positive patients directly.
“This is a group that is really left behind,” says Raifman. “They cannot wear masks themselves. They really depend on others around them wearing masks. There's not even one train car they can go on if their parents need to take public transportation… and not risk COVID transmission.”
Yet another challenge is presented for those who don’t speak English or Spanish. According to Translators without Borders, 65 million people in America speak a language other than English. Most state departments of health have a COVID-19 web page that redirects to the federal vaccines.gov in English, with an option to translate to Spanish only.
The main avenue for accessing information on vaccines relies on an internet connection, but 22 percent of rural Americans lack broadband access. “People who lack digital access, or don’t speak English…or know how to navigate or work with computers are unable to use that service and then don’t have access to the vaccines because they just don’t know how to get to them,” Jirmanus, an affiliate of the FXB Center for Health and Human Rights at Harvard and a member of The People’s CDC explains. She sees this issue frequently when working with immigrant communities in Massachusetts. “You really have to meet people where they’re at, and that means physically where they’re at.”
Equitable solutions
Grassroots and advocacy organizations like PTF have been filling a lot of the holes left by spotty federal policy. “In many ways this collective care has been as important as our gains to access the vaccine itself,” says Spira, the PTF co-founder.
PTF facilitates peer-to-peer networks of parents that offer support to each other. At least one parent in the group has crowdsourced information on locations that are providing vaccines for the very young and created a spreadsheet displaying vaccine locations. “It is incredible to me still that this vacuum of information and support exists, and it took a totally grassroots and volunteer effort of parents and physicians to try and respond to this need.” says Spira.
Kass, who is also affiliated with PTF, has been vaccinating any child who comes to his independent practice, regardless of whether they’re one of his patients or have insurance. “I think putting everything on retail pharmacies is not appropriate. By the time the kids' vaccines were released, all of our mass vaccination sites had been taken down.” A big way to help parents and pediatricians would be to allow mixing and matching. Any child who has had the full Pfizer series has had to forgo a bivalent booster.
“I think getting those first two or three doses into kids should still be a priority, and I don’t want to lose sight of all that,” states Renton, the researcher at Ariadne Labs. Through the vaccine equity planner, he has been trying to see if there are places where mobile clinics can go to improve access. Renton continues to work with local and state planners to aid in vaccine planning. “I think any way we can make that process a lot easier…will go a long way into building vaccine confidence and getting people vaccinated,” Renton says.

Michelle Baltes-Breitwisch, a pharmacist, and her two-year-old daughter, Charlee, live in Iowa. Her husband had to drive four hours roundtrip to get the boosters for Charlee.
Michelle Baltes-Breitwisch
Other changes need to come from the CDC. Even though the CDC “has this historic reputation and a mission of valuing equity and promoting health,” Jirmanus says, “they’re really failing. The emphasis on personal responsibility is leaving a lot of people behind.” She believes another avenue for more equitable access is creating legislation for upgraded ventilation in indoor public spaces.
Given the gaps in state policies, federal leadership matters, Raifman says. With the FDA leaning toward a yearly COVID vaccine, an equity lens from the CDC will be even more critical. “We can have data driven approaches to using evidence based policies like mask policies, when and where they're most important,” she says. Raifman wants to see a sustainable system of vaccine delivery across the country complemented with a surge preparedness plan.
With the public health emergency ending and vaccines going to the private market sometime in 2023, it seems unlikely that vaccine access is going to improve. Now more than ever, ”We need to be able to extend to people the choice of not being infected with COVID,” Jirmanus says.
*Some names were changed for privacy reasons.
Last month, a paper published in Cell by Harvard biologist David Sinclair explored root cause of aging, as well as examining whether this process can be controlled. We talked with Dr. Sinclair about this new research.
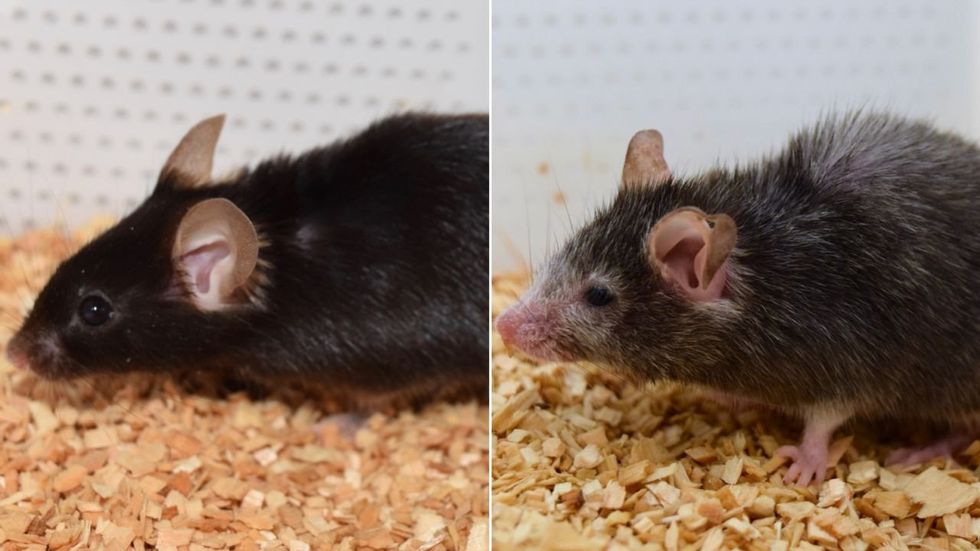
What causes aging? In a paper published last month, Dr. David Sinclair, Professor in the Department of Genetics at Harvard Medical School, reports that he and his co-authors have found the answer. Harnessing this knowledge, Dr. Sinclair was able to reverse this process, making mice younger, according to the study published in the journal Cell.
I talked with Dr. Sinclair about his new study for the latest episode of Making Sense of Science. Turning back the clock on mouse age through what’s called epigenetic reprogramming – and understanding why animals get older in the first place – are key steps toward finding therapies for healthier aging in humans. We also talked about questions that have been raised about the research.
Show links:
Dr. Sinclair's paper, published last month in Cell.
Recent pre-print paper - not yet peer reviewed - showing that mice treated with Yamanaka factors lived longer than the control group.
Dr. Sinclair's podcast.
Previous research on aging and DNA mutations.
Dr. Sinclair's book, Lifespan.

Harvard Medical School

