Short Story Contest Winner: "The Gerry Program"

A father and son gaze at the ducks in a lake.
It's an odd sensation knowing you're going to die, but it was a feeling Gerry Ferguson had become relatively acquainted with over the past two years. What most perplexed the terminally ill, he observed, was not the concept of death so much as the continuation of all other life.
Gerry's secret project had been in the works for two years now, ever since they found the growth.
Who will mourn me when I'm gone? What trait or idiosyncrasy will people most recall? Will I still be talked of, 100 years from now?
But Gerry didn't worry about these questions. He was comfortable that his legacy would live on, in one form or another. From his cozy flat in the west end of Glasgow, Gerry had managed to put his affairs in order and still find time for small joys.
Feeding the geese in summer at the park just down from his house, reading classics from the teeming bookcase in the living room, talking with his son Michael on Skype. It was Michael who had first suggested reading some of the new works of non-fiction that now littered the large oak desk in Gerry's study.
He was just finishing 'The Master Algorithm' when his shabby grandfather clock chimed six o'clock. Time to call Michael. Crammed into his tiny study, Gerry pulled his computer's webcam close and waved at Michael's smiling face.
"Hi Dad! How're you today?"
"I'm alright, son. How're things in sunny Australia?"
"Hot as always. How's things in Scotland?"
"I'd 'ave more chance gettin' a tan from this computer screen than I do goin' out there."
Michael chuckled. He's got that hearty Ferguson laugh, Gerry thought.
"How's the project coming along?" Michael asked. "Am I going to see it one of these days?"
"Of course," grinned Gerry, "I designed it for you."
Gerry's secret project had been in the works for two years now, ever since they found the growth. He had decided it was better not to tell Michael. He would only worry.
The two men chatted for hours. They discussed Michael's love life (or lack thereof), memories of days walking in the park, and their shared passion, the unending woes of Rangers Football Club. It wasn't until Michael said his goodbyes that Gerry noticed he'd been sitting in the dark for the best part of three hours, his mesh curtains casting a dim orange glow across the room from the street light outside. Time to get back to work.
*
Every night, Gerry sat at his computer, crawling forums, nourishing his project, feeding his knowledge and debating with other programmers. Even at age 82, Gerry knew more than most about algorithms. Never wanting to feel old, and with all the kids so adept at this digital stuff, Gerry figured he should give the Internet a try too. Besides, it kept his brain active and restored some of the sociability he'd lost in the previous decades as old friends passed away and the physical scope of his world contracted.
This night, like every night, Gerry worked away into the wee hours. His back would ache come morning, but this was the only time he truly felt alive these days. From his snug red brick home in Scotland, Gerry could share thoughts and information with strangers from all over the world. It truly was a miracle of modern science!
*
The next day, Gerry woke to the warm amber sun seeping in between a crack in the curtains. Like every morning, his thoughts took a little time to come into focus. Instinctively his hand went to the other side of the bed. Nobody there. Of course; she was gone. Rita, the sweetest woman he'd ever known. Four years this spring, God rest her soul.
Puttering around the cramped kitchen, Gerry heard a knock at the door. Who could that be? He could see two women standing in the hallway, their bodies contorted in the fisheye glass of the peephole. One looked familiar, but Gerry couldn't be sure. He fiddled with the locks and pulled the door open.
"Hi Gerry. How are you today?"
"Fine, thanks," he muttered, still searching his mind for where he'd seen her face before.
Noting the confusion in his eyes, the woman proffered a hand. "Alice, Alice Corgan. I pop round every now and again to check on you."
It clicked. "Ah aye! Come in, come in. Lemme get ya a cuppa." Gerry turned and shuffled into the flat.
As Gerry set about his tiny kitchen, Alice called from the living room, "This is Mandy. She's a care worker too. She's going to pay you occasional visits if that's alright with you."
Gerry poked his head around the doorway. "I'll always welcome a beautiful young lady in ma home. Though, I've tae warn you I'm a married man, so no funny business." He winked and ducked back into the kitchen.
Alice turned to Mandy with a grin. "He's a good man, our Gerry. You'll get along just fine." She lowered her voice. "As I said, with the Alzheimer's, he has to be reminded to take his medication, but he's still mostly self-sufficient. We installed a medi-bot to remind him every day and dispense the pills. If he doesn't respond, we'll get a message to send someone over."
Mandy nodded and scribbled notes in a pad.
"When I'm gone, Michael will have somethin' to remember me by."
"Also, and this is something we've been working on for a few months now, Gerry is convinced he has something…" her voice trailed off. "He thinks he has cancer. Now, while the Alzheimer's may affect his day-to-day life, it's not at a stage where he needs to be taken into care. The last time we went for a checkup, the doctor couldn't find any sign of cancer. I think it stems from--"
Gerry shouted from the other room: "Does the young lady take sugar?"
"No, I'm fine thanks," Mandy called back.
"Of course you don't," smiled Gerry. "Young lady like yersel' is sweet enough."
*
The following week, Mandy arrived early at Gerry's. He looked unsure at first, but he invited her in.
Sitting on the sofa nurturing a cup of tea, Alice tried to keep things light. "So what do you do in your spare time, Gerry?"
"I've got nothing but spare time these days, even if it's running a little low."
"Do you have any hobbies?"
"Yes actually." Gerry smiled. "I'm makin' a computer program."
Alice was taken aback. She knew very little about computers herself. "What's the program for?" she asked.
"Well, despite ma appearance, I'm no spring chicken. I know I don't have much time left. Ma son, he lives down in Australia now, he worked on a computer program that uses AI - that's artificial intelligence - to imitate a person."
Alice still looked confused, so Gerry pressed on.
"Well, I know I've not long left, so I've been usin' this open source code to make ma own for when I'm gone. I've already written all the code. Now I just have to add the things that make it seem like me. I can upload audio, text, even videos of masel'. That way, when I'm gone, Michael will have somethin' to remember me by."
Mandy sat there, stunned. She had no idea anybody could do this, much less an octogenarian from his small, ramshackle flat in Glasgow.
"That's amazing Gerry. I'd love to see the real thing when you're done."
"O' course. I mean, it'll take time. There's so much to add, but I'll be happy to give a demonstration."
Mandy sat there and cradled her mug. Imagine, she thought, being able to preserve yourself, or at least some basic caricature of yourself, forever.
*
As the weeks went on, Gerry slowly added new shades to his coded double. Mandy would leaf through the dusty photo albums on Gerry's bookcase, pointing to photos and asking for the story behind each one. Gerry couldn't always remember but, when he could, the accompanying stories were often hilarious, incredible, and usually a little of both. As he vividly recounted tales of bombing missions over Burma, trips to the beach with a young Michael and, in one particularly interesting story, giving the finger to Margaret Thatcher, Mandy would diligently record them through a Dictaphone to be uploaded to the program.
Gerry loved the company, particularly when he could regale the young woman with tales of his son Michael. One day, as they sat on the sofa flicking through a box of trinkets from his days as a travelling salesman, Mandy asked why he didn't have a smartphone.
He shrugged. "If I'm out 'n about then I want to see the world, not some 2D version of it. Besides, there's nothin' on there for me."
Alice explained that you could get Skype on a smartphone: "You'd be able to talk with Michael and feed the geese at the park at the same time," she offered.
Gerry seemed interested but didn't mention it again.
"Only thing I'm worried about with ma computer," he remarked, "is if there's another power cut and I can't call Michael. There's been a few this year from the snow 'n I hate not bein' able to reach him."
"Well, if you ever want to use the Skype app on my phone to call him you're welcome," said Mandy. "After all, you just need to add him to my contacts."
Gerry was flattered. "That's a relief, knowing I won't miss out on calling Michael if the computer goes bust."
*
Then, in early spring, just as the first green buds burst forth from the bare branches, Gerry asked Mandy to come by. "Bring that Alice girl if ya can - I know she's excited to see this too."
The next day, Mandy and Alice dutifully filed into the cramped study and sat down on rickety wooden chairs brought from the living room for this special occasion.
An image of Gerry, somewhat younger than the man himself, flashed up on the screen.
With a dramatic throat clearing, Gerry opened the program on his computer. An image of Gerry, somewhat younger than the man himself, flashed up on the screen.
The room was silent.
"Hiya Michael!" AI Gerry blurted. The real Gerry looked flustered and clicked around the screen. "I forgot to put the facial recognition on. Michael's just the go-to name when it doesn't recognize a face." His voice lilted with anxious excitement. "This is Alice," Gerry said proudly to the camera, pointing at Alice, "and this is Mandy."
AI Gerry didn't take his eyes from real Gerry, but grinned. "Hello, Alice. Hiya Mandy." The voice was definitely his, even if the flow of speech was slightly disjointed.
"Hi," Alice and Mandy stuttered.
Gerry beamed at both of them. His eyes flitted between the girls and the screen, perhaps nervous that his digital counterpart wasn't as polished as they'd been expecting.
"You can ask him almost anything. He's not as advanced as the ones they're making in the big studios, but I think Michael will like him."
Alice and Mandy gathered closer to the monitor. A mute Gerry grinned back from the screen. Sitting in his wooden chair, the real Gerry turned to his AI twin and began chattering away: "So, what do you think o' the place? Not bad eh?"
"Oh aye, like what you've done wi' it," said AI Gerry.
"Gerry," Alice cut in. "What did you say about Michael there?"
"Ah, I made this for him. After all, it's the kind o' thing his studio was doin'. I had to clear some space to upload it 'n show you guys, so I had to remove Skype for now, but Michael won't mind. Anyway, Mandy's gonna let me Skype him from her phone."
Mandy pulled her phone out and smiled. "Aye, he'll be able to chat with two Gerry's."
Alice grabbed Mandy by the arm: "What did you tell him?" she whispered, her eyes wide.
"I told him he can use my phone if he wants to Skype Michael. Is that okay?"
Alice turned to Gerry, who was chattering away with his computerized clone. "Gerry, we'll just be one second, I need to discuss something with Mandy."
"Righto," he nodded.
Outside the room, Alice paced up and down the narrow hallway.
Mandy could see how flustered she was. "What's wrong? Don't you like the chatbot? I think it's kinda c-"
"Michael's dead," Alice spluttered.
"What do you mean? He talks to him all the time."
Alice sighed. "He doesn't talk to Michael. See, a few years back, Michael found out he had cancer. He worked for this company that did AI chatbot stuff. When he knew he was dying he--" she groped in the air for the words-- "he built this chatbot thing for Gerry, some kind of super-advanced AI. Gerry had just been diagnosed with Alzheimer's and I guess Michael was worried Gerry would forget him. He designed the chatbot to say he was in Australia to explain why he couldn't visit."
"That's awful," Mandy granted, "but I don't get what the problem is. I mean, surely he can show the AI Michael his own chatbot?"
"No, because you can't get the AI Michael on Skype. Michael just designed the program to look like Skype."
"But then--" Mandy went silent.
"Michael uploaded the entire AI to Gerry's computer before his death. Gerry didn't delete Skype. He deleted the AI Michael."
"So… that's it? He-he's gone?" Mandy's voice cracked. "He can't just be gone, surely he can't?"
The women stood staring at each other. They looked to the door of the study. They could still hear Gerry, gabbing away with his cybercopy.
"I can't go back in there," muttered Mandy. Her voice wavered as she tried to stem the misery rising in her throat.
Alice shook her head and paced the floor. She stopped and stared at Mandy with grim resignation. "We don't have a choice."
When they returned, Gerry was still happily chatting away.
"Hiya girls. Ya wanna ask my handsome twin any other questions? If not, we could get Michael on the phone?"
Neither woman spoke. Gerry clapped his hands and turned gaily to the monitor again: "I cannae wait for ya t'meet him, Gerry. He's gonna be impressed wi' you."
Alice clasped her hands to her mouth. Tears welled in the women's eyes as they watched the old man converse with his digital copy. The heat of the room seemed to swell, becoming insufferable. Mandy couldn't take it anymore. She jumped up, bolted to the door and collapsed against a wall in the hallway. Alice perched on the edge of her seat in a dumb daze, praying for the floor to open and swallow the contents of the room whole.
Oblivious, Gerry and his echo babbled away, the blue glow of the screen illuminating his euphoric face. "Just wait until y'meet him Gerry, just wait."
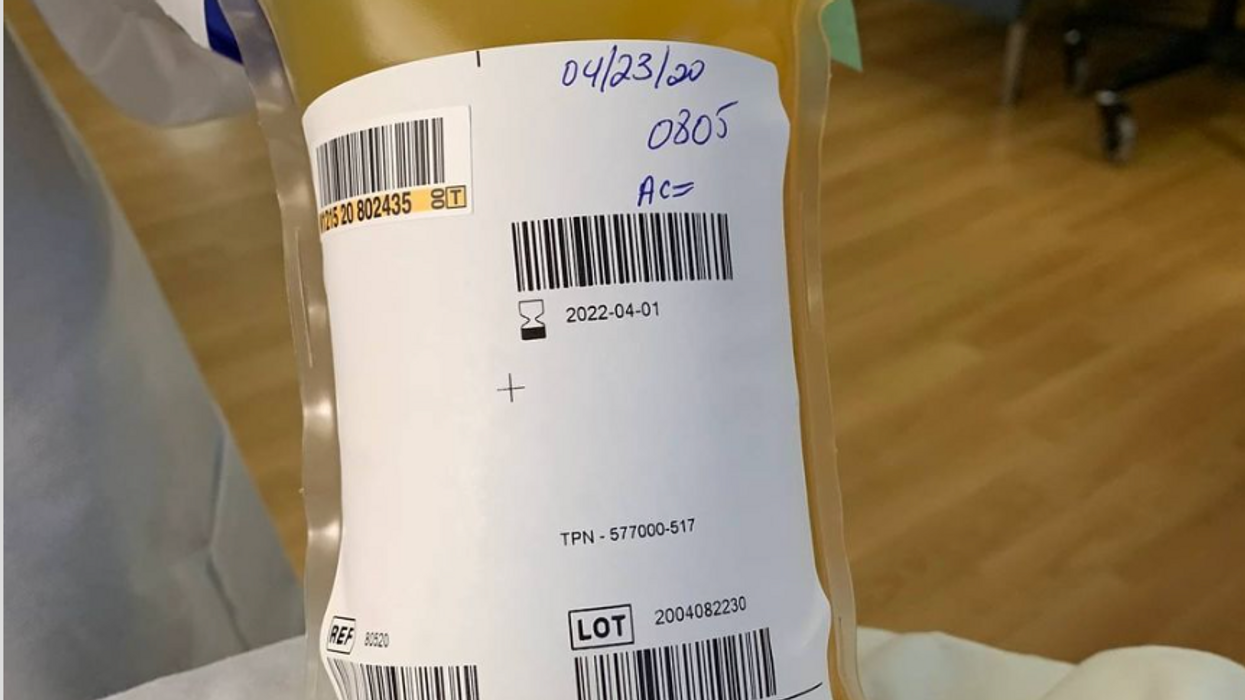
Blood Money: Paying for Convalescent Plasma to Treat COVID-19
A bag of plasma that Tom Hanks donated back in April 2020 after his coronavirus infection. (He was not paid to donate.)
Convalescent plasma – first used to treat diphtheria in 1890 – has been dusted off the shelf to treat COVID-19. Does it work? Should we rely strictly on the altruism of donors or should people be paid for it?
The biologic theory is that a person who has recovered from a disease has chemicals in their blood, most likely antibodies, that contributed to their recovery, and transferring those to a person who is sick might aid their recovery. Whole blood won't work because there are too few antibodies in a single unit of blood and the body can hold only so much of it.
Plasma comprises about 55 percent of whole blood and is what's left once you take out the red blood cells that carry oxygen and the white blood cells of the immune system. Most of it is water but the rest is a complex mix of fats, salts, signaling molecules and proteins produced by the immune system, including antibodies.
A process called apheresis circulates the donors' blood through a machine that separates out the desired parts of blood and returns the rest to the donor. It takes several times the length of a regular whole blood donation to cycle through enough blood for the process. The end product is a yellowish concentration called convalescent plasma.
Recent History
It was used extensively during the great influenza epidemic off 1918 but fell out of favor with the development of antibiotics. Still, whenever a new disease emerges – SARS, MERS, Ebola, even antibiotic-resistant bacteria – doctors turn to convalescent plasma, often as a stopgap until more effective antibiotic and antiviral drugs are developed. The process is certainly safe when standard procedures for handling blood products are followed, and historically it does seem to be beneficial in at least some patients if administered early enough in the disease.
With few good treatment options for COVID-19, doctors have given convalescent plasma to more than a hundred thousand Americans and tens of thousand of people elsewhere, to mixed results. Placebo-controlled trials could give a clearer picture of plasma's value but it is difficult to enroll patients facing possible death when the flip of a coin will determine who will receive a saline solution or plasma.
And the plasma itself isn't some uniform pill stamped out in a factory, it's a natural product that is shaped by the immune history of the donor's body and its encounter not just with SARS-CoV-2 but a lifetime of exposure to different pathogens.
Researchers believe antibodies in plasma are a key factor in directly fighting the virus. But the variety and quantity of antibodies vary from donor to donor, and even over time from the same donor because once the immune system has cleared the virus from the body, it stops putting out antibodies to fight the virus. Often the quality and quantity of antibodies being given to a patient are not measured, making it somewhat hit or miss, which is why several companies have recently developed monoclonal antibodies, a single type of antibody found in blood that is effective against SARS-CoV-2 and that is multiplied in the lab for use as therapy.
Plasma may also contain other unknown factors that contribute to fighting disease, say perhaps signaling molecules that affect gene expression, which might affect the movement of immune cells, their production of antiviral molecules, or the regulation of inflammation. The complexity and lack of standardization makes it difficult to evaluate what might be working or not with a convalescent plasma treatment. Thus researchers are left with few clues about how to make it more effective.
Industrializing Plasma
Many Americans living along the border with Mexico regularly head south to purchase prescription drugs at a significant discount. Less known is the medical traffic the other way, Mexicans who regularly head north to be paid for plasma donations, which are prohibited in their country; the U.S. allows payment for plasma donations but not whole blood. A typical payment is about $35 for a donation but the sudden demand for convalescent plasma from people who have recovered from COVID-19 commands a premium price, sometimes as high as $200. These donors are part of a fast-growing plasma industry that surpassed $25 billion in 2018. The U.S. supplies about three-quarters of the world's needs for plasma.
Payment for whole blood donation in the U.S. is prohibited, and while payment for plasma is allowed, there is a stigma attached to payment and much plasma is donated for free.
The pharmaceutical industry has shied away from natural products they cannot patent but they have identified simpler components from plasma, such as clotting factors and immunoglobulins, that have been turned into useful drugs from this raw material of plasma. While some companies have retooled to provide convalescent plasma to treat COVID-19, often paying those donors who have recovered a premium of several times the normal rate, most convalescent plasma has come as donations through traditional blood centers.
In April the Mayo Clinic, in cooperation with the FDA, created an expanded access program for convalescent plasma to treat COVID-19. It was meant to reduce the paperwork associated with gaining access to a treatment not yet approved by the FDA for that disease. Initially it was supposed to be for 5000 units but it quickly grew to more than twenty times that size. Michael Joyner, the head of the program, discussed that experience in an extended interview in September.
The Centers for Medicare and Medicaid Services (CMS) also created associated reimbursement codes, which became permanent in August.
Mayo published an analysis of the first 35,000 patients as a preprint in August. It concluded, "The relationships between mortality and both time to plasma transfusion, and antibody levels provide a signature that is consistent with efficacy for the use of convalescent plasma in the treatment of hospitalized COVID-19 patients."
It seemed to work best when given early in infection and in larger doses; a similar pattern has been seen in studies of monoclonal antibodies. A revised version will soon be published in a major medical journal. Some criticized the findings as not being from a randomized clinical trial.
Convalescent plasma is not the only intervention that seems to work better when used earlier in the course of disease. Recently the pharmaceutical company Eli Lilly stopped a clinical trial of a monoclonal antibody in hospitalized COVID-19 patients when it became apparent it wasn't helping. It is continuing trials for patients who are less sick and begin treatment earlier, as well as in persons who have been exposed to the virus but not yet diagnosed as infected, to see if it might prevent infection. In November the FDA eased access to this drug outside of clinical trials, though it is not yet approved for sale.
Show Me the Money
The antibodies that seem to give plasma its curative powers are fragile proteins that the body produces to fight the virus. Production shuts down once the virus is cleared and the remaining antibodies survive only for a few weeks before the levels fade. [Vaccines are used to train immune cells to produce antibodies and other defenses to respond to exposure to future pathogens.] So they can be usefully harvested from a recovered patient for only a few short weeks or months before they decline precipitously. The question becomes, how does one mobilize this resource in that short window of opportunity?
The program run by the Mayo Clinic explains the process and criteria for donating convalescent plasma for COVID-19, as well as links to local blood centers equipped to handle those free donations. Commercial plasma centers also are advertising and paying for donations.
A majority of countries prohibit paying donors for blood or blood products, including India. But an investigation by India Today touted a black market of people willing to donate convalescent plasma for the equivalent of several hundred dollars. Officials vowed to prosecute, saying donations should be selfless.
But that enforcement threat seemed to be undercut when the health minister of the state of Assam declared "plasma donors will get preference in several government schemes including the government job interview." It appeared to be a form of compensation that far surpassed simple cash.
The small city of Rexburg, Idaho, with a population a bit over 50,000, overwhelmingly Mormon and home to a campus of Brigham Young University, at one point had one of the highest per capita rates of COVID-19 in the current wave of infection. Rumors circulated that some students were intentionally trying to become infected so they could later sell their plasma for top dollar, potentially as much as $200 a visit.
Troubled university officials investigated the allegations but could come up with nothing definitive; how does one prove intentionality with such an omnipresent yet elusive virus? They chalked it up to idle chatter, perhaps an urban legend, which might be associated with alcohol use on some other campus.
Doctors, hospitals, and drug companies are all rightly praised for their altruism in the fight against COVID-19, but they also get paid. Payment for whole blood donation in the U.S. is prohibited, and while payment for plasma is allowed, there is a stigma attached to payment and much plasma is donated for free. "Why do we expect the donors [of convalescent plasma] to be the only uncompensated people in the process? It really makes no sense," argues Mark Yarborough, an ethicist at the UC Davis School of Medicine in Sacramento.
"When I was in grad school, two of my closest friends, at least once a week they went and gave plasma. That was their weekend spending money," Yarborough recalls. He says upper and middle-income people may have the luxury of donating blood products but prohibiting people from selling their plasma is a bit paternalistic and doesn't do anything to improve the economic status of poor people.
"Asking people to dedicate two hours a week for an entire year in exchange for cookies and milk is demonstrably asking too much," says Peter Jaworski, an ethicist who teaches at Georgetown University.
He notes that companies that pay plasma donors have much lower total costs than do operations that rely solely on uncompensated donations. The companies have to spend less to recruit and retain donors because they increase payments to encourage regular repeat donations. They are able to more rationally schedule visits to maximize use of expensive apheresis equipment and medical personnel used for the collection.
It seems that COVID-19 has been with us forever, but in reality it is less than a year. We have learned much over that short time, can now better manage the disease, and have lower mortality rates to prove it. Just how much convalescent plasma may have contributed to that remains an open question. Access to vaccines is months away for many people, and even then some people will continue to get sick. Given the lack of proven treatments, it makes sense to keep plasma as part of the mix, and not close the door to any legitimate means to obtain it.
Vaccines Without Vaccinations Won’t End the Pandemic
In this 2020 photograph, a bandage is placed on a patient who has just received a vaccine.
COVID-19 vaccine development has advanced at a record-setting pace, thanks to our nation's longstanding support for basic vaccine science coupled with massive public and private sector investments.
Yet, policymakers aren't according anywhere near the same level of priority to investments in the social, behavioral, and data science needed to better understand who and what influences vaccination decision-making. "If we want to be sure vaccines become vaccinations, this is exactly the kind of work that's urgently needed," says Dr. Bruce Gellin, President of Global Immunization at the Sabin Vaccine Institute.
Simply put: it's possible vaccines will remain in refrigerators and not be delivered to the arms of rolled-up sleeves if we don't quickly ramp up vaccine confidence research and broadly disseminate the findings.
According to the most recent Gallup poll, the share of U.S. adults who say they would get a COVID-19 vaccine rose to 58 percent this month from 50 percent in September, with non-white Americans and those ages 45-65 even less willing to be vaccinated. While there is still much we don't understand about COVID-19, we do know that without high levels of immunity in the population, a return to some semblance of normalcy is wishful thinking.
Research from prior vaccination campaigns such as H1N1, HPV, and the annual flu points us in the right direction. Key components of successful vaccination efforts require 1) Identifying the concerns of particular segments of the population; 2) Tailoring messages and incentives to address those concerns, and 3) Reaching out through trusted sources – health care providers, public health departments, and others in the community.
Research during the H1N1 flu found preparing people for some uncertainty actually improved trust, according to Dr. Sandra Crouse Quinn, professor and chair, Family Science, University of Maryland. Dr. Crouse Quinn's research during that period also underscored the need to address the specific vaccine concerns of racial and ethnic groups.
The stunning scientific achievement of COVID-19 vaccines anticipated to be ready in record time needs to be backed up by an equally ambitious and evidence-based effort to build the public's confidence in the vaccines.
Data science has provided crucial insight about the social media universe. Dr. Neil Johnson, a scientist at George Washington University, found that despite having fewer followers, anti-vaccination pages are more numerous and growing faster than pro-vaccination pages. They are more often linked to in discussions on other Facebook pages – such as school parent associations – where people are undecided about vaccination.
We've learned about building vaccine confidence from earlier campaigns. Now, however, we are faced with a unique and challenging set of obstacles to unpack quickly: How do we communicate the importance of eventual COVID-19 vaccines to Americans in light of the muddled-to-poor messaging from political leaders, the weaponizing of relatively simple public health recommendations, the enormous disproportionate toll on people of color, and the torrent of online misinformation? We urgently need data reflective of today's circumstances along with the policy to ensure it is quickly and effectively disseminated to the public health and clinical workforce.
Last year prompted in part by the measles outbreaks, Reps. Michael C. Burgess (R-TX) and Kim Shrier (D-WA), both physicians, introduced the bipartisan Vaccines Act to develop a national surveillance system to monitor vaccination rates and conduct a national campaign to increase awareness of the importance of vaccines. Unfortunately, that legislation wasn't passed. In response to COVID-19, Senate HELP Committee Ranking member Patty Murray (D-WA) has sought funds to strengthen vaccine confidence and combat misinformation with federally supported communication, research, and outreach efforts. Leading experts outside of Congress have called for this type of research, including the Sabin-Aspen Vaccine Science Policy Institute. Most recently, the National Academy of Sciences, in its report regarding the equitable distribution of the COVID-19 vaccine, included as one of its recommendations the need for "a rapid-response program to advance the science behind vaccine confidence."
Addressing trust in vaccination has never been as challenging nor as consequential. The stunning scientific achievement of COVID-19 vaccines anticipated to be ready in record time needs to be backed up by an equally ambitious and evidence-based effort to build the public's confidence in the vaccines. In its remaining days, the Trump Administration should invest in building vaccine confidence with current resources, targeting efforts to ensure COVID vaccines reduce rather than exacerbate racial and ethnic health disparities. Congress must also act to provide the additional research and outreach resources needed as well as pass the Vaccines Act so we are better prepared in the future.
If we don't succeed, COVID-19 will continue wreaking havoc on our health, our society, and our economy. We will also permanently jeopardize public trust in vaccines – one of the most successful medical interventions in human history.