Short-Term Suspended Animation for Humans Is Coming Soon

A man gasps for air through deep ice, in a symbolic representation of human hibernation through induced hypothermia.
At 1 a.m., Tony B. is flown to a shock trauma center of a university hospital. Five minutes earlier, he was picked up unconscious with no blood pressure, having suffered multiple gunshot wounds with severe blood loss. Standard measures alone would not have saved his life, but on the helicopter he was injected with ice-cold fluids intravenously to begin cooling him from the inside, and given special drugs to protect his heart and brain.
Suspended animation is not routine yet, but it's going through clinical trials at the University of Maryland and the University of Pittsburgh.
A surgeon accesses Tony's aorta, allowing his body to be flushed with larger amounts of cold fluids, thereby inducing profound hypothermia -- a body temperature below 10° C (50° F). This is suspended animation, a form of human hibernation, but officially the procedure is called Emergency Preservation and Resuscitation for Cardiac Arrest from Trauma (EPR-CAT).
This chilly state, which constitutes the preservation component of Tony's care, continues for an hour as surgeons repair injuries and connect his circulation to cardiopulmonary bypass (CPB). This allows blood to move through the brain delivering oxygen at low doses appropriate for the sharply reduced metabolic rate that comes with the hypothermia, without depending on the heart and lungs. CPB also enables controlled, gradual re-warming of Tony's body as fluid and appropriate amounts of red blood cells are transfused into him.
After another hour or so, Tony's body temperature reaches the range of 32-34° C (~90-93° F), called mild hypothermia. Having begun the fluid resuscitation process already, the team stops warming Tony, switches his circulation from CPB to his own heart and lungs, and begins cardiac resuscitation with electrical jolts to his heart. With his blood pressure stable, his heart rate slow but appropriate for the mild hypothermia, Tony is maintained at this intermediate temperature for 24 hours; this last step is already standard practice in treatment of people who suffer cardiac arrest without blood loss trauma.
The purpose is to prevent brain damage that might come with the rapid influx of too much oxygen, just as a feast would mean death to a starvation victim. After he is warmed to a normal temperature of 37° C (~99° F), Tony is awakened and ultimately recovers with no brain damage.
Tony's case is fictional; EPR-CAT is not routine yet, but it's going through clinical trials at the University of Maryland and the University of Pittsburgh, under the direction of trauma surgeon Dr. Samuel Tisherman, who spent many years developing the procedure in dogs and pigs. In such cases, patients undergo suspended animation for a couple of hours at most, but other treatments are showing promise in laboratory animals, like the use of hydrogen sulfide gas without active cooling to induce suspended animation in mice. Such interventions could ultimately fuse with EPR-CAT, sending the new technology further into what's still the realm of science fiction – at least for now.
Consider the scenario of a 5-year-old girl diagnosed with a progressive, incurable, terminal disease.
Experts say that extended suspended animation – cooling patients in a stable state for months or years -- could be possible at some point, although no one can predict when the technology will be clinical reality, since hydrogen sulfide and other chemical tactics would have to move into clinical use in humans and prove safe and effective in combination with EPR-CAT, or with a similar cooling approach.
How Could Long-Term Suspended Animation Impact Humanity?
Consider the scenario of a 5-year-old girl diagnosed with a progressive, incurable, terminal disease. Since available treatments would only lengthen the projected survival by a year, she is placed into suspended animation. She is revived partially every few years, as new treatments become available that can have a major impact on her disease. After 35 years of this, she is revived completely as treatments are finally adequate to cure her condition, but biologically she has aged only a few months. Physically, she is normal now, though her parents are in their seventies, and her siblings are grown and married.
Such hypothetical scenarios raise many issues: Where will the resources come from to take care of patients for that long? Who will pay? And how will patients adapt when they emerge into a completely different world?
"Heavy resource utilization is a factor if you've got people hibernating for years or decades," says Bradford Winters, an associate professor of anesthesiology and critical care medicine, and assistant professor of neurological surgery at Johns Hopkins.
Conceivably, special high-tech facilities with robots and artificial intelligence watching over the hibernators might solve the resource issue, but even then, Winters notes that long-term hibernation would entail major disparities between the wealthy and poor. "And then there is the psychological effect of being disconnected from one's family and society for a generation or more," he says. "What happens to that 5-year-old waking to her retired parents and married siblings? Will her younger sister adopt her? What would that be like?"
Probably better than dying is one answer.
Back on Earth, human hibernation would raise daunting policy questions that may take many years to resolve.
Outside of medicine, one application of human hibernation that has intrigued generations of science fiction writers is in long-duration space travel. During a voyage lasting years or decades, space explorers or colonists not only could avoid long periods of potential boredom, but also the aging process. Considering that the alternative to "sleeper ships" would be multi-generation starships so large that they'd be like small worlds, human hibernation in spaceflight could become an enabling technology for interstellar flight.
Big Questions: It's Not Too Early to Ask
Back on Earth, the daunting policy questions may take many years to resolve. Society ought to be aware of them now, before human hibernation technology outpaces its dramatic implications.
"Our current framework of ethical and legal regulation is adequate for cases like the gunshot victim who is chilled deeply for a few hours. Short-term cryopreservation is currently part of the continuum of care," notes David N. Hoffman, a clinical ethicist and health care attorney who teaches at Columbia University, and at Yeshiva University's Benjamin N. Cardozo School of Law and Albert Einstein College of Medicine.
"But we'll need a new framework when there's a capability to cryopreserve people for many years and still bring them back. There's also a legal-ethical issue involving the parties that decide to put the person into hibernation versus the patient wishes in terms of what risk benefit ratio they would accept, and who is responsible for the expense and burdens associated with cases that don't turn out just right?"
To begin thinking about practical solutions, Hoffman characterizes long-term human hibernation as an extension of the ethics of cyro-preserved embryos that are held for potential parents, often for long periods of time. But the human hibernation issue is much more complex.
"The ability of the custodian and patient to enter into a meaningful and beneficial arrangement is fraught, because medical advances necessary to address the person's illness or injury are -- by definition -- unknown," says Hoffman. "It means that you need a third party, a surrogate, to act on opportunities that the patient could never have contemplated."
Such multigenerational considerations might become more manageable, of course, in an era when gene therapy, bionic parts, and genetically engineered replacement organs enable dramatic life extension. But if people will be living for centuries regardless of whether or not they hibernate, then developing the medical technology may be the least of the challenges.
A robot server, controlled remotely by a disabled worker, delivers drinks to patrons at the DAWN cafe in Tokyo.
A sleek, four-foot tall white robot glides across a cafe storefront in Tokyo’s Nihonbashi district, holding a two-tiered serving tray full of tea sandwiches and pastries. The cafe’s patrons smile and say thanks as they take the tray—but it’s not the robot they’re thanking. Instead, the patrons are talking to the person controlling the robot—a restaurant employee who operates the avatar from the comfort of their home.
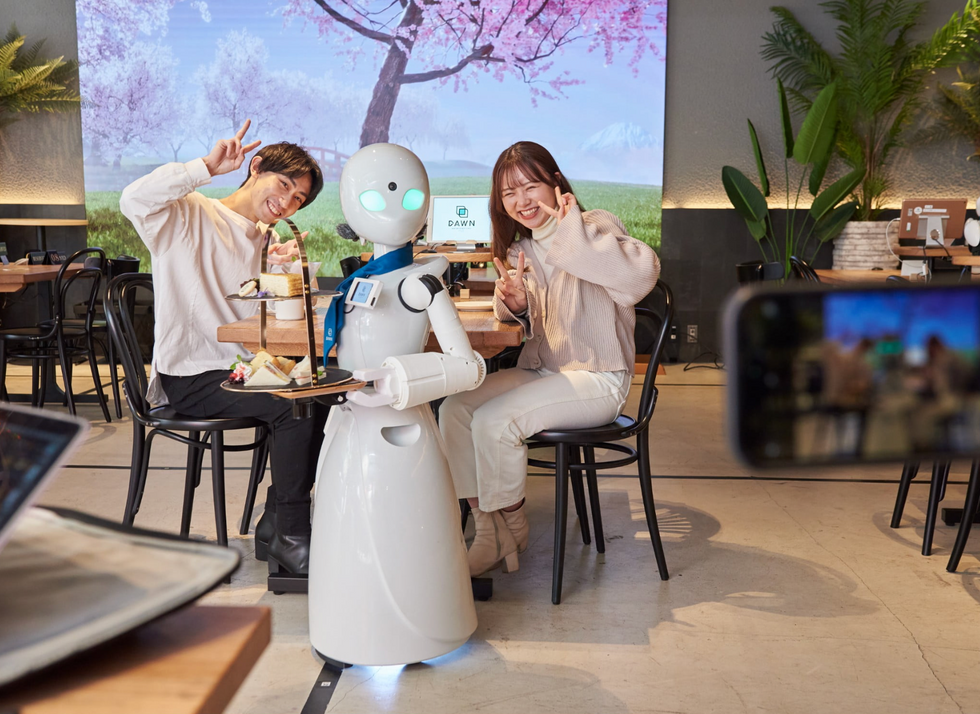
It’s a typical scene at DAWN, short for Diverse Avatar Working Network—a cafe that launched in Tokyo six years ago as an experimental pop-up and quickly became an overnight success. Today, the cafe is a permanent fixture in Nihonbashi, staffing roughly 60 remote workers who control the robots remotely and communicate to customers via a built-in microphone.
More than just a creative idea, however, DAWN is being hailed as a life-changing opportunity. The workers who control the robots remotely (known as “pilots”) all have disabilities that limit their ability to move around freely and travel outside their homes. Worldwide, an estimated 16 percent of the global population lives with a significant disability—and according to the World Health Organization, these disabilities give rise to other problems, such as exclusion from education, unemployment, and poverty.
These are all problems that Kentaro Yoshifuji, founder and CEO of Ory Laboratory, which supplies the robot servers at DAWN, is looking to correct. Yoshifuji, who was bedridden for several years in high school due to an undisclosed health problem, launched the company to help enable people who are house-bound or bedridden to more fully participate in society, as well as end the loneliness, isolation, and feelings of worthlessness that can sometimes go hand-in-hand with being disabled.
“It’s heartbreaking to think that [people with disabilities] feel they are a burden to society, or that they fear their families suffer by caring for them,” said Yoshifuji in an interview in 2020. “We are dedicating ourselves to providing workable, technology-based solutions. That is our purpose.”

Shota, Kuwahara, a DAWN employee with muscular dystrophy, agrees. "There are many difficulties in my daily life, but I believe my life has a purpose and is not being wasted," he says. "Being useful, able to help other people, even feeling needed by others, is so motivational."
A woman receives a mammogram, which can detect the presence of tumors in a patient's breast.
When a patient is diagnosed with early-stage breast cancer, having surgery to remove the tumor is considered the standard of care. But what happens when a patient can’t have surgery?
Whether it’s due to high blood pressure, advanced age, heart issues, or other reasons, some breast cancer patients don’t qualify for a lumpectomy—one of the most common treatment options for early-stage breast cancer. A lumpectomy surgically removes the tumor while keeping the patient’s breast intact, while a mastectomy removes the entire breast and nearby lymph nodes.
Fortunately, a new technique called cryoablation is now available for breast cancer patients who either aren’t candidates for surgery or don’t feel comfortable undergoing a surgical procedure. With cryoablation, doctors use an ultrasound or CT scan to locate any tumors inside the patient’s breast. They then insert small, needle-like probes into the patient's breast which create an “ice ball” that surrounds the tumor and kills the cancer cells.
Cryoablation has been used for decades to treat cancers of the kidneys and liver—but only in the past few years have doctors been able to use the procedure to treat breast cancer patients. And while clinical trials have shown that cryoablation works for tumors smaller than 1.5 centimeters, a recent clinical trial at Memorial Sloan Kettering Cancer Center in New York has shown that it can work for larger tumors, too.
In this study, doctors performed cryoablation on patients whose tumors were, on average, 2.5 centimeters. The cryoablation procedure lasted for about 30 minutes, and patients were able to go home on the same day following treatment. Doctors then followed up with the patients after 16 months. In the follow-up, doctors found the recurrence rate for tumors after using cryoablation was only 10 percent.
For patients who don’t qualify for surgery, radiation and hormonal therapy is typically used to treat tumors. However, said Yolanda Brice, M.D., an interventional radiologist at Memorial Sloan Kettering Cancer Center, “when treated with only radiation and hormonal therapy, the tumors will eventually return.” Cryotherapy, Brice said, could be a more effective way to treat cancer for patients who can’t have surgery.
“The fact that we only saw a 10 percent recurrence rate in our study is incredibly promising,” she said.

